Published online Jan 16, 2026. doi: 10.12998/wjcc.v14.i2.114671
Revised: November 1, 2025
Accepted: December 25, 2025
Published online: January 16, 2026
Processing time: 112 Days and 14.1 Hours
Although hepatic adenomas (HA) account for less than 0.04% of all liver neo
We report the case of a previously healthy 30-year-old female patient, a regular user of combined oral contraceptives, who presented with acute hemorrhagic abdomen due to spontaneous rupture of a HA. The clinical presentation occurred after physical exertion and was with evidence of intra-abdominal bleeding. Initial management included selective hepatic arterial embolization as a conservative approach. Due to ongoing hemorrhage, an urgent left partial hepatectomy was indicated.
The operation was completed without adverse events, and postoperative recovery was favorable. This report emphasizes the significance of prompt diagnosis and immediate surgical intervention when hemodynamic compromise occurs due to HA rupture.
Core Tip: Hepatic adenomas (HA) are rare benign liver neoplasms. Clinically, they are usually asymptomatic. We report a case of intra-abdominal hemorrhage due to spontaneous rupture, configuring a hemorrhagic acute abdomen with imminent risk to life. Combined with the analysis of cases indexed in PubMed, spontaneous rupture of a HA represents a rare and serious medical emergency, responsible for approximately 20%-30% of complications from these tumors. Early detection of suspicious lesions is a favorable factor for patient survival. After the discovery of HA, providing appropriate active treatment has positive effects on the prognosis of patients. The treatment plan should be based on the patient’s response to conservative measures and hepatic arterial embolization up to emergency hepatectomy, depending on the extent of the lesion and hemodynamic stability.
- Citation: Pagani Junior MA, Siman Lopes L, Sergi Filho FA, Goes Scorsioni FA, Tavares Filho MB, Maluf Amaral RP, Medeiros LE, Guillen Carneiro LI, Belluzzo HG, Vinholo TR, Buchaim DV, Buchaim RL. Partial left hepatectomy in a young patient with ruptured hepatic adenoma: A case report. World J Clin Cases 2026; 14(2): 114671
- URL: https://www.wjgnet.com/2307-8960/full/v14/i2/114671.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v14.i2.114671
Hepatic adenomas (HA) are frequently associated with the use of oral contraceptives in women of childbearing age[1], although they can also affect men, there are others risk factors such as: Metabolic syndromes with diabetes, obesity, glycogen storage diseases, and fatty liver disease[2].
Despite the known association between oral contraceptives and HA, this condition is rare in the general population. The estimated prevalence of HA is approximately 3 per 100000 women using oral contraceptives per year, with a high prevalence between the ages of 20 and 40[1]. This makes the occurrence of spontaneous hemorrhagic rupture in young patients even more uncommon, although clinically relevant, with a significant impact on emergency management.
This risk is higher in lesions larger than 5 cm or with specific histological characteristics[3]. Several recent reports indicate hepatectomy as an effective alternative for definitive hemorrhage control, especially when embolization fails or is not feasible. Computed tomography plays an essential role in early diagnosis, allowing the identification of signs of rupture and active bleeding[4-6].
A 30-year-old Brazilian woman presented on initial physical examination, a palpable and painful abdominal mass was found in the epigastrium extending laterally into the right hypochondrium for 12 hours after intense physical activity.
The patient reported a two-day history of recurrent abdominal pain before presentation.
The patient sought care at a local hospital after experiencing abdominal pain for two days. Computed tomography (CT) imaging of the abdomen revealed a heterogeneous, expansile mass with blood content, centered on the lateral segments of the left hepatic lobe; as a radiological change on admission from abdominal CT and evidence of contrast extravasation in the arterial phase at the level of the left hepatic artery in segment VIII. Our endovascular therapy procedure with embolization was performed using absolute ethanol material (98%), one of the most used sclerosing agents for em
The lesion had irregular contours, discontinuity of the upper border, and perilesional hematic fluid, consistent with tumor rupture and active bleeding. The patient was admitted to the intensive care unit for clinical monitoring, empirical antibiotic therapy, and serial laboratory monitoring of hemoglobin and hematocrit levels every six hours. During arteriography, contrast extravasation was observed in the hepatic nodular mass (segment 8), demonstrating active bleeding and the need for embolization intervention. Selective embolization of the left hepatic artery was performed, which was technically successful, with the control of bleeding after embolization of the target vessel. Given the failure to definitively control the bleeding and the strong suspicion of a ruptured hepatic adenoma, a multidisciplinary discussion involving the hepatobiliary surgery and interventional radiology teams was conducted, which indicated a left partial hepatectomy.
Patient with Hashimoto’s thyroiditis regularly in use of levothyroxine and combined oral contraceptives.
Physical examination revealed the following vital signs: Body temperature of 36.5 °C, blood pressure of 117/68 mmHg, heart rate of 82 beats per minute, and respiratory rate of 19 breaths per minute. A painful abdominal mass approximately 7 cm in diameter was detected in the right abdominal and epigastric areas.
Hemoglobin levels were decreased, while other blood and urine analyses revealed no abnormalities.
Initial abdominal ultrasound revealed two hepatic nodules in segment II. On August 3, 2024, a non-contrast abdominal CT scan was performed, which showed a heterogeneous expansile mass with hematic content, centered in the lateral segments of the left hepatic lobe. Initially, the patient was admitted with a non-contrast CT scan, without enhancement of the heterogeneous mass, followed by referral to our medical service, followed by a new tomography scan by the Hospital, this last examination with contrast identification and in the arterial phase a rapid and intense enhancement (hy
After the tomography on August 4, in the portal phase, the actual size tended to decrease, with the lesion being more isodense or slightly hypodense compared to the adjacent liver, however at the arterial phase the image demonstrated persistent vascularization in the expansive lesion, measuring approximately 8.7 cm in length, associated with an adjacent blood collection of approximately 65 cm3 in volume. Embolic material was observed in the arterial branches of the hepatic hilum, in addition to an anatomical variant with the left hepatic artery originating from the left gastric artery. A small bilateral pleural effusion and underlying atelectasis were also identified, with no evidence of active contrast extravasation into the peritoneal cavity.
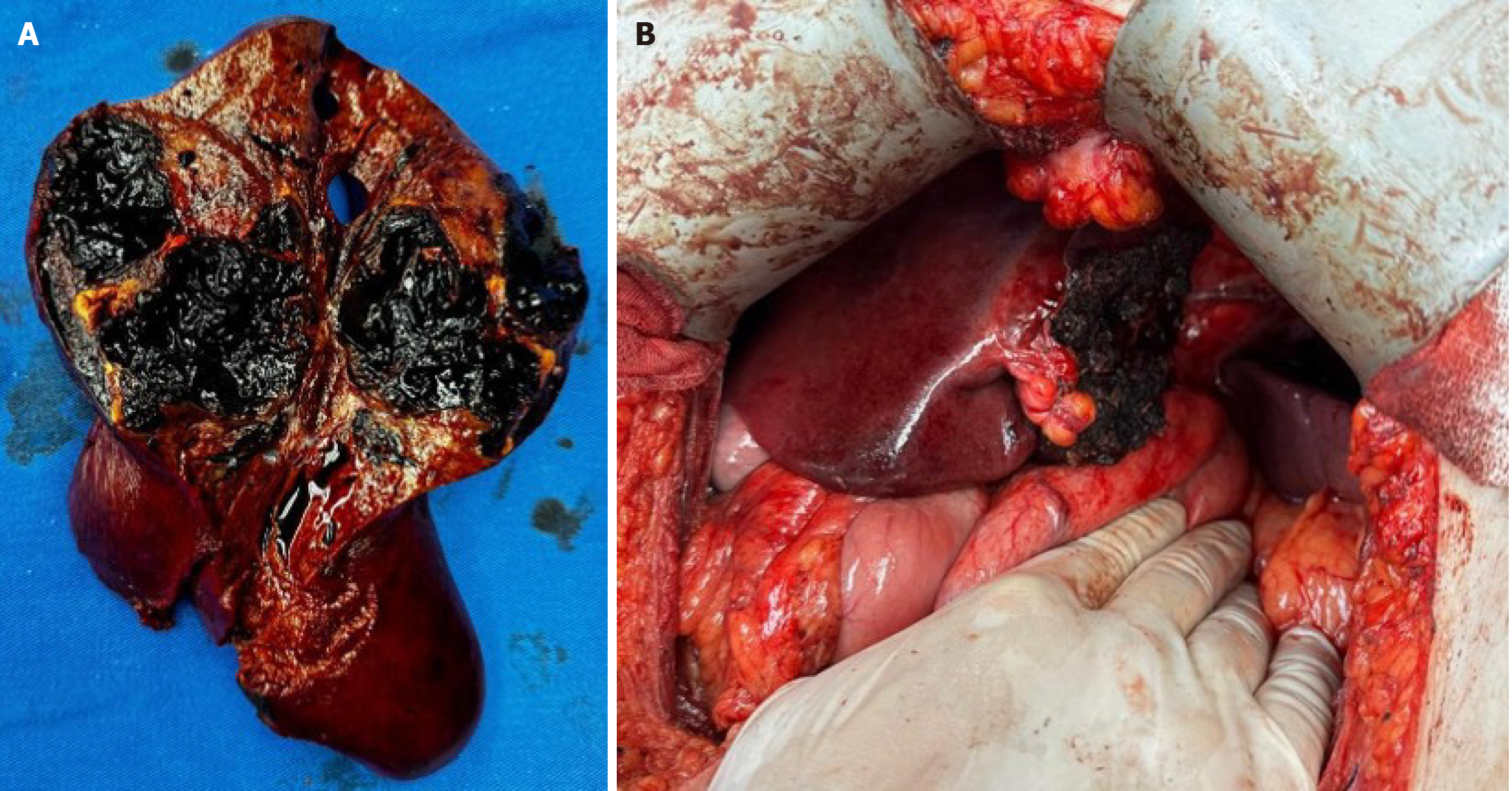
Combined with the patient’s clinical and imaging data, this shows a case of non-traumatic ruptured hepatic adenoma (Figure 1).
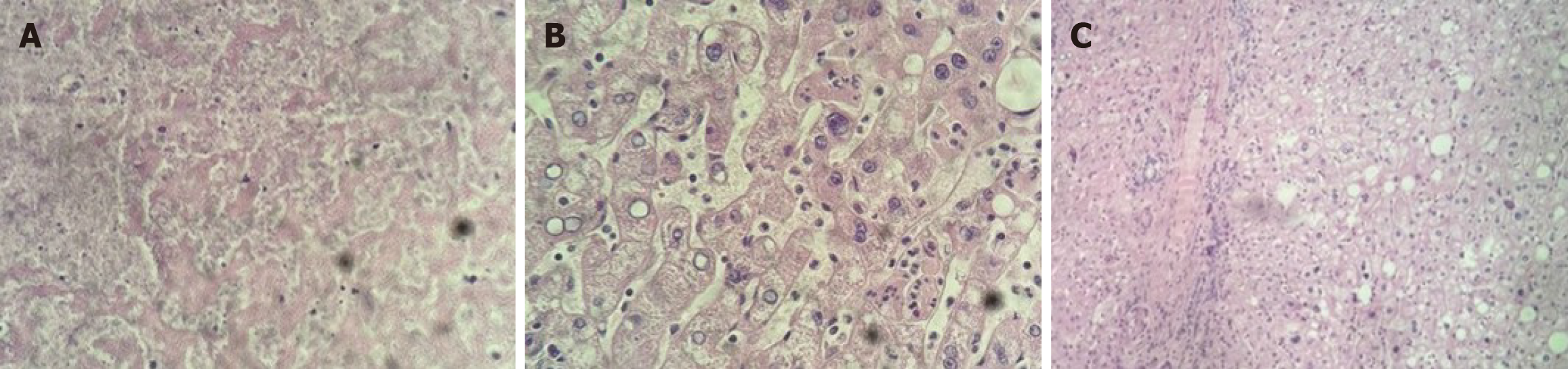
Ellinger Anatomical Pathology Laboratory in Marília, São Paulo, Brazil. Well-differentiated hepatocellular neoplasm, with circumscribed borders, hepatocytes with ample cytoplasm, focal macrovesicular steatosis (approximately 5%), without atypia, sparse ducts and unpaired arterioles, extensive hemorrhages, in a subcapsular location, measuring 10.5 cm. Diagnosis: Hepatocellular adenoma (Figure 2).
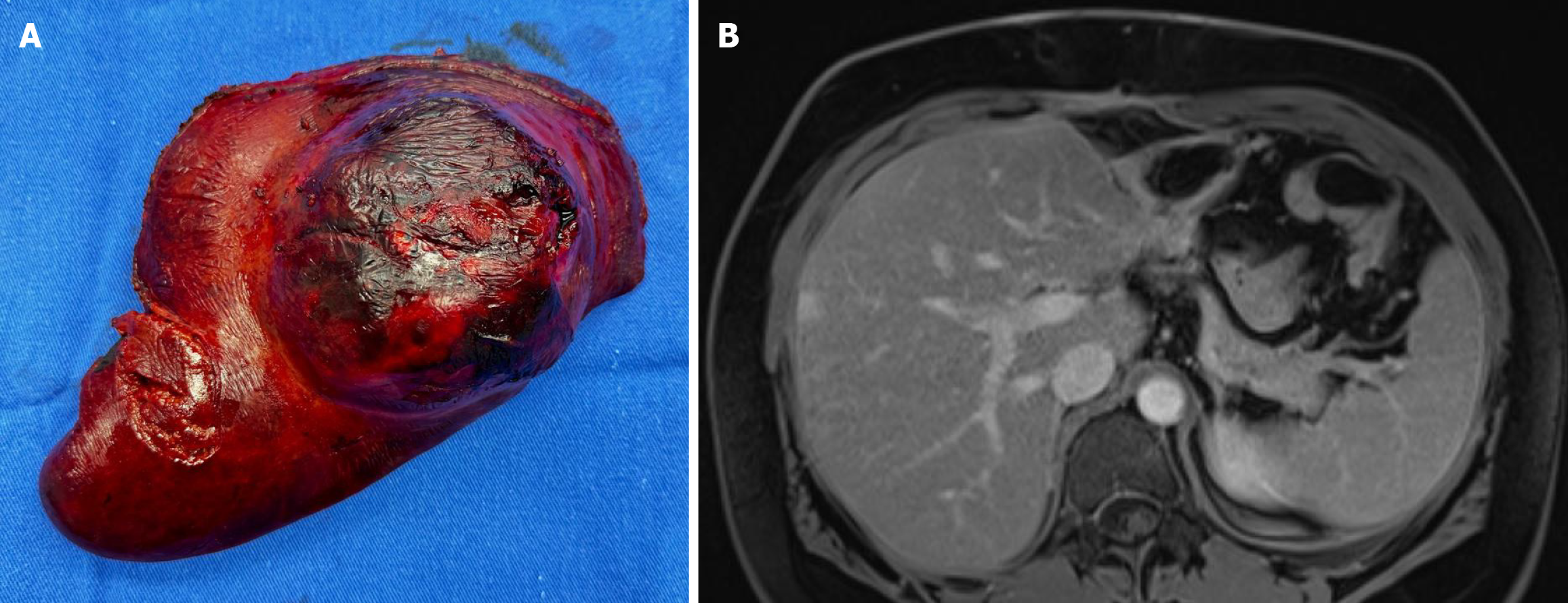
Following an uncomplicated recovery, the patient was discharged on the fifth postoperative day. Subsequent follow-up at two weeks involved clinical assessment and magnetic resonance imaging of the upper abdomen (Figure 3).
At 2 months postoperatively, the patient was released for physical and work activities.
Hemorrhagic rupture of HA is a rare but potentially fatal medical emergency that requires early diagnosis and appropriate intervention. The use of oral contraceptives is the risk factor most strongly associated with the development of adenomas, increasing both the incidence and the possibility of serious complications, such as spontaneous rupture and massive bleeding[1].
Selective arterial embolization is considered a valid initial approach in stable patients, as it can temporarily control bleeding and allow clinical stabilization[2-4]. However, procedure failure, as occurred in this case, reinforces the central role of surgery as definitive treatment[5]. Studies show that emergency hepatectomy, although challenging, can provide effective bleeding control and complete histopathological analysis, which is essential to rule out malignant transformation[6,7].
Recent reports highlight that bulky lesions, larger than 5 cm, are more prone to spontaneous rupture and massive intraperitoneal hemorrhage, supporting the indication for early surgery in these scenarios[8]. Situations which the rupture occurred after prior abdominal trauma, highlight that the presence of underlying liver lesions can complicate conditions initially attributed solely to trauma and reinforce the need for surgical management in cases of bulky or hemorrhagic tumors[9,10].
Another relevant aspect concerns diagnostic difficulties. A hepatic adenoma that mimicked metastasis on PET-CT, demonstrating that imaging methods cannot always accurately distinguish benign from malignant lesions[11]. This finding reinforces the importance of histopathological examination after resection, ensuring a definitive diagnosis and better risk stratification. Even rarer are cases that progress to severe liver failure. The first report of a two-stage liver transplant for a ruptured hepatic adenoma complicated by toxic liver syndrome after multiple embolization failures[12]. This case illustrates that, in extreme scenarios, resection alone may be insufficient, and transplantation should be considered as salvage therapy[13].
Furthermore, the literature emphasizes that multidisciplinary management is crucial to reducing complications. Some guidelines between hepatobiliary surgeons, interventional radiologists, and intensivists results in better postoperative outcomes. In the case presented, the joint decision-making between surgery and interventional radiology was crucial to therapeutic success[14].
Therefore, this case contributes to the literature by reinforcing that, although arterial embolization is the first-line treatment in selected situations, surgical resection remains essential in the event of conservative treatment, ensuring both definitive resolution of the hemorrhage and histopathological diagnosis of the adenoma[15].
Left partial hepatectomy was effective in treating a ruptured hepatic adenoma after conservative management failed. This case contributes to understanding the management of emergencies associated with benign liver lesions, emphasizing the importance of surgical intervention in situations where conservative options, such as embolization, fail. It also reinforces the need for individualized patient assessment and multidisciplinary management.
| 1. | Myers L, Ahn J. Focal Nodular Hyperplasia and Hepatic Adenoma: Evaluation and Management. Clin Liver Dis. 2020;24:389-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Nahm CB, Parker N, Gundara JS, Gill AJ, Bhimani N, Samra JS, Hugh TJ. Management of patients with hepatocellular adenoma: a single-institution experience. ANZ J Surg. 2020;90:786-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Mironova M, Mahdi MK, Bhatia J, Nielson RC, Doria C. From an Incidental Finding to an Emergent Treatment: A Case Report of a Hepatic Adenomatosis and Large Ruptured Hepatic Adenoma. Case Rep Gastrointest Med. 2021;2021:9963440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Kis LE, Centeno BA, Anaya DA, Kis B. Hepatic adenoma rupture following portal vein embolization. Radiol Case Rep. 2020;15:664-667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Herman P, Fonseca GM, Kruger JAP, Jeismann VB, Coelho FF. Guidelines for the Treatment of Hepatocellular Adenoma in the Era of Molecular Biology: An Experience-Based Surgeons' Perspective. J Gastrointest Surg. 2021;25:1494-1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Lanza D, Bilali M. Hepatic Adenomatosis in a Young Asymptomatic but High-risk Patient: An Incidental Diagnosis with Potentially Severe Clinical Implications. Eur J Case Rep Intern Med. 2021;8:002999. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Çakır Ç. Non-traumatic spontaneous ruptured hepatocellular adenoma after selective transcatheter arterial chemo-embolization for reduction of tumor mass: A case report. Ulus Travma Acil Cerrahi Derg. 2022;28:225-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Yoon PD, Chen AZL, Tovmassian D, Pleass H. Spontaneous hepatic haemorrhage secondary to ruptured hepatocellular adenoma in a young male patient. BMJ Case Rep. 2020;13:e235966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Sanford B, Hoeppner C, Ju T, Theisen BK, BuAbbud A, Estroff JM. Multidisciplinary management of the pregnant patient in haemorrhagic shock secondary to an undiagnosed ruptured liver adenoma. BMJ Case Rep. 2020;13:e231995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Kountouri I, Kokkali E, Giotas A, Katsarelas I, Dimasis P. A Rare Case of a Spontaneously Ruptured Hepatocellular Adenoma in the Third Trimester of Pregnancy. Cureus. 2024;16:e72447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Lim D, Lee SY, Lim KH, Chan CY. Hepatic adenoma mimicking a metastatic lesion on computed tomography-positron emission tomography scan. World J Gastroenterol. 2013;19:4432-4436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Salhanick M, MacConmara MP, Pedersen MR, Grant L, Hwang CS, Parekh JR. Two-stage liver transplant for ruptured hepatic adenoma: A case report. World J Hepatol. 2019;11:242-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Cotta-Pereira RL, Valente LF, De Paula DG, Eiras-Araújo AL, Iglesias AC. Rupture of a hepatic adenoma in a young woman after an abdominal trauma: a case report. World J Gastroenterol. 2013;19:4422-4426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Silva TS, Sung M, Nelson DW, DiFronzo AL, O'Connor VV. A Multicenter, 10-Year Experience With Hepatocellular Adenoma: Risk Factors and Disease Course. Am Surg. 2022;88:2345-2350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Lord J, Britton H, Spain SG, Lewis AL. Advancements in the development on new liquid embolic agents for use in therapeutic embolisation. J Mater Chem B. 2020;8:8207-8218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/