Published online Jan 16, 2026. doi: 10.12998/wjcc.v14.i2.114762
Revised: November 11, 2025
Accepted: December 24, 2025
Published online: January 16, 2026
Processing time: 110 Days and 17.5 Hours
Scorpion envenomation in pregnancy is a rare but potentially fatal obstetric em
A 31-year-old gravida 4, para 3 woman at 36 weeks’ gestation presented 30 min
This case illustrates that scorpion envenomation in late pregnancy poses a dual threat to both maternal and fetal well-being. Prompt recognition, continuous fetal monitoring, and the very early administration of antivenom-buttressed by mul
Core Tip: Scorpion envenomation in pregnancy triggers a dangerous autonomic storm threatening both mother and fetus. We present a successful case of a multigravida at 36 weeks who developed maternal hypertension/tachycardia and fetal tachycardia after a sting by Parabuthus maximus. This case highlights three critical lessons: (1) Scorpion stings are an obstetric emergency requiring immediate fetal monitoring; (2) Early administration of antivenom is a safe and effective definitive treatment in the third trimester and rapidly reverses both maternal and fetal distress; and (3) A coordinated response between obstetrics, toxicology, and critical care is essential to prevent catastrophic outcomes like placental abruption or fetal demise.
- Citation: Omullo FP. Successful management of third-trimester scorpion envenomation (Parabuthus maximus) in a resource-limited setting: A case report. World J Clin Cases 2026; 14(2): 114762
- URL: https://www.wjgnet.com/2307-8960/full/v14/i2/114762.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v14.i2.114762
Scorpion envenomation is a significant public health concern in tropical and subtropical regions[1]. While general management is established, its occurrence during pregnancy is clinically rare and presents a complex management challenge[2]. The venom of neurotoxic species, such as those in the Parabuthus genus, which is common in East Africa, contains potent neurotoxins that induce excessive autonomic neurotransmission, resulting in a catecholamine surge[3]. This can manifest as hypertension, tachycardia, pulmonary edema, and priapism[4]. In pregnancy, these effects can severely reduce uteroplacental perfusion, potentially causing fetal hypoxia, tachycardia, preterm labor, or even in
A 31-year-old woman, gravida 4, para 3, at 36 weeks of gestation, presented with acute severe right foot pain, agitation, and palpitations following a scorpion sting.
The patient was walking barefoot at approximately 07:30 AM when she felt a sudden sharp pain in her right foot. She immediately saw and captured the scorpion, which was later identified as Parabuthus maximus (Figure 1). Within minutes, she developed intense local pain, paresthesia, and warmth at the sting site. Over the next 30 minutes, she developed systemic symptoms including restlessness, profuse sweating, nausea, drooling, and a sensation of her “heart beating out of her chest”. She also reported a notable increase in fetal movements. Before arrival, a family member had applied a dark paste mixture of Kiwi shoe polish and Colgate toothpaste to the wound as traditional first aid (Figure 2).
The patient had a history of regular menstrual cycles, with her last menstrual period on November 2, 2024 and an estimated date of delivery on August 9, 2025. She had used Depo-Provera as contraception and reported no history of dysmenorrhea. The patient was gravida 4, para 3, with three prior uncomplicated vaginal deliveries.
The patient had no history of chronic medical conditions like hypertension, diabetes, or cardiac disease. No known drug allergies.
She lives in a region endemic to scorpions (Lodwar, Kenya). She is a homemaker with no history of smoking, alcohol, or substance use and no significant family history of genetic or autoimmune disorders.
On examination, the patient was anxious, agitated, and diaphoretic. Vital signs: Blood pressure 168/102 mmHg, pulse 142 bpm, respiratory rate 24/minutes, temperature 37.8 °C, SpO2 98% on room air. Local exam revealed a single puncture wound on the plantar right foot with 6 cm of surrounding erythema and marked hyperesthesia. The cardiovascular exam revealed a tachycardic rhythm with no murmurs. The patient’s lungs were clear to auscultation. Abdominopelvic exams showed a gravid uterus consistent with 36 weeks of gestation, soft, non-tender; fetal lie was longitudinal and presentation was cephalic. The neurological exam revealed hyperreflexia in the right lower limb, without cranial nerve deficits or motor weakness.
Laboratory investigations, including a complete blood count, comprehensive metabolic panel, and inflammatory markers, were within normal limits, except for an elevated C-reactive protein level (75.2 mg/L), a nonspecific finding likely reflecting the systemic inflammatory and stress response to envenomation (Tables 1, 2, 3, and 4).
| Parameter | Units | Results | Reference range |
| WBC | × 109/L | 4.69 | 4.0-10.8 |
| Neutrophils | % | 32.8 | 40-75 |
| Lymphocytes | % | 59.9 | 21-40 |
| Monocytes | % | 5.4 | 3-12 |
| Eosinophils | % | 1.4 | 0.5-5 |
| Basophils | % | 0.5 | 0.5-5 |
| RBC | × 109/L | 4.56 | 4.7-6.1 |
| HB | g/dL | 12.6 | 11.2-16.0 |
| HCT | % | 38.3 | 37.0-47.0 |
| MCV | fL | 83.9 | 76.0-100.0 |
| MCH | Pg | 27.5 | 27.0-31.0 |
| MCHC | g/dL | 32.8 | 32.0-36.0 |
| RDW-C | % | 13.8 | 11.5-14.5 |
| Platelets count | × 109/L | 202 | 160.0-450.0 |
| MPV | fL | 9.1 | 6.5-12.0 |
| PDW | % | 15.9 | 9.0-17.0 |
| PCT | % | 0.228 | 0.108-0.282 |
| Parameter | Units | Results | Reference range |
| Albumin | g/L | 36.33 | 35-52 |
| ALP | U/L | 38.1 | 35-104 |
| ALT | U/L | 34.2 | 0-40 |
| AST | U/L | 33.9 | 0-32 |
| GGT | U/L | 6.7 | 5-36 |
| Total protein | g/L | 68.4 | 66-87 |
| Parameter | Units | Results | Reference range |
| Chloride | mmol/L | 101.5 | 95-107 |
| Creatinine | µmol/L | 68 | 44-80 |
| Potassium | mmol/L | 3.86 | 3.5-5.1 |
| Sodium | mmol/L | 135.7 | 135-145 |
| Urea | mmol/L | 4.64 | 2.76-8.07 |
| Parameter | Units | Results | Reference range |
| CRP | mg/L | 75.2 | 0-10.0 |
Abdominopelvic ultrasound: A single viable fetus in cephalic presentation was identified, with an estimated fetal weight appropriate for gestational age. Normal amniotic fluid index. Cardiotocography: Revealed a fetal heart rate baseline of 175-180 bpm (tachycardia) with reduced variability.
Given the maternal autonomic crisis and concomitant fetal tachycardia, a multidisciplinary team comprising obstetrics, toxicology, and anesthesia/intensive care unit was convened. The consensus was to administer scorpion-specific antivenom (effective against Parabuthus species) as the definitive treatment for systemic envenomation, along with ongoing supportive care. The availability of the captured scorpion was pivotal in confirming the species and justifying the immediate use of this specific antivenom. The obstetrics team mandated continuous fetal monitoring throughout the crisis.
Systemic scorpion envenomation syndrome (due to Parabuthus maximus) with autonomic storm complicating pregnancy at 36 weeks of gestation.
Treatment was initiated immediately with a multi-pronged approach. Supportive care commenced with intravenous morphine (4 mg) for severe pain, followed by intravenous midazolam (2 mg, repeated once) to manage agitation and autonomic symptoms. As definitive therapy, one vial of intravenous South African vaccine producers polyvalent scorpion antivenom (Batch: SA106; composition: F(ab')2 fragments against Parabuthus, Androctonus, and Buthus species) was administered to neutralize the circulating venom. The rapid clinical improvement can be attributed to the antivenom neutralizing circulating venom antigens, thereby abruptly halting the pathological autonomic discharge. Concurrent obstetric care involved continuous maternal and fetal monitoring. Betamethasone (12 mg intramuscularly) was administered prophylactically to promote fetal lung maturation due to the significant risk of preterm labor precipitated by the envenomation and autonomic stress.
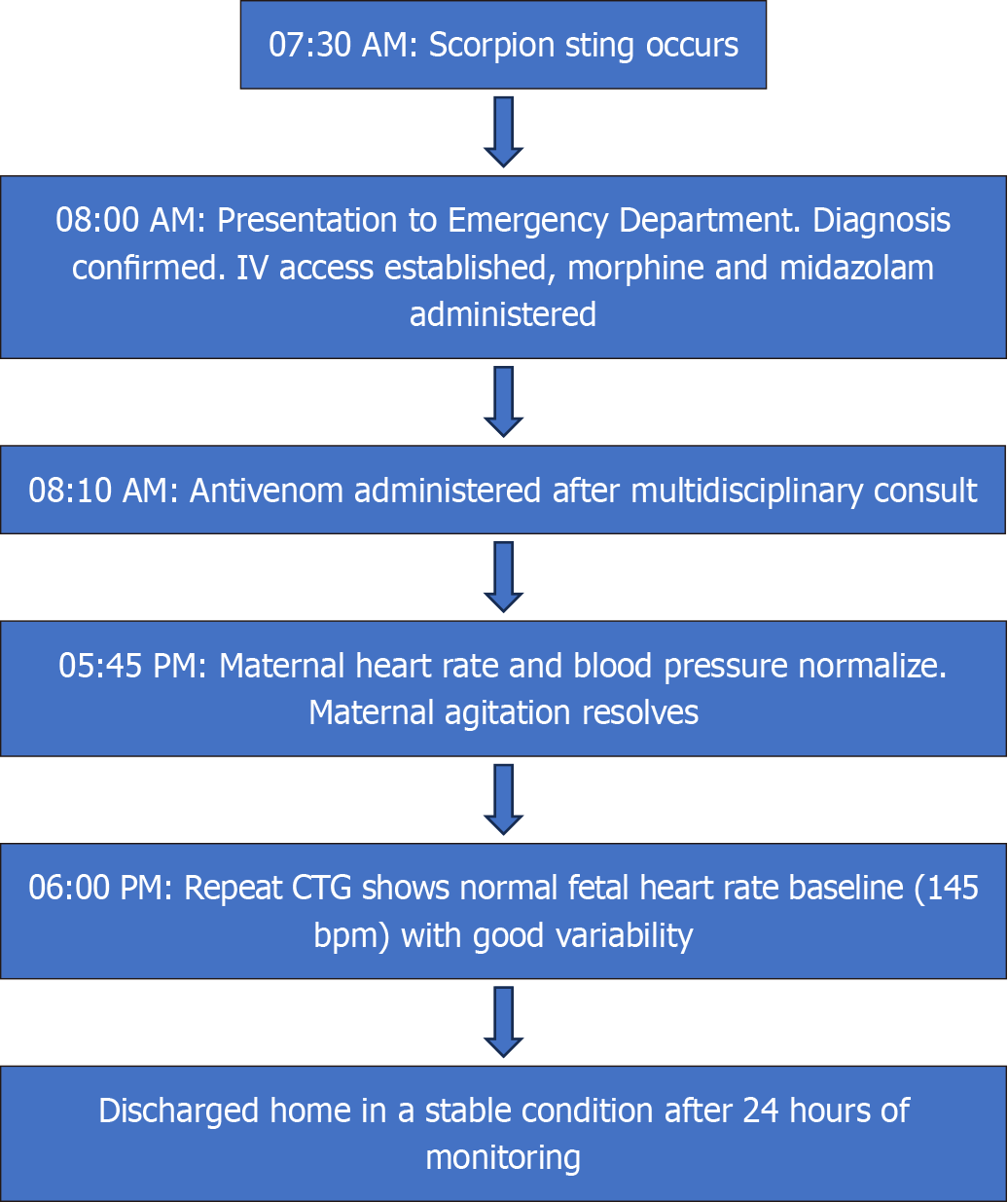
The patient showed dramatic improvement within hours of antivenom administration. Both maternal vitals and fetal heart rate pattern normalized. She was observed for 24 hours with no recurrence of symptoms. She was discharged with routine prenatal follow-up. The pregnancy continued uneventfully to term. She subsequently had a spontaneous vaginal delivery at 38 weeks of gestation of a healthy male infant weighing 3450 g with Apgar scores of 9 and 9 at 1 minute and 5 minutes, respectively. Both mother and baby were well at the 2-week postnatal check as summarized in Figure 3. A pediatrician examined the newborn and showed no signs of adverse neurological or other sequelae. Long-term follow-up for neonatal development was recommended; however, the family was lost to follow-up after the 2-week visit, which is a recognized limitation in this setting.
This case highlights the significant clinical and public health challenges posed by scorpion envenomation during pre
Reported outcomes in the literature are markedly heterogeneous (Table 5). Kaplanoglu and Helvaci[6] described a series of exclusively mild envenomations managed with symptomatic care alone, whereas Leibenson et al[7] documented a tragic stillbirth following envenomation in late pregnancy. A critical outcome differentiator appears to be the time to administer definitive therapy (Table 6). Antivenom was administered within 40 minutes of the sting in the present case. This stands in stark contrast to other series, such as Najafian et al[2], where antivenom was given 6-12 hours post-sting and was associated with an 11% rate of neonatal complications. Larger studies from endemic regions like Iran and Tunisia have further correlated delayed intervention with increased rates of miscarriage, preterm birth, and neonatal complications[2,8]. The rapid clinical resolution observed in our patient following early antivenom administration starkly contrasts these adverse outcomes. It reinforces emerging evidence that timely antivenom is the cornerstone of therapy, capable of reversing both maternal and fetal instability[9,10]. While a single case cannot prove universal safety, this finding contributes to the growing body of evidence that robustly challenges historical hesitancy regarding potential teratogenicity or hypersensitivity reactions and strengthens the imperative for its inclusion in obstetric emergency protocols.
| Ref. | Country | Trimester | Management | Maternal outcome | Fetal outcome |
| Najafian et al[2], 2020 | Iran | All | Antivenom administered 6-12 hours post-sting; supportive care | Stable | 11% neonatal complications; Apgar < 8 in 11.3% of preterm births |
| Ben Nasr et al[8], 2009 | Tunisia | All | Supportive care; antivenom use recommended | Stable | Risk of preterm birth, fetal anomalies, and long-term developmental issues |
| Kaplanoglu and Helvaci[6], 2015 | Turkey | All | Symptomatic care (no antivenom) | Stable | All live births |
| Leibenson et al[7], 2009 | Israel | 3rd | Supportive care | Stable | Stillbirth |
| Brown et al[10], 2013 | Review | All | Supportive care; antivenom for severe cases | Optimal outcomes with early intervention | Improved fetal outcomes with maternal stabilisation |
| Present case, 2025 | Kenya | 3rd | Early antivenom; multidisciplinary care | Full recovery | Healthy neonate |
| Aspect | Clinical implications |
| Pathophysiology | Catecholamine-induced uteroplacental vasoconstriction leading to fetal hypoxia |
| Maternal symptoms | Autonomic storm (hypertension, tachycardia), local pain, potential for severe complications (eclampsia, myocarditis) |
| Fetal effects | Tachycardia, distress, potential preterm labor or demise in severe cases |
| Critical management | Prompt antivenom administration, multidisciplinary care, and continuous fetal monitoring |
| Resource-limited challenges | Antivenom accessibility, harmful traditional practices, and delayed presentation |
A pivotal factor in this success was the accurate identification of the scorpion species. The patient's action of capturing the scorpion removed diagnostic ambiguity, allowing clinicians to administer species-specific antivenom confidently and without delay. This highlights a crucial pre-hospital factor: Community education should strongly emphasize that safely capturing and bringing the scorpion (or a clear photograph) to the healthcare facility is a critical step that directly guides life-saving treatment.
Equally critical to the successful outcome was the coordinated multidisciplinary approach. The seamless integration of obstetric, toxicology, and critical care expertise ensured simultaneous maternal stabilization and vigilant fetal monitoring. Such coordination, although logistically challenging in low-resource environments, is crucial in preventing catastrophic sequelae, such as placental abruption or intrauterine demise.
A pivotal, and likely life-saving, factor in this case was the patient's action of capturing and bringing the scorpion to the hospital. This allowed for precise species identification, which is often impossible but crucial for administering the correct, specific antivenom. This stands as a powerful public health lesson. Community education in endemic areas must emphasize this critical yet straightforward action. Furthermore, the documentation of harmful traditional first-aid practices, such as applying shoe polish and toothpaste, underscores a crucial gap in health literacy and highlights the urgent need for targeted community education programs[11]. These programs should integrate evidence-based first aid into routine prenatal care initiatives.
Key first-aid recommendations for scorpion stings:
Do: Clean the wound with soap and water, immobilize the limb, and transport the patient immediately to the nearest medical facility.
Do: If safe to do so, capture or take a clear photograph of the scorpion for identification.
Do not: Apply a tourniquet, incise the wound, attempt to suck out the venom, or apply herbal concoctions, ice packs, or other non-evidence-based substances.
According to the World Health Organization, scorpion stings affect over 1.2 million people annually, leading to more than 3000 deaths, primarily in underserved communities where access to care and correct information is limited[1]. The escalating global burden of scorpionism[1] necessitates strategic investments in the health system to improve antivenom accessibility at peripheral clinics, as reducing treatment delays remains the single most significant modifiable factor for improving outcomes.
This case report is not without limitations. The absence of long-term developmental follow-up for the neonate means potential delayed effects cannot be entirely ruled out, a challenge common in resource-limited settings. Its nature as a single instance precludes definitive conclusions about causality or generalizability. Nevertheless, it adds a significant data point to the scarce global literature by demonstrating that: (1) Antivenom is both safe and efficacious for third-trimester systemic scorpion envenomation; (2) Multidisciplinary care is indispensable for optimizing outcomes; and (3) Co
Third-trimester scorpion envenomation by Parabuthus maximus presents a grave threat to maternal and fetal survival. This case irrefutably demonstrates that rapid multidisciplinary intervention coupled with very early administration of antivenom can restore maternal hemodynamics and fetal well-being, ensuring an exemplary outcome. The patient’s action of providing the scorpion for identification was a key link in this successful chain of care. Beyond acute clinical care, addressing pre-hospital delays stemming from antivenom inaccessibility and harmful traditional practices through concerted public health education-focusing on evidence-based first aid and the critical importance of scorpion identification and decentralized toxicology management strategies are essential for endemic regions worldwide.
The author gratefully acknowledges the clinical staff at Equity Afya, Lodwar, for their exemplary patient care and collaborative spirit throughout this case.
| 1. | Vasconez-Gonzalez J, Alexander-León H, Noboa-Lasso ML, Izquierdo-Condoy JS, Puente-Villamarín E, Ortiz-Prado E. Scorpionism: a neglected tropical disease with global public health implications. Front Public Health. 2025;13:1603857. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 2. | Najafian M, Ghorbani A, Zargar M, Baradaran M, Baradaran N. Scorpion stings in pregnancy: an analysis of outcomes in 66 envenomed pregnant patients in Iran. J Venom Anim Toxins Incl Trop Dis. 2020;26:e20190039. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Inceoglu B, Lango J, Pessah IN, Hammock BD. Three structurally related, highly potent, peptides from the venom of Parabuthus transvaalicus possess divergent biological activity. Toxicon. 2005;45:727-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Langley RL. A review of venomous animal bites and stings in pregnant patients. Wilderness Environ Med. 2004;15:207-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Abroug F, Ouanes-Besbes L, Tilouche N, Elatrous S. Scorpion envenomation: state of the art. Intensive Care Med. 2020;46:401-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 6. | Kaplanoglu M, Helvaci MR. Scorpion stings in pregnant women: an analysis of 11 cases and review of literature. Clin Exp Obstet Gynecol. 2015;42:228-230. [PubMed] |
| 7. | Leibenson L, Leibenson M, Silberstein T. Antepartum fetal death following a yellow scorpion sting. Arch Gynecol Obstet. 2010;281:247-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Ben Nasr H, Serria H, Chaker S, Riadh B, Zouheir S, Kamel J, Tarek R, Khaled Z. Some biological effects of scorpion envenomation in late pregnant rats. Exp Toxicol Pathol. 2009;61:573-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Ramirez-Cruz MP, Smolinske SC, Warrick BJ, Rayburn WF, Seifert SA. Envenomations during pregnancy reported to the national poison data system, 2009-2018. Toxicon. 2020;186:78-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Brown SA, Seifert SA, Rayburn WF. Management of envenomations during pregnancy. Clin Toxicol (Phila). 2013;51:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/