Published online Dec 16, 2025. doi: 10.12998/wjcc.v13.i35.115410
Revised: November 11, 2025
Accepted: December 10, 2025
Published online: December 16, 2025
Processing time: 61 Days and 14.8 Hours
Liposarcoma is the most common soft tissue tumor in adults. Liposarcoma com
We present the case of a 71-year-old male patient with a giant posterior medi
VATS is safer than thoracotomy for treating giant mediastinal liposarcoma. For tumors extensively involving the esophagus, preventive measures against eso
Core Tip: We report a very rare case of giant mediastinal liposarcoma. To the best of our knowledge, this is the first report of bilateral single-port video-assisted thoracoscopic surgery for giant mediastinal liposarcoma and the first report of esophageal fistula after this surgery. This report provided valuable lessons and reference for selection of appropriate surgical approach and the management of postoperative esophageal fistula.
- Citation: Ding YZ, Tang DQ, Zhao XJ. Esophageal fistula after resection of giant mediastinal liposarcoma: A case report. World J Clin Cases 2025; 13(35): 115410
- URL: https://www.wjgnet.com/2307-8960/full/v13/i35/115410.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i35.115410
Mediastinal soft tissue tumors are very rare, accounting for 2%-6% of mediastinal malignancies[1]. Liposarcoma is the most common soft tissue tumor in adults[2] and commonly occurs in the lower extremities and retroperitoneum[3]. There are four histologic sub-types of liposarcoma: Myxoid, well differentiated, dedifferentiated, and pleomorphic[4]. Lipo
Surgery remains the first-choice treatment for mediastinal ALTs[2]. However, ALTs may cause only minimal symp
In the present case, we successfully resected a giant posterior mediastinal ALT involving the esophagus during bilateral single-port video-assisted thoracoscopic surgery (VATS). The patient suffered from esophageal fistula 9 days after surgery and 2 days after eating. To the best of our knowledge, this is the first report of bilateral single-port VATS for giant mediastinal liposarcoma and the first report of esophageal fistula after this surgery. We present our experience with choosing the surgical approach and managing complications.
A 71-year-old male patient presented to the hospital complaining of a giant mediastinal mass, revealed by a computed tomography (CT) scan.
The mass was discovered by CT scan during a routine examination, and the patient had no symptom.
The patient had a history of hypertension and took amlodipine besylate tablets 5 mg qd. The patient was a smoker with 30 pack-years.
The patient was healthy and had no personal or family history of tumors.
The patient presented mild coarse breath sounds in the right upper lung during auscultation.
Laboratory tests revealed an increased percentage of neutrophilic leukocytes (78.4%) with normal hematocrit and platelet count values. Tumor markers such as carcinoembryonic antigen, Carbohydrate antigen (CA) 199, CA125, neuron-specific enolase, and cytokeratin fraction 21-1 were all in the normal range.
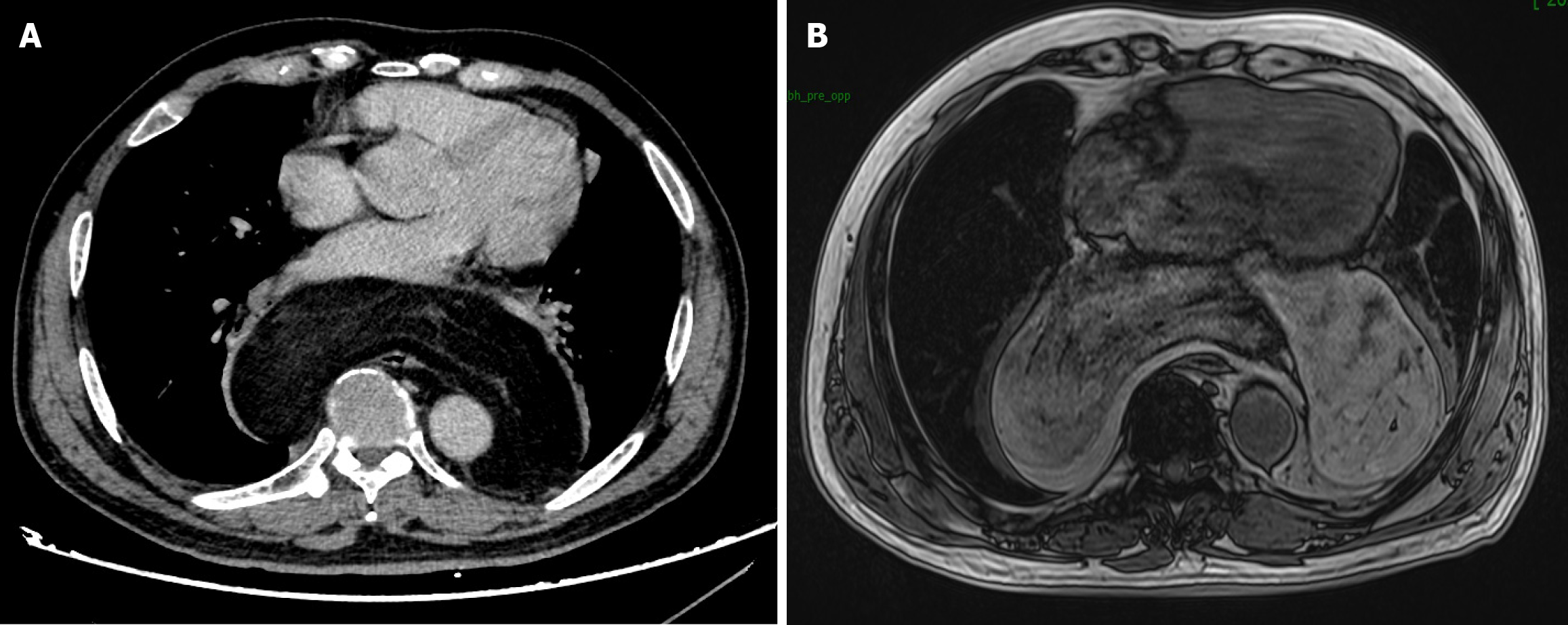
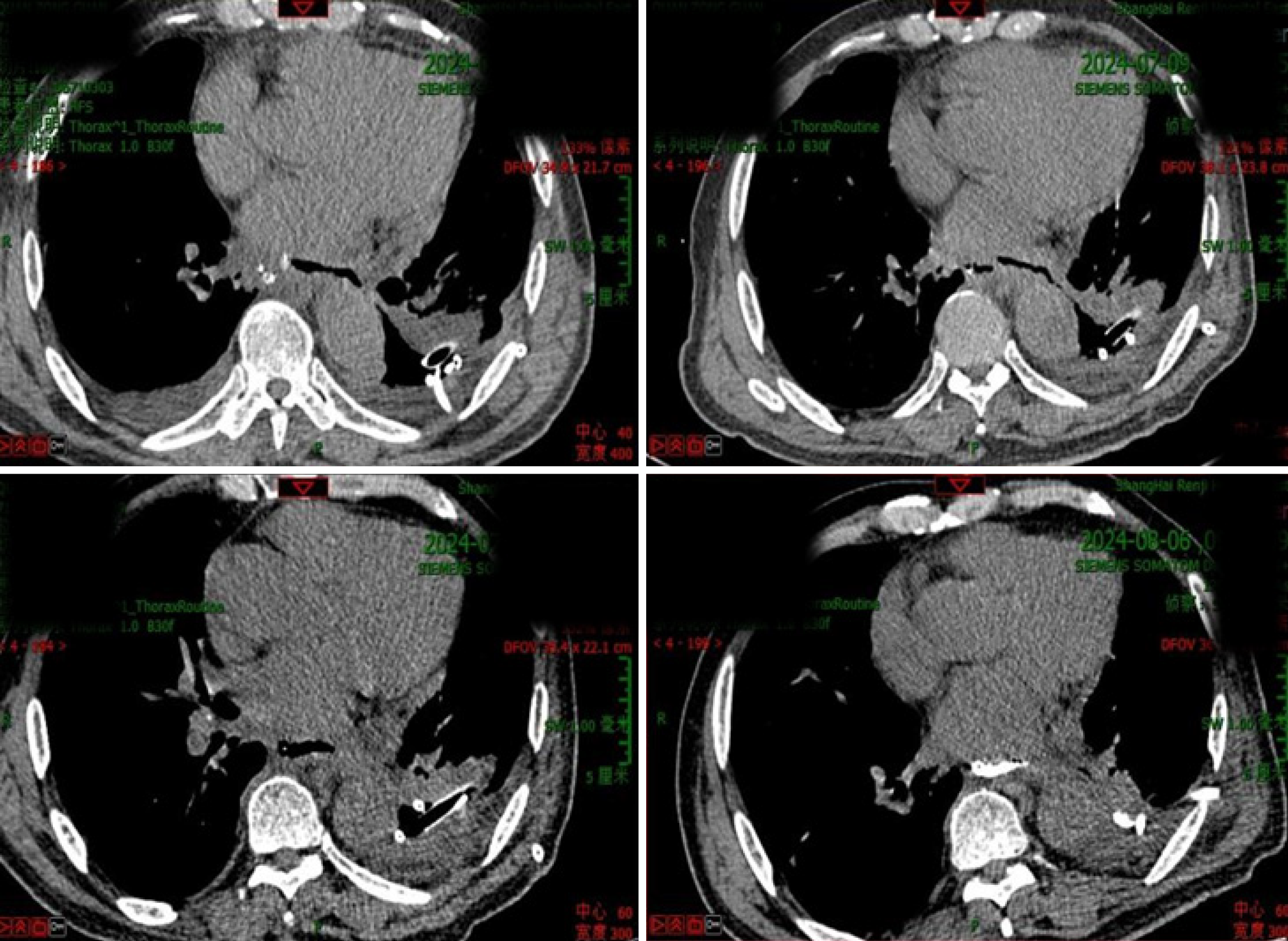
Contrast-enhanced CT scan showed a giant posterior mediastinal tumor with a fatty component (Figure 1A). The mass completely involved the esophagus and descending aorta. The heart and lower lobes of both lungs were deviated anteriorly by the tumor. Giant mass with variable proportions of fat, soft tissue, and myxoid tissue, these imaging features of the tumor were suggestive of well-differentiated liposarcoma. Positron emission tomography showed no dis
The final diagnosis for this patient was well-differentiated liposarcoma and esophageal fistula after surgery.
According to the inspection results, surgical resection was indicated. The biggest issue is determining the surgical approach. Enhanced magnetic resonance imaging of the chest showed the tumor completely involved the esophagus. However, there was still a small gap between the tumor and esophagus (Figure 1B). To avoid accidental damage to the esophagus, a nasogastric tube was placed before surgery.
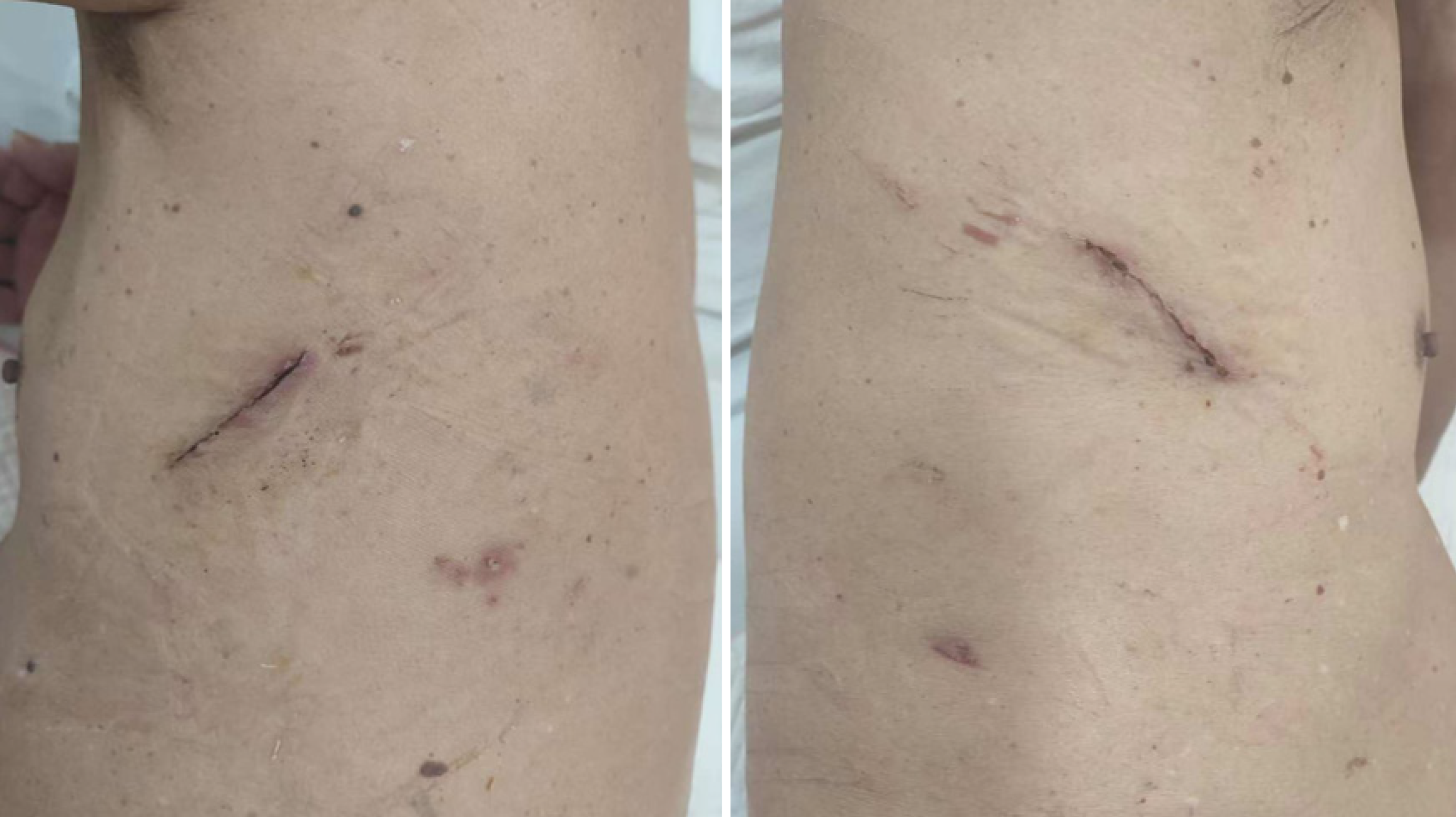
Given the unusual size and location of the tumor, a bilateral single-port VATS approach was selected. The size of the port was 40 mm. The patient was initially placed in the left lateral position, and the tumor in the right thoracic cavity was dissected by the single-port video-assisted thoracoscopic approach (Figure 2). The esophagus was peeled off from the tumor at the same time. Then, we turned the patient over, and the left tumor was also dissected by the single-port video-assisted thoracoscopic approach. The huge tumor was finally removed from the thoracic cavity piece by piece. A specimen bag was used to prevent tumor dissemination in the chest cavity. The tumor measured 30 cm × 19 cm × 5 cm.
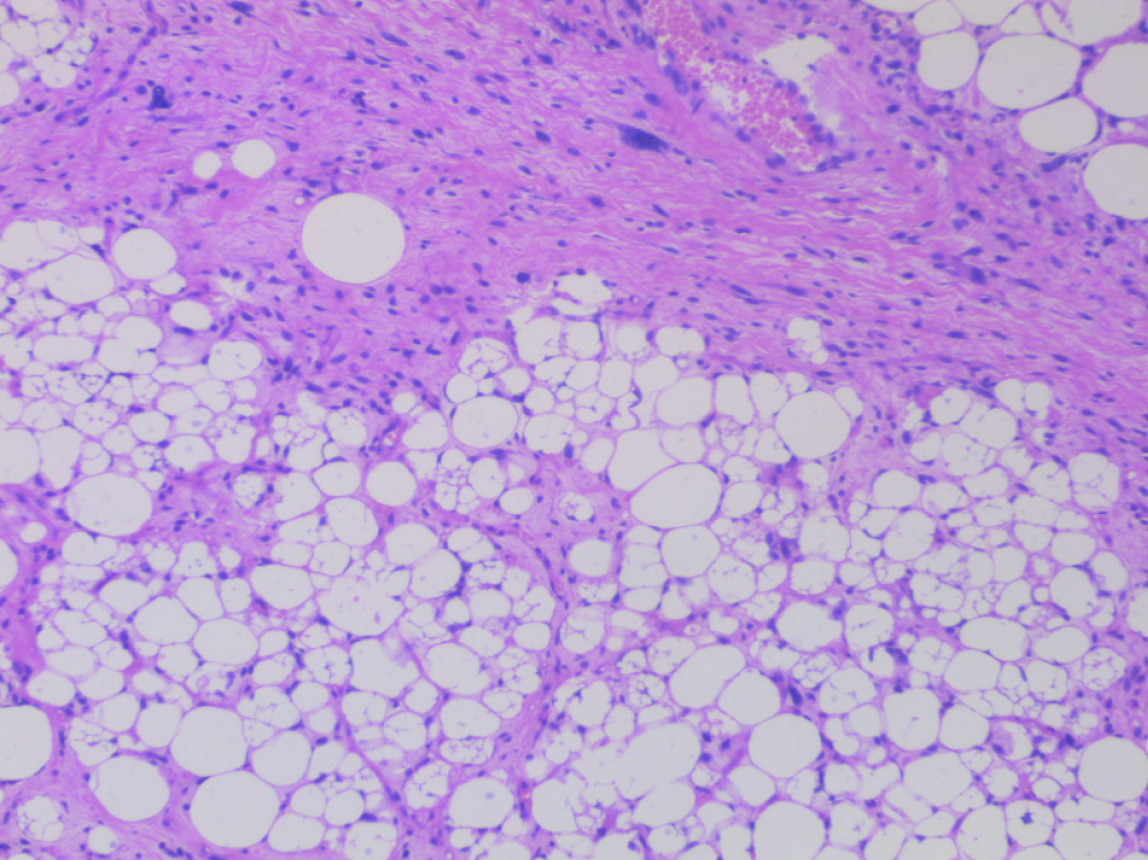
Pathological examination demonstrated well-differentiated liposarcoma, and Fluorescence in situ hybridization examination indicated amplification of murine double minute 2 (Figure 3).
The patient was fasting from solids and liquids during the first week after surgery. On the seventh day after surgery, the patient underwent a CT scan after taking iopamidol orally. The scan showed no leakage of contrast agent. Then, the patient started to eat liquid food.
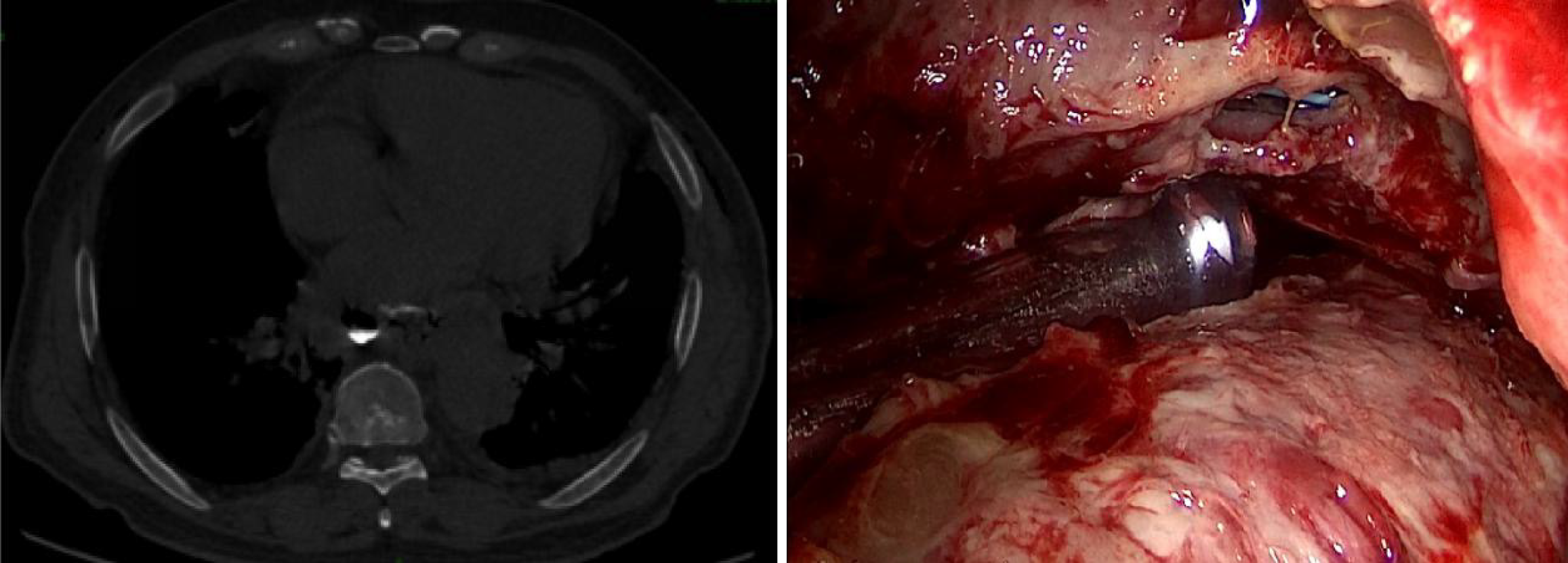
Unfortunately, an esophageal fistula combined with mediastinitis and empyema was detected 9 days after surgery and 2 days after eating. Emergency debridement surgery was performed with VATS using the same port of the first surgery, and a drainage tube was placed (Figure 4). After surgery, the patient was fasting from solids and liquids again and nut
Two months after the second surgery, gastroscopy was performed to confirm the fistula had totally healed, and the patient was discharged. Two weeks after the patient get home, he was able to eat normally. Six months after surgery, the patient underwent a CT scan, and there was no evidence of local recurrence.
Liposarcomas arising within the mediastinum are quite uncommon tumors, accounting for only about 0.1%-0.75% of mediastinal tumors[5,6]. The mean age of the patients was 52.6 ± 17.4 years reported in references and there was no sex predilection in these cases[6]. The World Health Organization histopathologic classification includes four distinct types of liposarcomas: Myxoid, well differentiated, dedifferentiated, and pleomorphic[4]. Although mediastinal liposarcoma is extremely rare, all four types can arise within the mediastinum[1].
ALT is the most common histologic sub-type of mediastinal liposarcoma, accounting for approximately 40% of all liposarcomas[9]. ALTs usually grow slowly and insidiously, and remain asymptomatic until reaching a huge size[2]. Berry et al[10] and Klimstra et al[11] reported that the average size of mediastinal liposarcomas is 15.7 cm, ranging from 6 cm to 40 cm, and the average weight is 1.5 kg. As liposarcoma is not sensitive to chemotherapy or radiotherapy, complete surgical resection using the standard median sternotomy or lateral thoracotomy is the most employed therapeutic choice[2,12]. Since the tumor is usually huge and compresses intrathoracic organs, such as the heart, great vessels, lungs, and esophagus[2], VATS is seldom reported as the treatment for mediastinal liposarcoma. In our case, the tumor was huge, occupied both sides of the chest cavity, and completely involved the esophagus. Minimally invasive surgery seemed impossible for this patient. However, according to enhanced chest magnetic resonance imaging, a small gap was still present between the tumor and esophagus. As VATS has a clear surgical field of view, we tried a bilateral single-port VATS approach, which has never been reported before. During the operation, the boundary between the tumor and the esophagus was clearly visible on the video, and the huge tumor was finally removed completely. The magnifying effect and clear surgical field of view seem to make VATS safer than thoracotomy.
Esophageal fistula after resection of a giant mediastinal tumor has not been reported in the literature before. As the tumor extensively involved the esophagus in the present case, measures were taken to prevent the occurrence of esophageal fistula. A nasogastric tube was placed before the first surgery, and the patient was fasting from solids and liquids during the first week after surgery. Before eating, the patient underwent a CT scan after taking iopamidol orally, and the scan showed no leakage of contrast agent. However, esophageal fistula still occurred after the patient ate. By reviewing the surgical video, we confirm that there was no direct damage to the esophageal wall during the surgery. We believe that the cause of the esophageal fistula was ischemia after peeling the esophagus from the tumor. Extensive periesophageal dissection, especially during resection of large, adherent tumors, can impair blood flow to the esophageal wall, leading to tissue necrosis and fistula formation. Fasting for a longer period may help prevent esophageal fistula.
Esophageal fistula after surgery is associated with high rates of mortality[13]. Thus, early identification and mana
To the best of our knowledge, this is the first report of bilateral single-port VATS for giant mediastinal liposarcoma, and the first report of esophageal fistula after this surgery. The magnifying effect and clear surgical field of view make VATS safer than thoracotomy. For tumors extensively involving the esophagus, fasting for a longer period may help prevent the occurrence of esophageal fistula. Early identification and management of esophageal fistula are very important. Surgical debridement, controlled drainage, nil per os and antibiotic therapy are the main treatments for esophageal fistula.
We are grateful to the patient for his agreement of publication of this report and accompanying images.
| 1. | den Bakker MA, Marx A, Mukai K, Ströbel P. Mesenchymal tumours of the mediastinum--part I. Virchows Arch. 2015;467:487-500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Chen C, Chen M, Liu W, Yuan Y, Yu F. Successful removal of giant mediastinal lipoma and liposarcoma involving both chest cavities: Two case reports. Medicine (Baltimore). 2018;97:e11806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Nguyen DC, Olatubosun O, Yu W, Loor G, Burt BM. Giant Mediastinal Liposarcoma: A Rare Yet Distinct Clinical Entity. Ann Thorac Surg. 2018;106:e117-e119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Coindre JM. [New WHO classification of tumours of soft tissue and bone]. Ann Pathol. 2012;32:S115-S116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Edagawa M, Haratake N, Shimamatsu S, Toyozawa R, Nosaki K, Hirai F, Yamaguchi M, Taguchi K, Kaneko K, Seto T, Takenoyama M, Ichinose Y. Surgical resection of a well-differentiated inflammatory liposarcoma of the middle mediastinum: a case report. J Thorac Dis. 2017;9:E689-E693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Rao J, Zhu Q, Yang X. Giant primary liposarcoma of the mediastinum: A case report and review of the literature. SAGE Open Med Case Rep. 2023;11:2050313X231206031. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Lee ATJ, Thway K, Huang PH, Jones RL. Clinical and Molecular Spectrum of Liposarcoma. J Clin Oncol. 2018;36:151-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 265] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 8. | Suzuki T, Sato T, Hasumi T. Resection of a giant mediastinal atypical lipomatous tumor involving the esophagus. J Surg Case Rep. 2021;2021:rjaa561. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Oh YJ, Yi SY, Kim KH, Cho YJ, Beum SH, Lee YH, Suh JS, Hur H, Kim KS, Kim SH, Choi YD, Shin KH, Jun HJ, Kim SJ, Lee J, Park SH, Noh SH, Rha SY, Kim HS. Prognostic Model to Predict Survival Outcome for Curatively Resected Liposarcoma: A Multi-Institutional Experience. J Cancer. 2016;7:1174-1180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Berry MF, Sporn TA, Moore JO, D'Amico TA. Giant thoracic liposarcoma treated with induction chemotherapy followed by surgical resection. J Thorac Oncol. 2009;4:768-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Klimstra DS, Moran CA, Perino G, Koss MN, Rosai J. Liposarcoma of the anterior mediastinum and thymus. A clinicopathologic study of 28 cases. Am J Surg Pathol. 1995;19:782-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 59] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Marulli G, Rea F, Feltracco P, Calabrese F, Giacometti C, Rizzardi G, Vincenzo L, Sartori F. Successful resection of a giant primary liposarcoma of the posterior mediastinum. J Thorac Oncol. 2007;2:453-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Turrentine FE, Denlinger CE, Simpson VB, Garwood RA, Guerlain S, Agrawal A, Friel CM, LaPar DJ, Stukenborg GJ, Jones RS. Morbidity, mortality, cost, and survival estimates of gastrointestinal anastomotic leaks. J Am Coll Surg. 2015;220:195-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 155] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 14. | Birla R, Hoara P, Dinu D, Rosianu C, Constantinoiu S. Postoperative Esophageal Leaks in Malignant Pathology - Optimal Management: A Systematic Review. Chirurgia (Bucur). 2019;114:429-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 15. | Freeman RK, Vyverberg A, Ascioti AJ. Esophageal stent placement for the treatment of acute intrathoracic anastomotic leak after esophagectomy. Ann Thorac Surg. 2011;92:204-8; discussion 208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/