Published online Jan 16, 2026. doi: 10.12998/wjcc.v14.i2.115462
Revised: November 1, 2025
Accepted: January 6, 2026
Published online: January 16, 2026
Processing time: 91 Days and 10.9 Hours
Erdheim-Chester disease (ECD) is an ultra-rare non-Langerhans cell histiocytosis driven by clonal proliferation of lipid-laden histiocytes. With fewer than a thou
A 46-year-old male presented with chronic leg pain, polyuria, and visual dis
This case represents the first case of ECD reported from Pakistan. Awareness of its distinct imaging and histologic patterns can facilitate diagnosis even in resource-limited settings. National rare disease registries and access to molecular diag
Core Tip: Erdheim-Chester disease, a rare non-Langerhans histiocytosis, can mimic pituitary and other systematic on imaging. Recognition of its characteristic radiologic and immunohistochemical profile enables timely diagnosis and treatment in low-resource settings.
- Citation: Haq M, Bukhari SMRUAN, Basit A, Ismail Q, Jabeen M. Erdheim-Chester disease presenting with multisystem involvement: A case report. World J Clin Cases 2026; 14(2): 115462
- URL: https://www.wjgnet.com/2307-8960/full/v14/i2/115462.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v14.i2.115462
Erdheim-Chester disease (ECD) is a rare clonal histiocytic neoplasm first described in 1930. It is characterized by infiltration of tissues by foamy, lipid-laden histiocytes that are CD68 and CD163 positive but CD1a and Langerin negative. The disease affects multiple organ systems, including the skeleton, retroperitoneum, cardiovascular system, and central nervous system. Global incidence is estimated at fewer than one per million, with a slight male predominance and peak presentation between 40 years and 70 years of age[1,2].
Advances in molecular profiling have identified mutations in the mitogen-activated protein kinase (MAPK) pathway, primarily BRAF V600E, in nearly two-thirds of cases[3]. These discoveries have shifted ECD’s classification from an inflammatory disorder to a neoplastic disease and opened the door for targeted therapies such as vemurafenib[4].
Despite global awareness, ECD remains underdiagnosed in low- and middle-income countries like Pakistan, where advanced molecular and immunohistochemical diagnostics are limited. This case likely represents the first histologically and molecularly confirmed instance of ECD reported from Pakistan. It highlights how recognition of characteristic radiologic and pathologic features can enable diagnosis even in settings without full access to genomic testing.
A 46-year-old male, school teacher by profession a resident of Lahore presented to the outpatient clinic with progressive dull pain in both legs for 18 months, associated with increased thirst, polyuria, and nocturia for one year, and recent blurring of vision over four months.
There was no history of fever, night sweats, tuberculosis exposure, or autoimmune illness.
Unremarkable.
The patient had no significant family history and denied consanguinity.
Physical examination revealed mild right-sided proptosis, tenderness along the tibial shafts, and dry skin. No lym
Initial laboratory workup showed mild normocytic anemia (hemoglobin 12.3 g/dL) and elevated erythrocyte sedi
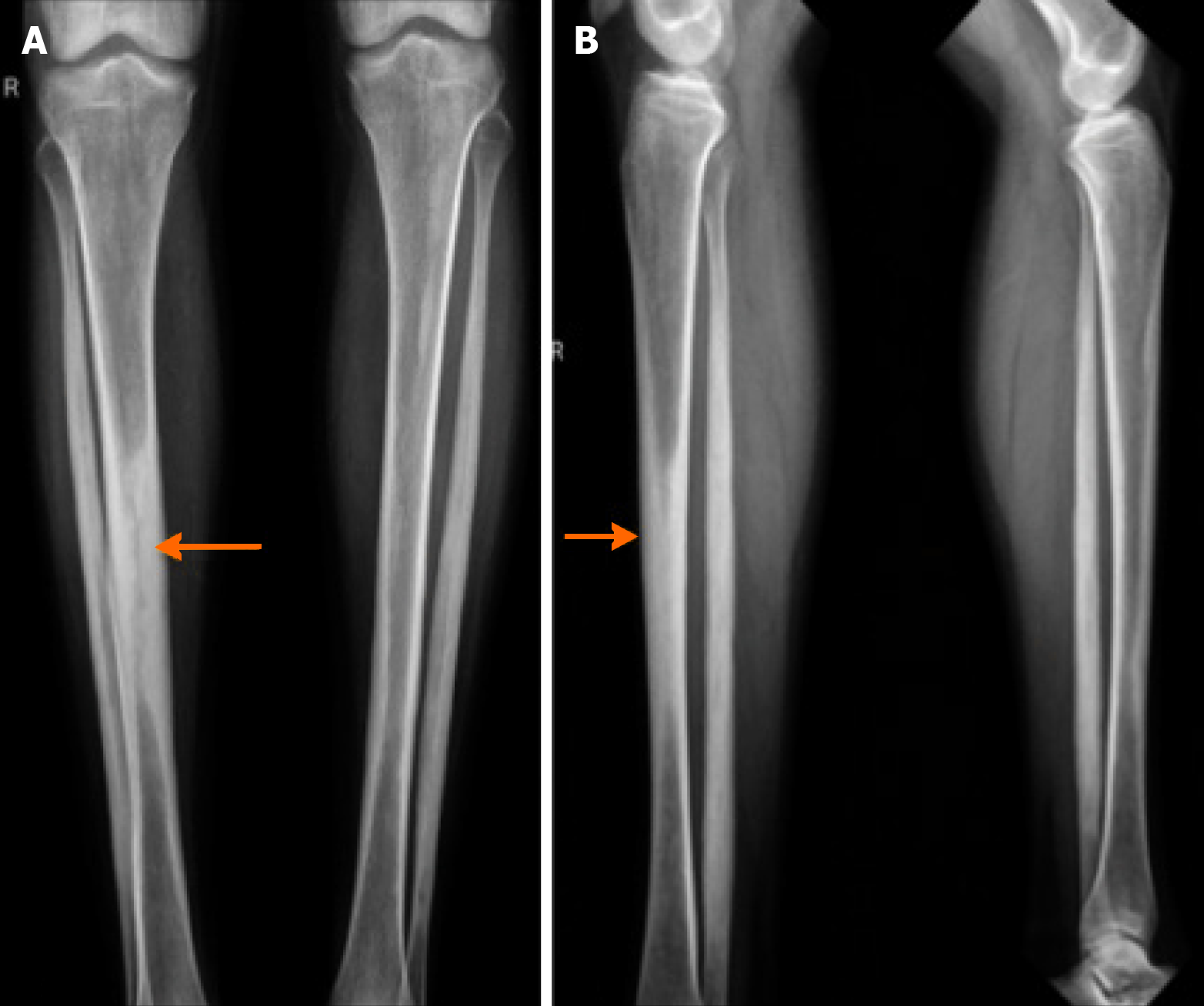
X-rays of both lower limbs demonstrated bilateral, symmetric, osteosclerosis of the metaphyseal-diaphyseal regions (“candle wax” appearance) as shown in Figure 1.
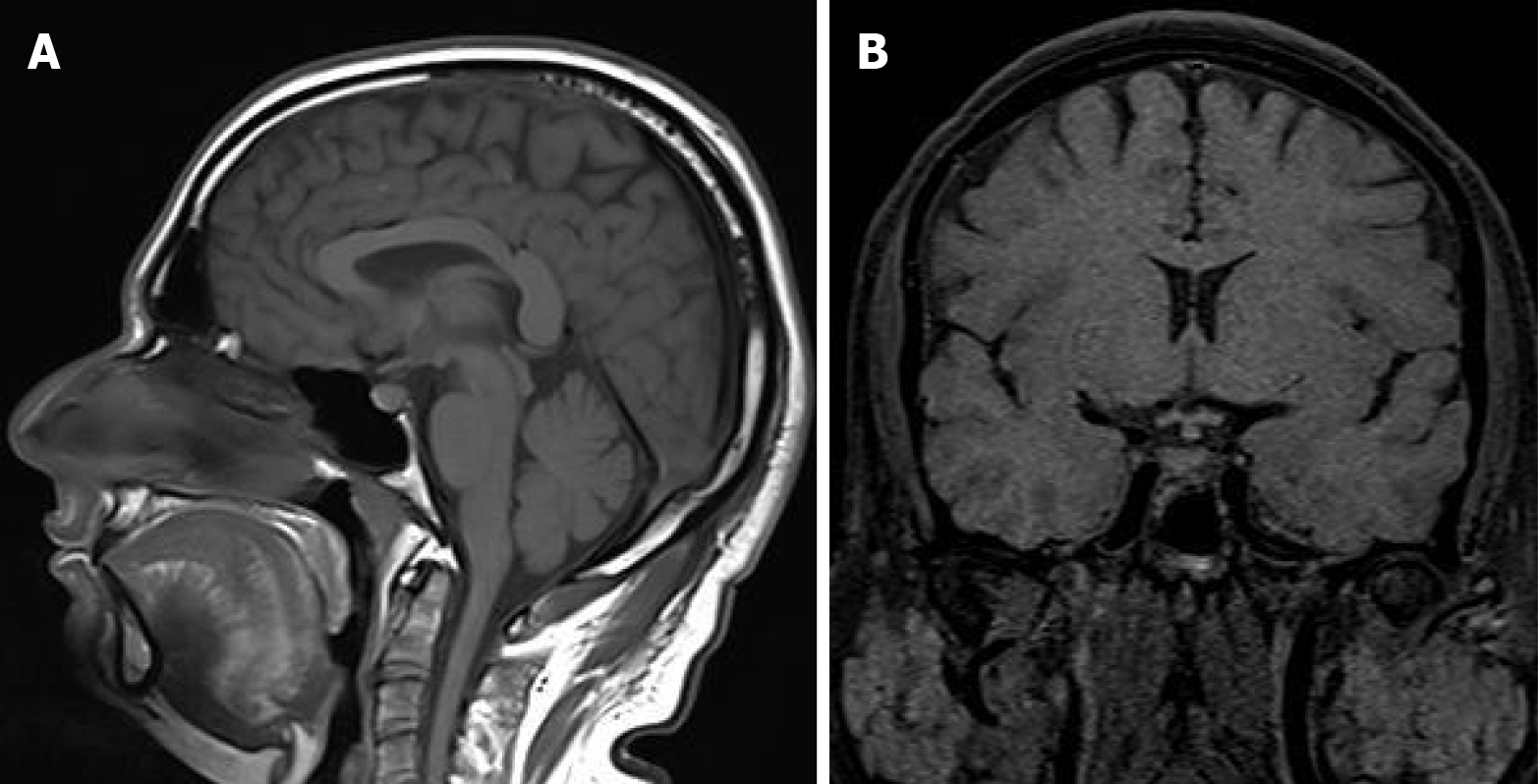
Magnetic resonance imaging (MRI) of the brain showed thickened pituitary stalk and loss of the posterior pituitary bright spot as shown in Figure 2. An open biopsy of the perirenal tissue via computed tomography (CT)-guided biopsy showed dense infiltration of foamy histiocytes with scattered Touton-type giant cells in a fibrotic stroma. Immunohistochemical analysis demonstrated positivity for CD68 and CD163 but negativity for CD1a and Langerin, confirming a non-Langerhans histiocytosis. PCR-based mutation analysis performed in an external laboratory detected BRAF V600E mutation, confirming ECD.
The following are diseases for differential diagnosis: ECD; Langerhans cell histiocytosis; sarcoidosis; immunoglobulin G4-related disease; idiopathic retroperitoneal fibrosis.
The definitive diagnosis was established on the basis of immunological and histopathological testing. The key distinguishing feature of ECD is its unique immunophenotype-it is CD1a- and Langerin-negative, which differentiates it from Langerhans cell histiocytosis, and it often harbors a BRAF V600E mutation, helping to distinguish it from sarcoidosis. The final diagnosis is ECD.
The patient was started on oral prednisolone (40 mg/day, tapered) and subcutaneous interferon-alpha (3 million IU, thrice weekly). Desmopressin nasal spray was initiated for central diabetes insipidus.
At six months’ follow-up, the patient reported improved bone pain and reduced polyuria, with CT showing partial regression of perirenal infiltration and stable skeletal sclerosis.
ECD represents a histiocytic neoplasm within the L-group histiocytoses, characterized by chronic inflammation and tissue infiltration by foamy macrophages. The condition has a striking male predominance and can involve virtually any organ, leading to highly variable clinical presentations[1-3].
The skeletal system is affected in over 90% of patients, typically manifesting as bilateral symmetrical osteosclerosis of long bones, as seen in this patient. Extra-skeletal involvement, particularly in the retroperitoneum, cardiovascular system, and central nervous system, occurs in nearly 60% of cases and determines prognosis[4].
Histopathologically, ECD lesions consist of lipid-laden histiocytes surrounded by fibrosis. The immunophenotype-CD68 and CD163 positive but CD1a and Langerin negative-distinguishes ECD from Langerhans Cell Histiocytosis[2]. The detection of BRAF V600E or other MAPK pathway mutations confirms the clonal nature of the disease[3].
The major challenge in Pakistan is the lack of diagnostic infrastructure, including immunohistochemistry panels and molecular testing for BRAF mutations. Consequently, ECD may be mistaken for idiopathic retroperitoneal fibrosis or granulomatous infections such as tuberculosis, which are far more prevalent. Recognition of characteristic radiologic features can therefore serve as a critical diagnostic clue in resource-limited settings[5].
Treatment strategies depend on mutation status and organ involvement. Targeted therapy with vemurafenib (for BRAF-mutant ECD) has transformed survival outcomes, achieving response rates exceeding 80%[1,6]. However, access to these agents is limited in Pakistan due to cost and regulatory barriers. Interferon-alpha remains a viable option and can stabilize disease in the absence of targeted therapy. Corticosteroids provide short-term symptomatic relief but do not alter long-term outcomes[5,6].
This case illustrates how strategic clinical suspicion, imaging correlation, and basic immunohistochemistry can lead to correct diagnosis even without advanced molecular facilities. Establishing regional referral centers for histiocytic dis
This report describes what is likely the first histologically and molecularly confirmed case of ECD in Pakistan. It de
| 1. | Goyal G, Heaney ML, Collin M, Cohen-Aubart F, Vaglio A, Durham BH, Hershkovitz-Rokah O, Girschikofsky M, Jacobsen ED, Toyama K, Goodman AM, Hendrie P, Cao XX, Estrada-Veras JI, Shpilberg O, Abdo A, Kurokawa M, Dagna L, McClain KL, Mazor RD, Picarsic J, Janku F, Go RS, Haroche J, Diamond EL. Erdheim-Chester disease: consensus recommendations for evaluation, diagnosis, and treatment in the molecular era. Blood. 2020;135:1929-1945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 280] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 2. | Haroche J, Cohen-Aubart F, Rollins BJ, Donadieu J, Charlotte F, Idbaih A, Vaglio A, Abdel-Wahab O, Emile JF, Amoura Z. Histiocytoses: emerging neoplasia behind inflammation. Lancet Oncol. 2017;18:e113-e125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 146] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 3. | Emile JF, Abla O, Fraitag S, Horne A, Haroche J, Donadieu J, Requena-Caballero L, Jordan MB, Abdel-Wahab O, Allen CE, Charlotte F, Diamond EL, Egeler RM, Fischer A, Herrera JG, Henter JI, Janku F, Merad M, Picarsic J, Rodriguez-Galindo C, Rollins BJ, Tazi A, Vassallo R, Weiss LM; Histiocyte Society. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016;127:2672-2681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 722] [Cited by in RCA: 1043] [Article Influence: 104.3] [Reference Citation Analysis (1)] |
| 4. | Mazor RD, Manevich-Mazor M, Shoenfeld Y. Erdheim-Chester Disease: a comprehensive review of the literature. Orphanet J Rare Dis. 2013;8:137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 183] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 5. | Liu J, Gao L, Pu H, He W, Peng L. Erdheim-Chester disease with multisystem involvement evaluated by multimodal imaging: A case report. Radiol Case Rep. 2022;17:784-789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 6. | Guo S, Yan Q, Rohr J, Wang Y, Fan L, Wang Z. Erdheim-Chester disease involving the breast--a rare but important differential diagnosis. Hum Pathol. 2015;46:159-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/