Published online Nov 26, 2025. doi: 10.12998/wjcc.v13.i33.112241
Revised: July 25, 2025
Accepted: October 21, 2025
Published online: November 26, 2025
Processing time: 122 Days and 17 Hours
Thyroid nodules (TN) are increasingly diagnosed worldwide; investigating the association between TN and colon polyps could be helpful in early detection and management. To our knowledge no meta-analysis has assessed the relationship between TN and adenomatous colonic polyps.
To assess the association between adenomatous colonic polyps, thyroid-stimu
We searched PubMed, MEDLINE, Cochrane Library, EBSCO, and the first 100 articles in Google for articles published in English from inception until April 2025. We included prospective cohorts, retrospective studies, case-control studies, and cross-sectional studies. The keywords thyroid nodules, adenomatous colon pol
Out of 237 articles, 25 full texts were reviewed, and 5 full texts were included in the final meta-analysis. No relationship was found between TN, colonic polyps, and thyroid-stimulating hormone levels [odd ratio (OR): 1.78, 95% confidence interval (CI): 0.55-5.74, P = 0.33]. Colonic polyps were more common among patients with TN when addressing heterogeneity (OR: 0.42, 95%CI: 0.30-0.52, P < 0.001 and OR: 0.08, 95%CI: 0.70-0.86, P = 0.85).
TN were similar among patients with and without adenomatous colonic polyps. However, TN was more common among colon polyps when addressing the heterogeneity. Thyroid-stimulating hormone was not different between those with and without TN. Age, sex, adiposity, and smoking effects might explain the higher rate observed by the included studies. Further studies controlling for the same are needed.
Core Tip: Thyroid polyps are common among the middle age group, and colonoscopy is indicated in individuals older than 50 years. However, it is invasive, making easy reliable methods for risk stratification for colonic polyps screening important. The few studies that assessed the association of thyroid nodules and colon polyps showed contradicting results. The current meta-analysis contributed significantly to the field because it is the first meta-analysis to find an association. Our research challenges the current colonic polyp screening guidelines because physicians might need to include thyroid nodules as a risk factor for colonic polyps.
- Citation: Mirghani HO, Alghamdi S. Thyroid nodules as predictors of adenomatous colonic polyps: A systematic review and meta-analysis. World J Clin Cases 2025; 13(33): 112241
- URL: https://www.wjgnet.com/2307-8960/full/v13/i33/112241.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i33.112241
Thyroid nodules (TN) may be present in nearly two-thirds of the population depending on age. However, only 20% are clinically significant (cancer, pressure symptoms, and thyroid activity in 10%, 5%, and 5% respectively). TN are common, and thyroid cancer occurs in 7%-15% of patients with TN. Clinical examination, thyroid ultrasound, thyroid function tests, fine needle aspiration, and molecular testing are indicated for management and future planning[1,2]. Functioning TN are rarely malignant, but TN with normal or high thyroid-stimulating hormone (TSH) and suspicious ultrasound are candidates for fine needle aspiration. Indeterminate TN require molecular testing in the adult population. However, in children and pregnant females, their role is not validated[3].
The incidence of thyroid cancer is on the rise worldwide, and various environmental factors are to blame including iodine deficiency, vitamin D deficiency, increasing weight, and toxins exposure[4,5]. A case-control study showed the association between vitamin D deficiency and thyroid cancer[6]. Further studies concluded an association between vitamin D and thyroid disease[7-9]. On the other hand, Yildiz et al[10] and Laney et al[11] showed no association. Further studies showed the association between TSH, low vitamin D, and thyroid cancer[12,13].
Colorectal cancer is the third-leading cause of cancer-related deaths globally, and most cancers develop from polyps. The prevalence increases with age, and 12.9% suffered from polyps in a recent survey[14]. A study conducted in Asia found that nearly half were single polyps, and the majority were small and sessile[15]. Early detection of colonic polyps by colonoscopy was shown to reduce this common cancer mortality[16].
TN detection by ultrasonography might be a simple noninvasive measure to assess colonic polys risk and refer those at risk for screening. Given the above and the fact that colonic cancer develops in 5% of patients with colonic polyps[17], we conducted this meta-analysis to assess the relationship between colonic polyps and TN.
We searched PubMed, MEDLINE, Cochrane Library, EBSCO, and the first 100 articles in Google for articles published from inception until April 2025 with adherence to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines.
Prospective cohorts, retrospective studies, case-control studies, and cross-sectional studies assessing the relationship between TN and adenomatous colon polyps were included. Articles published on polyps other than adenomatous were excluded. In addition, case reports, series, opinions, editorials, poster presentations, and abstracts were not included.
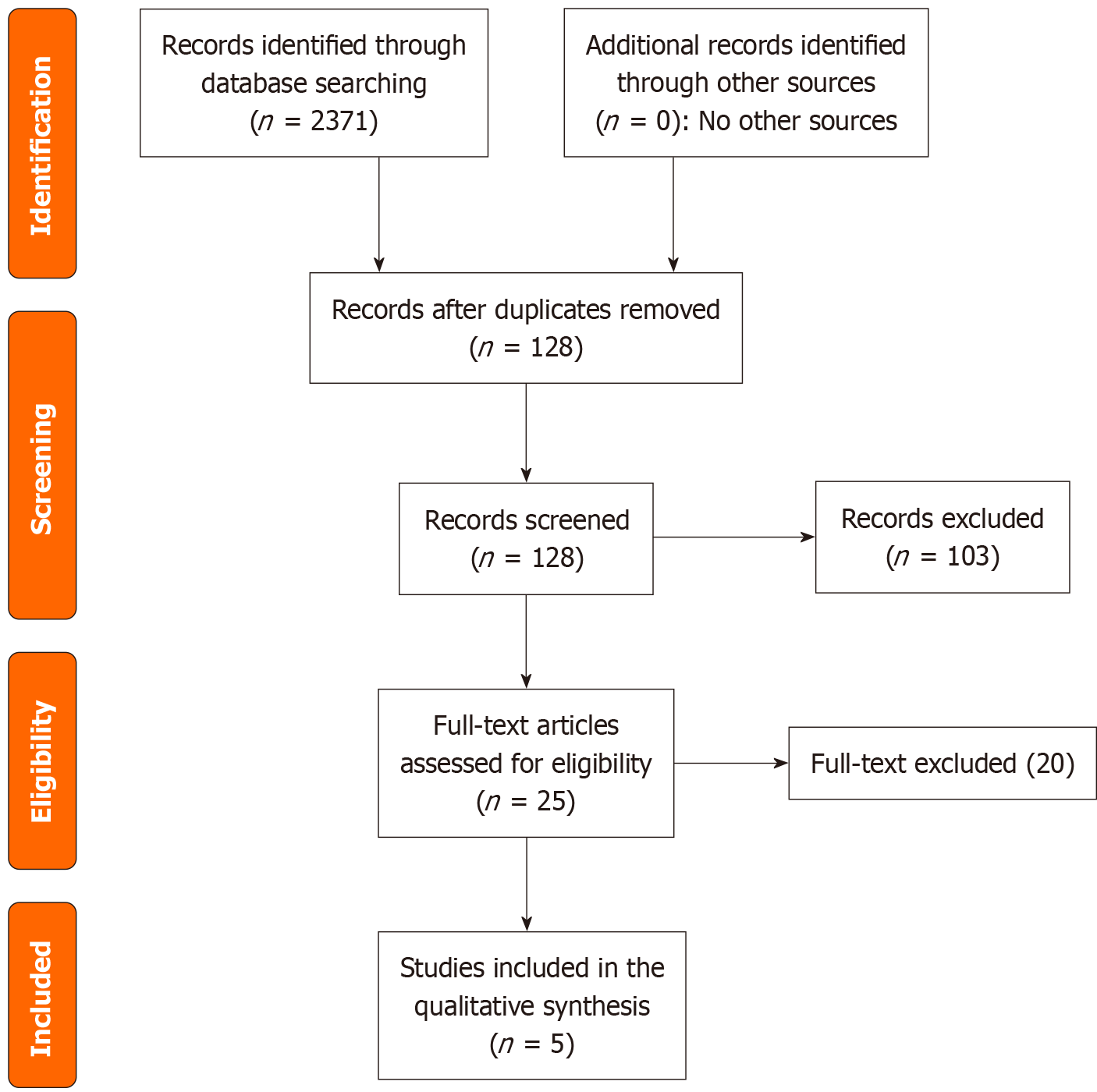
Two authors (Mirghani HO and Alghamdi S) systematically searched the literature for relevant articles that assessed the association of adenomatous colon polyps and TN. The title and abstracts were assessed in addition to their references. The keywords thyroid nodules, adenomatous colon polyps, thyroid volume, and thyroid malignancy were used. Two hundred and thirty-seven articles were eligible, and 128 remained after duplication removal. Of them 25 full texts were reviewed, and 5 full texts were included in the final meta-analysis.
The data were extracted to an Excel sheet detailing the first author’s name, country, study type, year of publication, TN and polyps in cases and control, age, female percentage, body mass index, waist circumference, smoking status, and TSH among patients with/without nodules. The text included three case-control, a prospective cohort, and one retrospective study (Figure 1, Tables 1, 2, and 3).
| Ref. | Country | Methodology | Polyps and nodules in cases | Polyps and nodules in controls | Results |
| Duran et al[19], 2012 | Türkiye | Case-control | 44/66 | 61/146 | More nodules in patients with polyps, P = 0.001 |
| Mousa et al[20], 2019 | United Kingdom | Case-control | 55/105 | 24/68 | More nodules in patients with polyps, P = 0.017 |
| Ozturk et al[21], 2022 | Türkiye | Retrospective | 15/20 | 36/103 | More nodules in patients with polyps, P < 0.03 |
| Park et al[22], 2015 | Korea | Prospective | 63/266 | 37/277 | No significant difference |
| Yu et al[23], 2021 | China | Case-control | 542/1379 | 1035/3135 | More nodules in patients with polyps, P < 0.001 |
| Ref. | Age | Females% | Obesity/BMI | Waist | Smoking |
| Duran et al[19], 2012 | 53.3 ± 11.4 vs 51.8 ± 11.4 | Matched | Not assessed | Not assessed | Not assessed |
| Mousa et al[20], 2019 | 54.48 ± 10.01 vs 51.87 ± 10. 86 | 47.3% vs 52.7% | 28.88 ± 7.66 vs 27.99 ± 4. 06 | 50.6% vs 49.4% high waist | Not assessed |
| Ozturk et al[21], 2022 | 61.95 ± 9.01 vs 57.13 ± 14.49 | 35% vs 69 67% | Not assessed | Not assessed | Not assessed |
| Park et al[22], 2015 | 52.08 ± 11.48 vs 47.02 ± 9.26 | 36.5% vs 55.6% | 37.2% vs 27.1% | 83.56 ± 9.16 vs 80.20 ± 9.07 | 16.5% vs 10.5% |
| Yu et al[23], 2021 | 50 vs 45 | 25.1% vs 43.6% | 24.5 vs 23.3% | 3.24 ± 9.58 | 39.3% vs 23.5% |
The quality of the included studies was assessed using the Newcastle Ottawa Scale[18] (Table 4).
The RevMan system, version 5.4 was used for data analysis. The data were dichotomous and entered manually. Forest plots were generated, and the effect size was estimated as odds ratio (OR) and 95% confidence interval (CI). The random effect model was used due to the significant heterogeneity observed (heterogeneity < 25 was considered mild, and heterogeneity ≥ 50 was considered significant). A P value of 0.05 was considered significant.
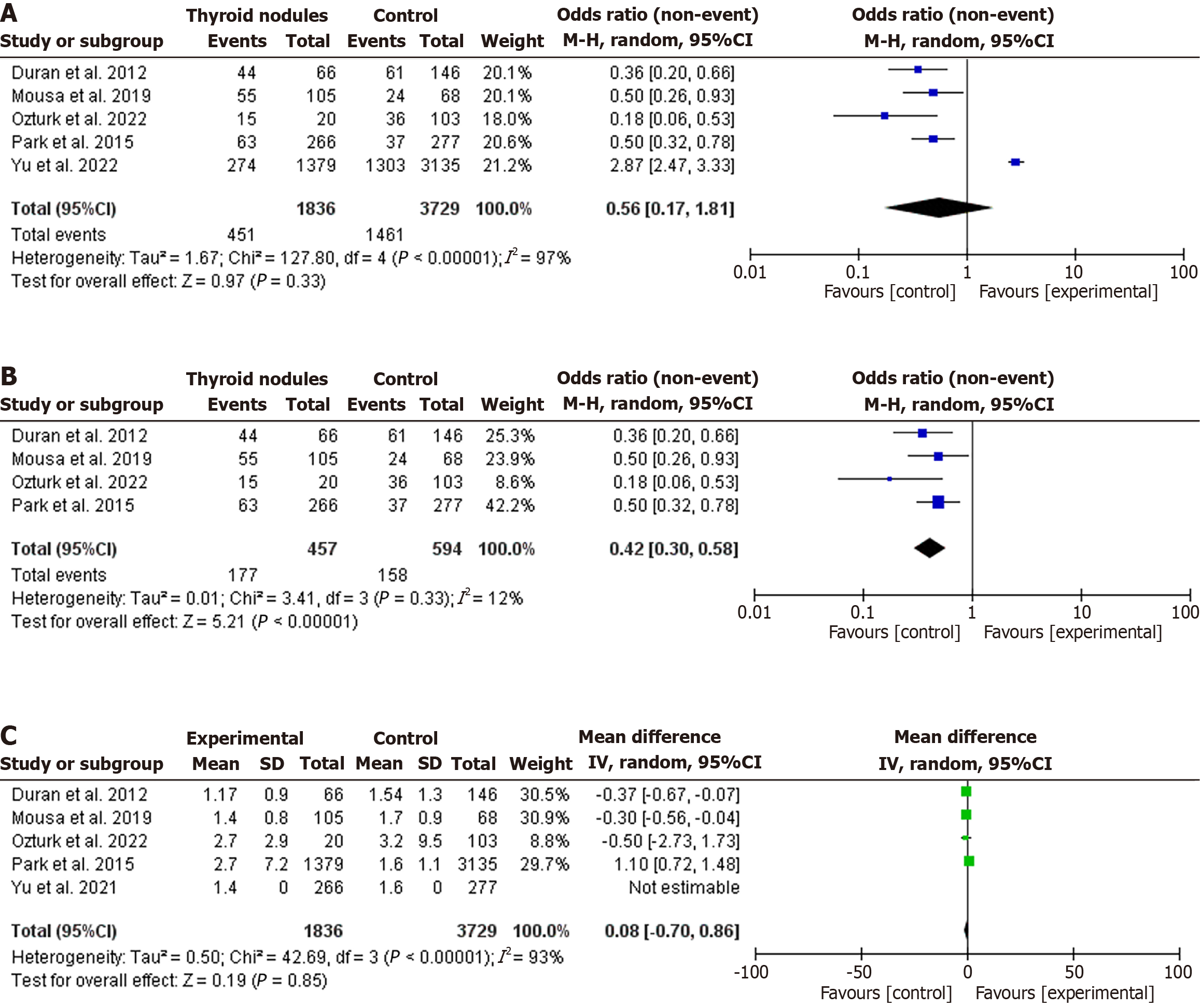
The current meta-analysis included three case-control studies, one prospective study, and one retrospective cohort (four from Asia and one from Europe). The studies included 1912 events among 5565 patients[19-23]. No relationship was found between TN and colonic polyps (OR: 1.78, 95%CI: 0.55-5.74, P = 0.33). However, significant heterogeneity was observed (I2 = 97%, P < 0.001) (Figure 2A). However, after removing one study to eliminate heterogeneity, colonic polyps were more common among patients with TN (OR: 0.42, 95%CI: 0.30-0.52, P < 0.001, I2 = 12%, P for heterogeneity = 0.33) (Figure 2B).
TSH levels were not different between patients with and without TN (OR: 0.08, 95%CI: 0.70-0.86, P = 0.85). However, substantial heterogeneity was found (I2 = 93%, P < 0.001) (Figure 2C).
Literature on the link between TN and colonic polyps is scarce. Common risk factors for these two common disorders are age, male sex, and metabolic risk factors[24]. In the present study TN incidence was similar among patients with and without adenomatous colon polyps (OR: 1.78, 95%CI: 0.55-5.74, P = 0.33). However, after removing the heterogeneous study, the relationship became positive (OR: 0.42, 95%CI: 0.30-0.52, and P < 0.001). TSH levels were not different between those with and without TN (OR: 0.08, 95%CI: 0.70-0.86, P = 0.85).
The first study to observe the association of colonic polyps and TN was published by Duran et al[19]. They did not assess body mass index, waist circumference, and smoking, limiting the study. TN were found to be associated with obesity and diabetes[25]. Similarly, the higher rate of TN among patients with adenomatous colonic polyps observed by Mousa et al[20] might be explained by the higher age, male sex, and body mass index (Table 2). High insulin, glucose-dependent insulinotropic peptide, and Insulin-like growth factor 1 (IGF-1) levels are also suggested to mediate the association[26,27]. The results of Park et al[22] included in this study were limited by the older age, male, body mass index, and smoking among patients with colonic polyps. In addition, higher smoking among the colonic polyp arm might bias the results of Yu and Wu[23]. The above observations imply that the higher TN among patients with colonic polyps might be due to various confounding variables (age, male sex, obesity, and smoking status).
The role of the TSH on thyroid growth is conflicting with some showing a positive relationship[28,29] and others failing to show any association[30,31]. In the current meta-analysis TSH levels were not different between patients with and without TN, similar to Layegh et al[32], who conducted a study among patients with obesity and normal body mass index and found no difference in TSH levels among patients with and without TN.
Two out of the five studies included in this analysis reported a higher prevalence of smoking among patients with TN[23,23]. Higher smoking among the TN arm might greatly influence the results[33,34].
Limitations of this study must be acknowledged. The small number of included studies and the observational methodology limited our study. High heterogeneity was also observed.
TN were similar among patients with and without adenomatous colonic polyps. TSH levels were not different between those with and without TN. Age, sex, adiposity, and smoking effects might explain the higher rate observed by the included studies. Further studies controlling for the same are needed.
| 1. | Durante C, Grani G, Lamartina L, Filetti S, Mandel SJ, Cooper DS. The Diagnosis and Management of Thyroid Nodules: A Review. JAMA. 2018;319:914-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 527] [Article Influence: 65.9] [Reference Citation Analysis (2)] |
| 2. | Wong R, Farrell SG, Grossmann M. Thyroid nodules: diagnosis and management. Med J Aust. 2018;209:92-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 117] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 3. | Kant R, Davis A, Verma V. Thyroid Nodules: Advances in Evaluation and Management. Am Fam Physician. 2020;102:298-304. [PubMed] |
| 4. | Fan J, Fu S, Chen X, Li Y, Zhao Y, Lv F, Yao Y. Thyroid nodules and its association with vitamin D in centenarians. Exp Gerontol. 2022;161:111730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 5. | Barrea L, Gallo M, Ruggeri RM, Giacinto PD, Sesti F, Prinzi N, Adinolfi V, Barucca V, Renzelli V, Muscogiuri G, Colao A, Baldelli R; E. O.L.O. Group. Nutritional status and follicular-derived thyroid cancer: An update. Crit Rev Food Sci Nutr. 2021;61:25-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 6. | Heidari Z, Nikbakht M, Mashhadi MA, Jahantigh M, Mansournia N, Sheikhi V, Mansournia MA. Vitamin D Deficiency Associated with Differentiated Thyroid Carcinoma: A Case- Control Study. Asian Pac J Cancer Prev. 2017;18:3419-3422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 7. | Bener A, Ozdenkaya Y, Al-Hamaq AOAA, Barisik CC, Ozturk M. Low Vitamin D Deficiency Associated With Thyroid Disease Among Type 2 Diabetic Mellitus Patients. J Clin Med Res. 2018;10:707-714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Sulibhavi A, Rohlfing ML, Jalisi SM, McAneny DB, Doherty GM, Holick MF, Noordzij JP. Vitamin D deficiency and its relationship to cancer stage in patients who underwent thyroidectomy for papillary thyroid carcinoma. Am J Otolaryngol. 2019;40:536-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Li H, Jin X, Zhang M, Wang X, Wang H. Differential expression of cytokines and vitamin D in benign and malignant thyroid diseases. Sci Rep. 2025;15:23493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Yildiz S, Ekinci O, Ucler R. The relationship between 25 hydroxy Vitamin D3 and thyroid antibodies with thyroid benign-malign neoplasms. Niger J Clin Pract. 2019;22:1224-1228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Laney N, Meza J, Lyden E, Erickson J, Treude K, Goldner W. The Prevalence of Vitamin D Deficiency Is Similar between Thyroid Nodule and Thyroid Cancer Patients. Int J Endocrinol. 2010;2010:805716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Danilovic DL, Ferraz-de-Souza B, Fabri AW, Santana NO, Kulcsar MA, Cernea CR, Marui S, Hoff AO. 25-Hydroxyvitamin D and TSH as Risk Factors or Prognostic Markers in Thyroid Carcinoma. PLoS One. 2016;11:e0164550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Zhang Q, Wang Z, Sun M, Cao M, Zhu Z, Fu Q, Gao Y, Mao J, Li Y, Shi Y, Yang F, Zheng S, Tang W, Duan Y, Huang X, He W, Yang T. Association of high vitamin d status with low circulating thyroid-stimulating hormone independent of thyroid hormone levels in middle-aged and elderly males. Int J Endocrinol. 2014;2014:631819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Koirala D, Pathak R, Kafle Bhandari B, Jha A, Hamal R, Gnawali A, Pandey R, Bhusal M. Detection of Colonic Polyps During Colonoscopy in a Tertiary Care Center of Nepal. J Nepal Health Res Counc. 2021;19:596-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Qari YA. Clinicopathological characterization of colonic polyps. Niger J Clin Pract. 2020;23:1048-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Azer SA. Challenges Facing the Detection of Colonic Polyps: What Can Deep Learning Do? Medicina (Kaunas). 2019;55:473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Safiyeva AK, Bayramov NY. The importance of colonoscopy in the treatment of colorectal polyps and colorectal cancer screening. Ann Ital Chir. 2019;90:311-317. [PubMed] |
| 18. | Stang A, Jonas S, Poole C. Case study in major quotation errors: a critical commentary on the Newcastle-Ottawa scale. Eur J Epidemiol. 2018;33:1025-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 19. | Duran C, Gokturk HS, Kulaksizoglu M, Bakdik S, Unler GK, Erbayrak M, Ozkaya G, Pamuk BO, Gonen MS. Frequency of Thyroid Nodules among Patients with Colonic Polyps. Gastroenterol Res Pract. 2012;2012:178570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Mousa U, Anil C, Demir CC, Bozkus Y, Ozturk K, Bascil Tutuncu N, Gursoy A. Thyroid Nodules Are More Prevalent in Subjects with Colon Polyps, Independent of Insulin Resistance. Med Princ Pract. 2019;28:418-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 21. | Ozturk M, Avci E. The prevalence of colon polyps in patients with thyroid nodules. Acta Medica Mediterr. 2022;38:653-655. [DOI] [Full Text] |
| 22. | Park CW, Kim EK, Yun YB, Ryu BS, Park JH, Ko J, Seo HW. The correlation between thyroid nodules and the incidence rate of colonic polyps based on body mass index. Korean J Fam Pract. 2015;5:354-360. |
| 23. | Yu Y, Wu J. Presence of Metabolic Syndrome and Thyroid Nodules in Subjects with Colorectal Polyps. Med Sci Monit. 2021;27:e927935. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 24. | Lai X, Ouyang P, Zhu H, An S, Xia L, Yao Y, Zhang H, Li Z, Deng K. [Detection rate of thyroid nodules in routine health check-up and its influencing factors: a 10-year survey of 309 576 cases]. Nan Fang Yi Ke Da Xue Xue Bao. 2020;40:268-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 25. | Buscemi S, Massenti FM, Vasto S, Galvano F, Buscemi C, Corleo D, Barile AM, Rosafio G, Rini N, Giordano C. Association of obesity and diabetes with thyroid nodules. Endocrine. 2018;60:339-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 26. | Soubry A, Il'yasova D, Sedjo R, Wang F, Byers T, Rosen C, Yashin A, Ukraintseva S, Haffner S, D'Agostino R Jr. Increase in circulating levels of IGF-1 and IGF-1/IGFBP-3 molar ratio over a decade is associated with colorectal adenomatous polyps. Int J Cancer. 2012;131:512-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 27. | Sasaki Y, Takeda H, Sato T, Orii T, Fujishima S, Nagino K, Nishise S, Saito H, Tanaka Y, Kawata S. Increased levels of serum glucose-dependent insulinotropic polypeptide as a novel risk factor for human colorectal adenoma. Metabolism. 2011;60:1253-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Duran AO, Anil C, Gursoy A, Nar A, Inanc M, Bozkurt O, Tutuncu NB. Thyroid volume in patients with glucose metabolism disorders. Arq Bras Endocrinol Metabol. 2014;58:824-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Ertek S, Cicero AF, Caglar O, Erdogan G. Relationship between serum zinc levels, thyroid hormones and thyroid volume following successful iodine supplementation. Hormones (Athens). 2010;9:263-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 30. | Sousa PA, Vaisman M, Carneiro JR, Guimarães L, Freitas H, Pinheiro MF, Liechocki S, Monteiro CM, Teixeira Pde F. Prevalence of goiter and thyroid nodular disease in patients with class III obesity. Arq Bras Endocrinol Metabol. 2013;57:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 31. | Dauksiene D, Petkeviciene J, Klumbiene J, Verkauskiene R, Vainikonyte-Kristapone J, Seibokaite A, Ceponis J, Sidlauskas V, Daugintyte-Petrusiene L, Norkus A, Zilaitiene B. Factors Associated with the Prevalence of Thyroid Nodules and Goiter in Middle-Aged Euthyroid Subjects. Int J Endocrinol. 2017;2017:8401518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 32. | Layegh P, Asadi A, Jangjoo A, Layegh P, Nematy M, Salehi M, Shamsian A, Ranjbar G. "Comparison of thyroid volume, TSH, free t4 and the prevalence of thyroid nodules in obese and non-obese subjects and correlation of these parameters with insulin resistance status". Caspian J Intern Med. 2020;11:278-282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 33. | Aydin LY, Aydin Y, Besir FH, Demirin H, Yildirim H, Önder E, Dumlu T, Celbek G. Effect of smoking intensity on thyroid volume, thyroid nodularity and thyroid function: the Melen study. Minerva Endocrinol. 2011;36:273-280. [PubMed] |
| 34. | Jiang H, Tian Y, Yan W, Kong Y, Wang H, Wang A, Dou J, Liang P, Mu Y. The Prevalence of Thyroid Nodules and an Analysis of Related Lifestyle Factors in Beijing Communities. Int J Environ Res Public Health. 2016;13:442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 100] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/