Published online Jan 16, 2026. doi: 10.12998/wjcc.v14.i2.110627
Revised: July 21, 2025
Accepted: December 22, 2025
Published online: January 16, 2026
Processing time: 219 Days and 16.7 Hours
Oral cavity cancers are highly invasive malignancies, typically treated with a com
The case involves a 70-year-old woman who underwent a right segmental man
This case highlights how a multidisciplinary, comprehensive, personalized, and biopsychosocial approach can optimize outcomes in complex oral rehabilitation following oncological surgery.
Core Tip: This case highlights the full oral rehabilitation of a patient who underwent segmental mandibulectomy with fibula free flap reconstruction for advanced oral squamous cell carcinoma. A multidisciplinary approach was employed to address trismus, masticatory dysfunction, and aesthetic deficits, combining custom-made dentures, fluoride trays, and hyaluronic acid injections. Hyaluronic acid contributed to improving facial symmetry and reducing scarring, enhancing the patient’s quality of life. This case underscores the importance of innovative, patient-centered dental interventions in managing complex post-surgical complications and demonstrates a practical, reproducible approach applicable to similar clinical scenarios.
- Citation: Hessloehl N, Collart-Dutilleul PY, Romieu O, Carayon D. Functional and aesthetic oral rehabilitation after cancer treatment using dental prosthesis and hyaluronic acid injections: A case report and review of literature. World J Clin Cases 2026; 14(2): 110627
- URL: https://www.wjgnet.com/2307-8960/full/v14/i2/110627.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v14.i2.110627
Oral squamous cell carcinoma (OSCC) is a prevalent malignancy characterized by aggressive local invasion and sig
In this case report, we present a multidisciplinary rehabilitation approach following surgical reconstruction, combining removable dentures with hyaluronic acid (HA) injections to address both functional deficits and aesthetic concerns of a patient treated for OSCC. We emphasize the efficacy of this integrated treatment strategy in enhancing oral function and facial aesthetics following OSCC treatment. HA injections in facial reconstruction can augment soft tissue volume and improve cosmetic outcomes[12,14]. HA is a high-molecular-weight polysaccharide formed by the polymerization of glucuronic acid alternating with N-acetylglucosamine. It is a naturally occurring glycosaminoglycan found in the extracellular matrix of the skin, where it plays a key role in regulating cell proliferation, migration, and differentiation. It also contributes significantly to skin hydration, elasticity, and smoothness[15]. When used as an injectable, HA functions as a biocompatible dermal filler with hydrating and volumizing properties. It has garnered interest for its potential in managing radiation-induced fibrosis and in restoring facial symmetry in cancer survivors[16-18]. Clinical use of HA has been shown to improve scar elasticity, enhance facial aesthetics, and reduce the visible effects of soft tissue deficits[19-21].
To our knowledge, no prior case reports have integrated intraoral prosthetic rehabilitation with targeted perioral HA injections for aesthetic correction in post-OSCC patients. While prosthetic rehabilitation and HA fillers have each been described separately in oncology contexts[12,22], the combined use of both interventions to address commissural asymmetry and functional rehabilitation in a single multidisciplinary protocol remains undocumented. This case, therefore, offers preliminary feasibility data for a reproducible approach that integrates oral function restoration with aesthetic soft-tissue correction in the complex setting of post-oncologic reconstruction. This case report aims to explore the benefits of combining HA injections with removable partial prosthetic rehabilitation in a patient presenting with severe functional and aesthetic deficits following extensive oral cancer treatment. This approach underscores the importance of addressing not only oral function but also the psychological and social well-being of patients recovering from oncological surgery.
A 70-year-old female patient presented to the Odontology Department of Montpellier University Hospital with complaints of impaired oral function and noticeable facial asymmetry following treatment for OSCC. She reported limited mouth opening, difficulty with mastication, and aesthetic concerns, including collapse of the right cheek and lower lip.
The patient’s symptoms began three years prior, initially manifesting as recurrent infections at a tooth extraction site in the right retromolar region. A biopsy with bone sampling confirmed squamous cell carcinoma. She was referred to the ear, nose, and throat department, where a diagnosis of OSCC of the right retromolar trigone was established. Tumor invasion of the mandible necessitated a right segmental mandibulectomy, fibula free flap reconstruction, and bilateral cervical lymphadenectomy. Histopathological analysis classified the disease as pT4aN2b, according to the American Joint Committee on Cancer staging system[23], with invasion of the tongue’s extrinsic muscles and the mandible, along with metastases in multiple ipsilateral lymph nodes. The patient subsequently underwent adjuvant chemoradiotherapy with cisplatin and carboplatin-cetuximab, receiving 66 grays of radiation to the tumor site. During recovery, she developed significant trismus, severe soft tissue atrophy, and psychological distress.
Her medical history included hypothyroidism, managed with levothyroxine, and a prior cholecystectomy. She had no history of tobacco or alcohol use and reported no known drug allergies. She tolerated oncologic treatment well, com
The patient reported no significant personal habits detrimental to oral or general health. She used a soft-bristled too
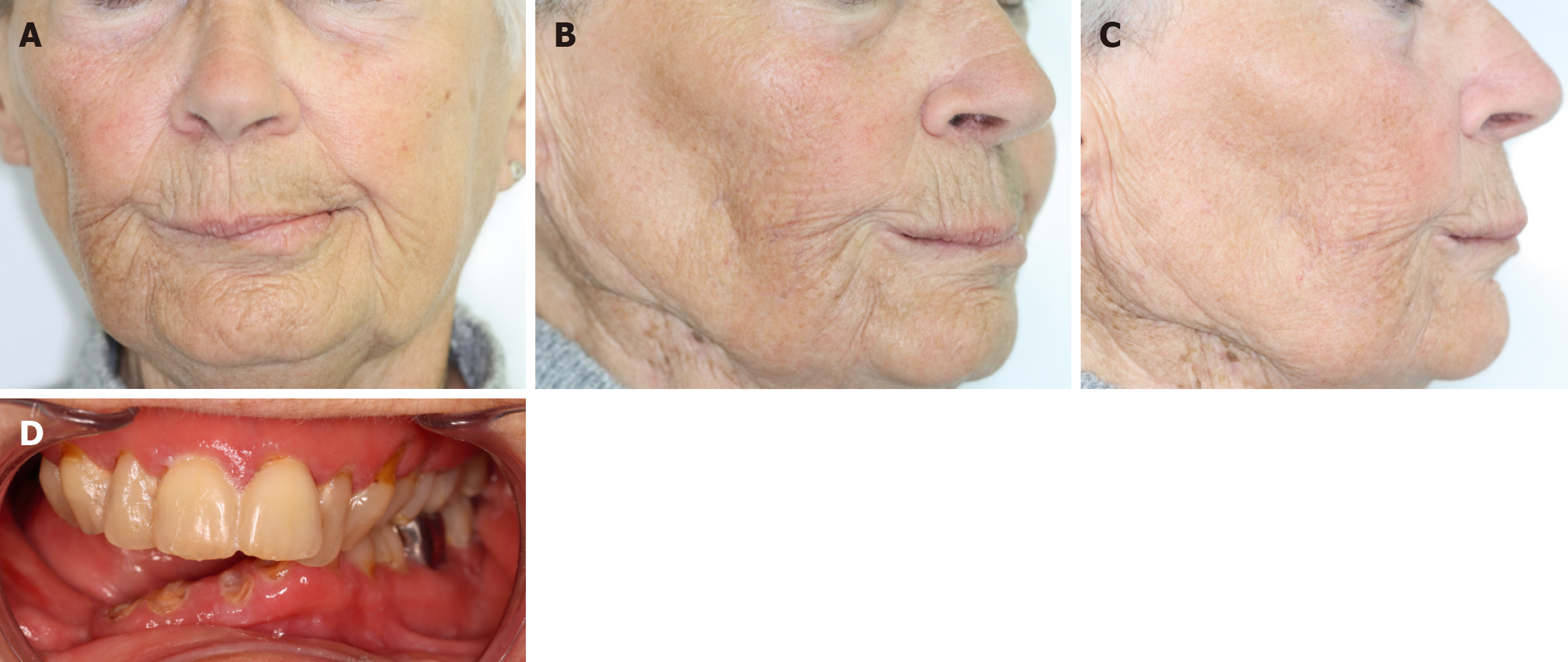
Extraoral examination revealed marked facial asymmetry, with soft tissue collapse of the right cheek and loss of support in the right lower lip. Intraoral examination showed severe trismus, with a maximum mouth opening of 15 mm. Generalized gingival inflammation and poor oral hygiene were noted, along with substantial, extensive plaque accumulation, thick and scanty saliva, and a posterior mandibular edentulous space at tooth 43. Root remnants were present at teeth 16, 17, 31, 32, 41, and 42, accompanied by multiple carious lesions (Figure 1).
No laboratory-related tests were performed in this case.
Radiographic evaluation confirmed the stability of the mandibular reconstruction with no evidence of malignant recurrence. However, due to restricted mouth opening, retroalveolar imaging was challenging. Panoramic and periapical radiographs revealed widespread carious lesions on teeth 15, 14, 13, 12, 11, 21, 22, 23, 24, 26, 33, and 37 (Figure 2).
Dental diagnoses included extensive post-radiation carious lesions and external root resorptions, Kennedy-Applegate class II edentulism (posterior unilateral edentulism[24]), radiation-induced trismus, gingivitis, xerostomia, and soft-tissue deficits following surgical resection and facial asymmetry. These factors contributed to functional impairment and aesthetic problems.
The treatment plan aimed to restore oral function and aesthetics in a patient who had undergone extensive surgical reconstruction after cancer therapy. This multidisciplinary approach addressed dental decay, occlusal dysfunction, radiation-induced complications, and facial asymmetry secondary to soft tissue and bone loss. The patient’s dental care focused on restoring function and aesthetics while treating complications resulting from oncology treatment. Initial management focused on the conservative treatment of carious lesions using minimally invasive techniques. Selective excavation was performed via a palatal approach, followed by the placement of glass ionomer restorations or biodentine, as indicated. Root remnants were preserved to reduce the risk of osteoradionecrosis, a critical consideration in irradiated tissues. Additionally, temporary direct composite restorations were placed on teeth 26 and 27 to facilitate progressive mouth-opening exercises (Figure 3A).
Oral hygiene protocols were reinforced through patient education, including individualized instruction on brushing technique and the recommendation of agents to stimulate salivary flow[13,25]. A custom fluoride tray was fabricated from digital impressions to aid in the prevention of radiation-induced dental caries. A 2000 ppm fluoride gel was prescribed for lifelong use, with the patient demonstrating high compliance, requiring only minor modifications to accommodate gingival sensitivity[26,27]. Fluoride trays are presented in Figure 3B.
An optical impression was captured using the 3Shape intraoral scanner[28], and a transitional mandibular removable prosthesis with a hard base was fabricated, extending from teeth 32 to 46. This prosthesis served multiple functions: Re-establishing posterior occlusal support, enhancing masticatory efficiency, stabilizing the occlusal relationship, and contributing to neuromuscular and temporomandibular joint rehabilitation. Due to the presence of residual roots and the associated risk of osteoradionecrosis, extractions were deferred when clinically feasible[29]. The prosthesis also provided external labial support and partially compensated for jugal soft tissue loss, contributing to improved facial contour (Figure 4). To address residual facial asymmetry and volume loss, HA injections were administered, with particular attention to the right perioral and lower facial regions. The HA injections improved tissue hydration, restored structural support, and helped correct scar-associated contour deformities. This intervention significantly enhanced the patient’s facial aesthetics and psychosocial well-being, providing an important adjunct to the overall reconstructive strategy[12,14].
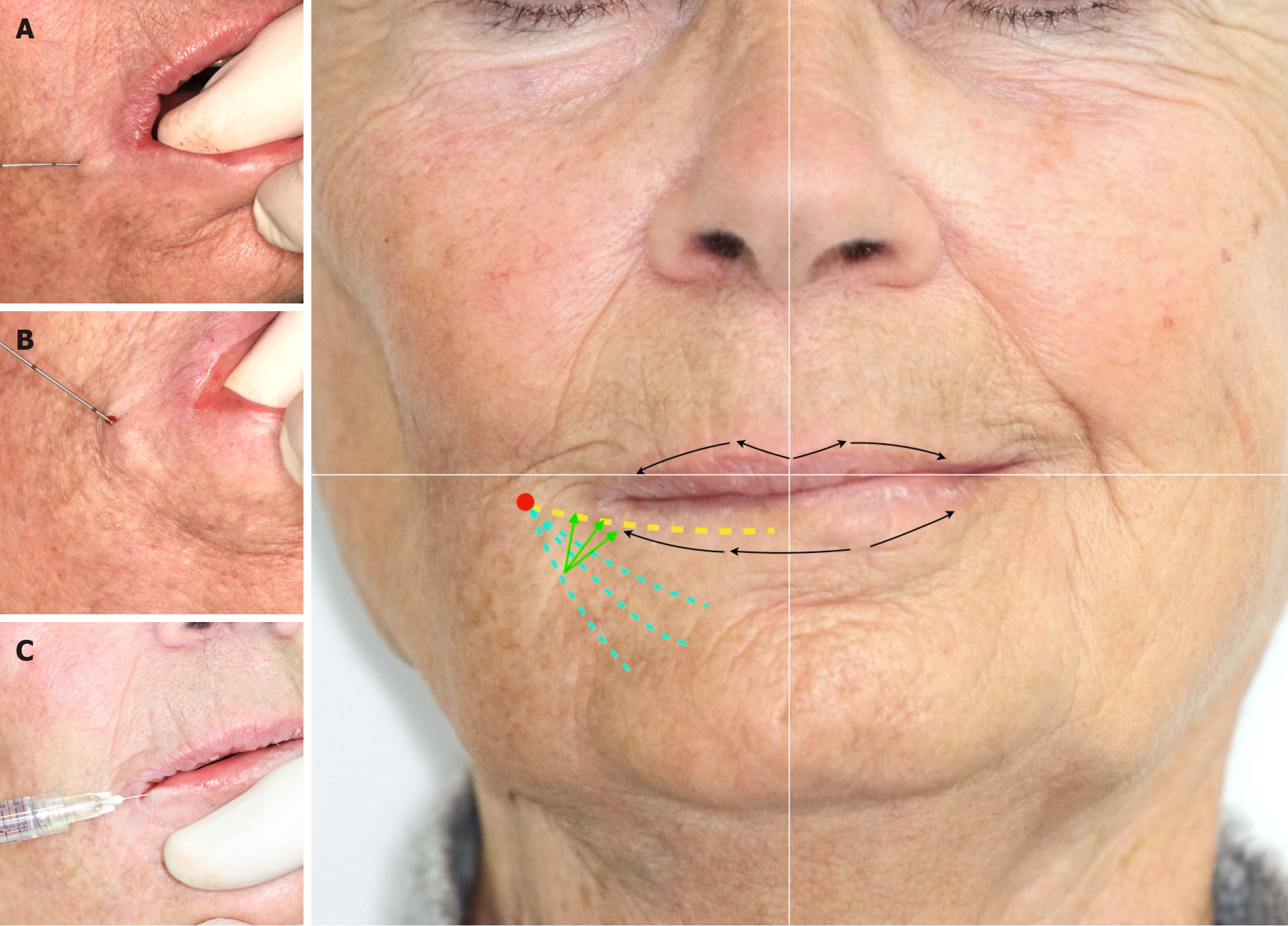
The procedure began with local asepsis using 2% aqueous chlorhexidine, followed by an anesthetic nerve block with 2% articaine without vasoconstrictor, targeting the branches of the right mental nerve. The operator injected the reticulated HA filler (25 mg/mL) with a 25-G cannula inserted laterally to the modiolus. The cannula entered the lower lip to recreate labial volume, first in the red lip area and then in the white lip area. The operator elevated the right labial commissure (marionette line) using 27-G sharp needle injections, delivering the material in a fan shape from a single needle entry point (the tip of the “fan”). By directing the needle upward, the operator added more volume to the mouth corners, reinforcing the supportive effect. Finally, retrograde injections along the lip vermilion restored lip shape. A total of 2 mL of HA was injected. Injection techniques are presented and illustrated in Figure 5.
This treatment provided a double benefit. Aesthetic Improvement: By restoring volume, HA injections rebalanced the patient's facial symmetry and reduced the appearance of surgical scars, contributing to a marked improvement in self-confidence. Functional Enhancement: By compensating for the loss of soft tissue, injections have improved the fit and comfort of prostheses, particularly when tissue healing and contraction interfered with the fit and stability of braces. The procedure was minimally invasive, well-tolerated, and performed in two sessions to optimize results. The patient, initially hesitant because she feared the result would be too artificial, was very satisfied from the very first follow-up visit. Facial pictures taken during the follow-up period are presented in Figure 6.
This approach is in line with current literature supporting the use of HA in post-oncology rehabilitation, particularly for scar modulation, soft tissue augmentation, and aesthetic enhancement[17,18]. These injections illustrate the potential of adjunctive therapies to improve both functional recovery and psychological well-being in patients undergoing complex oral and maxillofacial rehabilitation[30,31]. Dental rehabilitation significantly improved the patient's oral function and aesthetics. The removable mandibular prosthesis successfully restored occlusal support, allowing the patient to regain masticatory efficiency, improve exobuccal aesthetics, and improve phonation. After adjustments, the prosthesis was stable and comfortable, with no major complaints reported at follow-up visits. The fluoride tray helped mitigate the risk of demineralization, despite occasional sensitivity requiring a change in the application schedule. Restorative treatments, including dental cavity management and occlusal composite bonding, stabilized the dentition and improved the occlusal relationship, thereby reducing discomfort and functional deviations.
HA injections have provided substantial aesthetic benefits by correcting facial asymmetry and increasing perioral soft tissue volume. These treatments also had a positive psychosocial impact, as the patient reported greater confidence and satisfaction with her appearance; she reported being less afraid of the looks of others in the street. Regular follow-up visits allowed for prosthesis adjustments, monitoring of dental and soft tissue health, and reinforcement of oral hygiene practices. The overall result was considered very satisfactory, meeting both the functional and aesthetic challenges posed by intensive oncological treatment (Table 1).
| Year | Treatment timeline |
| 2020 | Diagnosis of OSCC, surgical interruptive, reconstruction, and adjuvant radiochemotherapy |
| 2021-2023 | Follow-up visits. Radiographs confirmed stable reconstruction of the mandibular defect with no signs of malignant recurrence; the right mandibular segment demonstrated radiographic stability, and soft tissue imaging was consistent with postsurgical changes |
| 2023 | Management of trismus, caries, posterior wedging, manufacture of a removable muco-supported prosthesis, xerostomia, and gingivitis |
| 2024 | Prosthetic modifications, including denture rebasing of the removable prosthesis; HA injections were administered to treat soft tissue asymmetry and scar-related deficits, with significant aesthetic improvement |
Mouth-opening gradually improved during prosthetic rehabilitation, with an interincisal distance increasing from 15 mm at baseline to 22 mm after a few months. This objective interincisal distance could not be followed as mandibular incisors were lost during oral rehabilitation. The patient-reported outcomes were significant at 12 months, with the patient reporting improved symmetry and confidence. Prosthesis comfort was rated as “excellent” from the third month onward. The patient remained free of oncologic recurrence during the entire follow-up period, without dental caries reappearance, and no HA-related adverse events were reported.
This case highlights the complexity and multidisciplinary nature of oral rehabilitation in a patient previously treated for advanced cervical cancer with extensive surgery and adjuvant chemoradiotherapy. In the absence of cancer recurrence to date, rehabilitative efforts have focused on addressing the significant functional and aesthetic complications resulting from oncologic treatment. The integration of a removable mandibular prosthesis, fluoride trays, conservative caries management, occlusal bonding, and HA injections illustrates a comprehensive and individualized approach that balances clinical efficacy with patient-centered care.
The clinical interventions demonstrated a clear causal relationship with the observed outcomes. The use of custom fluoride trays contributed to the prevention of radiation-induced caries, while the mandibular prosthesis successfully restored occlusal support, masticatory function, and contributed to neuromuscular and articular rehabilitation. HA injections, targeted to correct post-surgical soft tissue asymmetries and volume deficits, significantly enhanced facial aesthetics and self-image. Over time, improvements were also observed in trismus and oral hygiene compliance, supporting the logical sequencing and effectiveness of the chosen treatment modalities. Future care is planned to include a metal-based removable partial denture, continued caries surveillance, and periodic HA injections - guided by ongoing neuro-musculoskeletal rehabilitation.
This case is notable for the successful management of multiple concurrent challenges, including restricted oral access, severe trismus, high caries risk, and psychosocial consequences of oncologic treatment. Key features include: (1) The use of HA for aesthetic rehabilitation in a post-mandibulectomy context, a strategy that remains underreported in the literature; (2) The adaptation of removable prosthetic design to accommodate limited prosthetic space and compromised soft tissue support; and (3) The effective integration of preventive measures - such as fluoride trays - within a broader rehabilitative framework.
This report underscores the adaptability required in dental and maxillofacial care for medically complex patients. The incorporation of aesthetic interventions, particularly HA injections, into functional rehabilitation plans illustrates the potential for innovation in improving outcomes for this population. Such interdisciplinary approaches may not only restore oral function but also contribute significantly to psychosocial recovery and patient satisfaction.
Despite encouraging outcomes, several limitations merit discussion: (1) Severe trismus necessitated multiple prosthetic adjustments and precluded the use of optimal techniques, such as the placement of composite resin under rubber dam isolation; (2) Aesthetic outcomes were assessed through patient-reported satisfaction rather than objective soft tissue measurement tools, limiting standardization and reproducibility; and (3) The current follow-up period is insufficient to assess long-term prosthetic durability and soft tissue volume stability.
Additionally, outcome variability must be considered in relation to patient adherence, systemic health status, and institutional resource availability. These factors highlight the need for future studies exploring standardized, evidence-based protocols that integrate both functional and aesthetic rehabilitation. While this single case demonstrates feasibility, its generalizability remains limited. Future research should include prospective cohorts with standardized outcome measures to validate reproducibility, long-term efficacy, and complication rates of combined prosthetic and HA-based rehabilitation in post-oncologic patients.
This case supports several key recommendations for future clinical practice: (1) Early and close collaboration among oncologists, maxillofacial surgeons, and dental professionals to streamline rehabilitation timelines and outcomes; (2) Integration of HA injections as a valuable adjunct in managing facial volume loss and aesthetic imbalance following oncologic surgery; and (3) Ongoing patient education and preventive care as central components of long-term success in post-cancer oral rehabilitation.
This case report demonstrates that significant functional and aesthetic restoration is achievable in medically complex patients through a personalized, multidisciplinary approach. The strategic integration of novel aesthetic techniques into established dental rehabilitation protocols reflects a promising path forward in comprehensive post-oncologic care. It highlights the importance of an interdisciplinary approach in the dental rehabilitation of a patient with OSCC treated by segmental mandibulectomy and fibula free flap reconstruction. The use of fluoride trays, removable mandibular prostheses, caries management, occlusal surface restorations, and HA injections has shown positive outcomes in restoring both function and esthetics. Evidence supports that these interventions are essential for improving oral health, quality of life, and patient satisfaction[2,13]. Clinicians should prioritize individualized care plans that address functional, aesthetic, and psychological needs. This case provides preliminary feasibility data; future controlled studies are needed to validate efficacy and reproducibility, and future research should focus on the long-term outcomes of prosthetic rehabilitation in patients with mandibular reconstruction and the role of adjunctive therapies, such as HA, in optimizing results. This case also highlights the need for continued advancements in dental rehabilitation strategies to address the complexities of post-oncologic care, including the consideration of fibular dental implants during multidisciplinary meetings, ideally with the participation of an oral or dental surgeon.
| 1. | Matsuda Y, Jayasinghe RD, Zhong H, Arakawa S, Kanno T. Oral Health Management and Rehabilitation for Patients with Oral Cancer: A Narrative Review. Healthcare (Basel). 2022;10:960. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 2. | Zeman-Kuhnert K, Gaggl AJ, Bottini GB, Wittig J, Zimmermann G, Steiner C, Lauth W, Brandtner C. Long-Term Outcomes of Dental Rehabilitation and Quality of Life after Microvascular Alveolar Ridge Reconstruction in Patients with Head and Neck Cancer. J Clin Med. 2024;13:3110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 3. | Epstein JB, Thariat J, Bensadoun RJ, Barasch A, Murphy BA, Kolnick L, Popplewell L, Maghami E. Oral complications of cancer and cancer therapy: from cancer treatment to survivorship. CA Cancer J Clin. 2012;62:400-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 332] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 4. | Kranjčić J, Džakula N, Vojvodić D. Simplified Prosthetic Rehabilitation of a Patient after Oral Cancer Removal. Acta Stomatol Croat. 2016;50:258-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Sivan V, Vozenin-Brotons MC, Tricaud Y, Lefaix JL, Cosset JM, Dubray B, Martin MT. Altered proliferation and differentiation of human epidermis in cases of skin fibrosis after radiotherapy. Int J Radiat Oncol Biol Phys. 2002;53:385-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Hidalgo DA, Pusic AL. Free-flap mandibular reconstruction: a 10-year follow-up study. Plast Reconstr Surg. 2002;110:438-49; discussion 450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 282] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 7. | Thiele OC, Seeberger R, Engel M, Freier K, Hoffmann J. Development of the clinical use of distant flaps for head and neck reconstruction. J Craniomaxillofac Surg. 2014;42:79-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Schrag C, Chang YM, Tsai CY, Wei FC. Complete rehabilitation of the mandible following segmental resection. J Surg Oncol. 2006;94:538-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Petrovic I, Rosen EB, Matros E, Huryn JM, Shah JP. Oral rehabilitation of the cancer patient: A formidable challenge. J Surg Oncol. 2018;117:1729-1735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 10. | Vosselman N, Alberga J, Witjes MHJ, Raghoebar GM, Reintsema H, Vissink A, Korfage A. Prosthodontic rehabilitation of head and neck cancer patients-Challenges and new developments. Oral Dis. 2021;27:64-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 11. | Dimmock M, Alshehri S, Delanoë F, Pradines M, Georg S, Lauwers F, Lopez R. Oral rehabilitation after squamous cell carcinoma mandibular resection. J Oral Med Oral Surg. 2021;27:52. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Aubry S, Collart-Dutilleul PY, Renaud M, Batifol D, Montal S, Pourreyron L, Carayon D. Benefit of Hyaluronic Acid to Treat Facial Aging in Completely Edentulous Patients. J Clin Med. 2022;11:5874. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Yuwanati M, Gondivkar S, Sarode SC, Gadbail A, Desai A, Mhaske S, Pathak SK, N Khatib M. Oral health-related quality of life in oral cancer patients: systematic review and meta-analysis. Future Oncol. 2021;17:979-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 14. | La Gatta A, Salzillo R, Catalano C, D'Agostino A, Pirozzi AVA, De Rosa M, Schiraldi C. Hyaluronan-based hydrogels as dermal fillers: The biophysical properties that translate into a "volumetric" effect. PLoS One. 2019;14:e0218287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 15. | Toole BP. Hyaluronan is not just a goo! J Clin Invest. 2000;106:335-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 112] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Rohrich RJ, Bartlett EL, Dayan E. Practical Approach and Safety of Hyaluronic Acid Fillers. Plast Reconstr Surg Glob Open. 2019;7:e2172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 84] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 17. | Primavera G, Carrera M, Berardesca E, Pinnaró P, Messina M, Arcangeli G. A double-blind, vehicle-controlled clinical study to evaluate the efficacy of MAS065D (XClair), a hyaluronic acid-based formulation, in the management of radiation-induced dermatitis. Cutan Ocul Toxicol. 2006;25:165-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Ringer J, Morrison B, Kingsley K. Evaluation of Hyaluronic Acid to Modulate Oral Squamous Cell Carcinoma Growth In Vitro. J Funct Biomater. 2020;11:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Ferguson EL, Roberts JL, Moseley R, Griffiths PC, Thomas DW. Evaluation of the physical and biological properties of hyaluronan and hyaluronan fragments. Int J Pharm. 2011;420:84-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Sudhakar K, Ji SM, Kummara MR, Han SS. Recent Progress on Hyaluronan-Based Products for Wound Healing Applications. Pharmaceutics. 2022;14:2235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 21. | Chen M, Li L, Wang Z, Li P, Feng F, Zheng X. High molecular weight hyaluronic acid regulates P. gingivalis-induced inflammation and migration in human gingival fibroblasts via MAPK and NF-κB signaling pathway. Arch Oral Biol. 2019;98:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 22. | Schnorr NGP, Salazar-Gamarra R, Latuff DC, Dib LL. Oculofacial Prosthetic Rehabilitation Complemented With Temporary Fillers and Neurotoxin. J Craniofac Surg. 2022;33:e482-e488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 23. | Lydiatt WM, Patel SG, O'Sullivan B, Brandwein MS, Ridge JA, Migliacci JC, Loomis AM, Shah JP. Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67:122-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 893] [Cited by in RCA: 1103] [Article Influence: 122.6] [Reference Citation Analysis (0)] |
| 24. | Şakar O. Classification of Partially Edentulous Arches. In: Şakar O, editor. Removable Partial Dentures. Cham: Springer International Publishing, 2016: 21-25. [DOI] [Full Text] |
| 25. | Hong CH, Napeñas JJ, Hodgson BD, Stokman MA, Mathers-Stauffer V, Elting LS, Spijkervet FK, Brennan MT; Dental Disease Section, Oral Care Study Group, Multi-national Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO). A systematic review of dental disease in patients undergoing cancer therapy. Support Care Cancer. 2010;18:1007-1021. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 205] [Cited by in RCA: 173] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 26. | Epstein JB, van der Meij EH, Lunn R, Stevenson-Moore P. Effects of compliance with fluoride gel application on caries and caries risk in patients after radiation therapy for head and neck cancer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:268-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 56] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Spak CJ, Johnson G, Ekstrand J. Caries incidence, salivary flow rate and efficacy of fluoride gel treatment in irradiated patients. Caries Res. 1994;28:388-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 28. | Desoutter A, Subsol G, Bouchiha K, Benmoumen I, Cuisinier F, Fages M, Carayon D. Unified protocol to evaluate intraoral scanner resolution, trueness and precision: the RTP-protocol. Metrol Meas Syst. 2024. [DOI] [Full Text] |
| 29. | El-Rabbany M, Duchnay M, Raziee HR, Zych M, Tenenbaum H, Shah PS, Azarpazhooh A. Interventions for preventing osteoradionecrosis of the jaws in adults receiving head and neck radiotherapy. Cochrane Database Syst Rev. 2019;2019:CD011559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Monheit GD, Coleman KM. Hyaluronic acid fillers. Dermatol Ther. 2006;19:141-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 124] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 31. | Bass LS. Injectable Filler Techniques for Facial Rejuvenation, Volumization, and Augmentation. Facial Plast Surg Clin North Am. 2015;23:479-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 82] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/