Published online Nov 26, 2025. doi: 10.12998/wjcc.v13.i33.112160
Revised: August 16, 2025
Accepted: October 23, 2025
Published online: November 26, 2025
Processing time: 125 Days and 12.7 Hours
Pelvic squamous cell carcinoma of unknown primary (CUP) is extremely rare, accounting for less than one percent of all CUP cases, and its infrequency has lim
A 77-year-old female with a history of resected lung adenocarcinoma presented with worsening constipation. Imaging revealed a 2.5 cm mass adjacent to the right levator ani muscle. Biopsy confirmed poorly differentiated squamous cell carcinoma, positive for pancytokeratin and p40, and negative for p16, cytokeratin 7, cytokeratin 20, and neuroendocrine markers. No primary lesion was identified despite extensive evaluation. She underwent five cycles of 5-fluorouracil (1000 mg/m2 continuous infusion, days 1-4) and mitomycin-C (10 mg/m2 on day 1) with concurrent pelvic radiotherapy (50.4 Gy in 28 fractions). Follow-up imaging demonstrated complete remission sustained for 12 months. Electrocorticography performance status improved from 2 at diagnosis to 1 during follow-up.
This case highlights the potential role of chemoradiotherapy in managing pelvic squamous cell CUP, achieving durable remission in selected patients.
Core Tip: This case report describes an elderly woman with pelvic squamous cell carcinoma of unknown primary (CUP), an entity accounting for less than 1% of CUP cases. A comprehensive diagnostic workup ruled out common primaries, and multidisciplinary evaluation led to chemoradiotherapy with 5-fluorouracil and mitomycin-C plus radiotherapy. The patient achieved complete remission for 12 months with improved functional status. This report emphasizes the value of imaging, pathology, and individualized multidisciplinary management in achieving durable remission in rare pelvic squamous CUP.
- Citation: Gupta AK, Polavarapu H. Squamous cell carcinoma of unknown primary in the pelvis after complete remission following chemoradiotherapy: A case report. World J Clin Cases 2025; 13(33): 112160
- URL: https://www.wjgnet.com/2307-8960/full/v13/i33/112160.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i33.112160
Carcinoma of unknown primary (CUP) refers to metastatic malignancy without an identifiable primary despite extensive evaluation[1]. CUP constitutes about 2% of all cancers, with squamous histology representing fewer than 5%[1,2]. Within this group, pelvic CUP is exceedingly rare, accounting for less than 1% of cases[3,4]. The rarity is highlighted by popu
A 77-year-old woman presented with gradually worsening constipation over six months.
The constipation was not accompanied by rectal bleeding, prolapse, or other pelvic symptoms. Symptoms progressively worsened, prompting further evaluation.
The patient had no significant medical history other than a previously resected and curatively treated lung cancer. She had no known history of HPV or Epstein-Barr virus infections.
No relevant personal or family medical history was reported.
General physical examination, including perineal and abdominal assessment, was unremarkable. Digital rectal examination during colonoscopy identified a firm, lobulated mass in the right perirectal area with mobile overlying mucosa showing no obvious abnormalities.
Complete blood count, basic metabolic panel, and comprehensive metabolic profile were within normal limits.
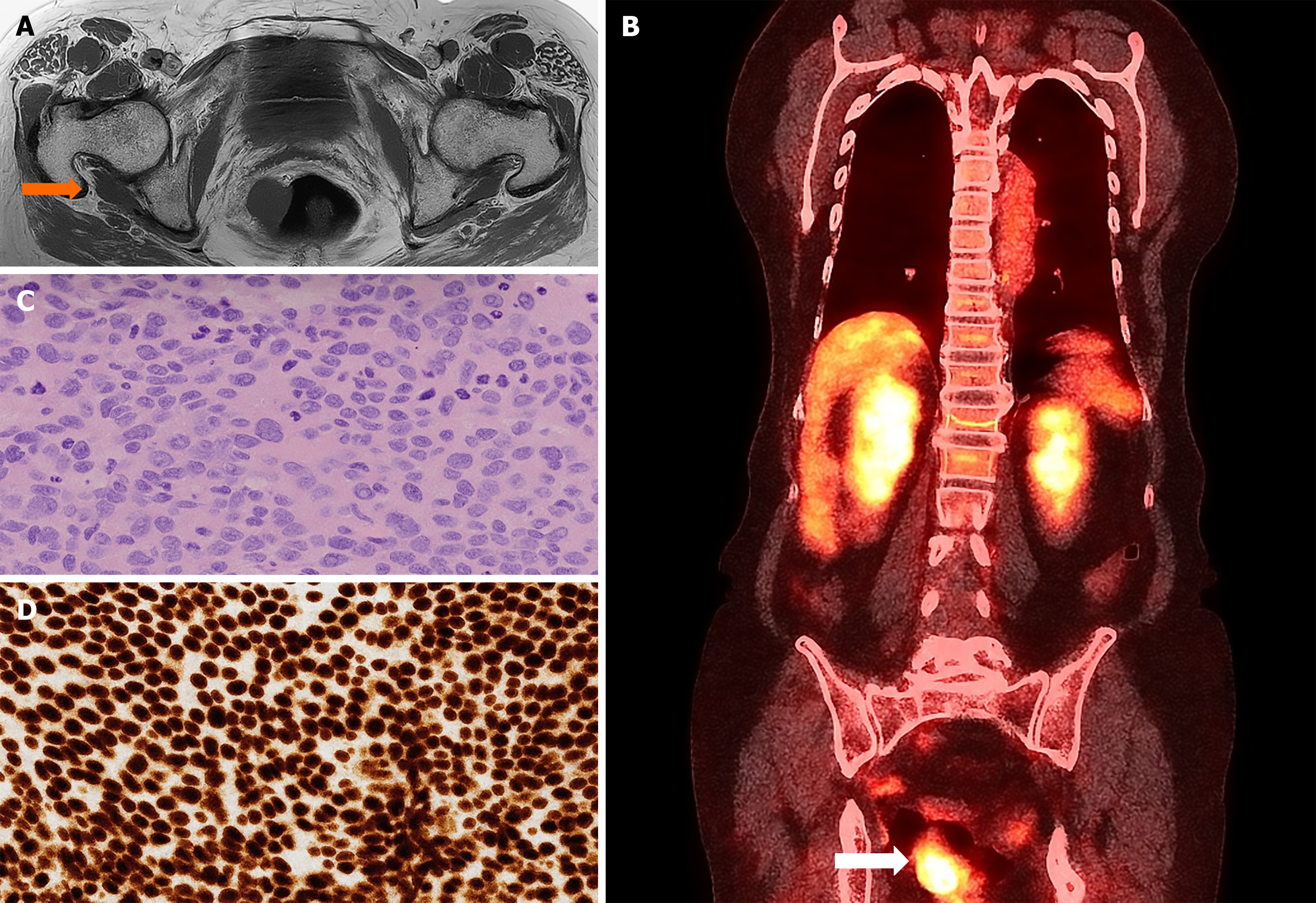
Colonoscopy revealed a tubular adenoma in the transverse colon. Computed tomography (CT) and magnetic resonance imaging demonstrated a 2.5 cm × 2.4 cm × 2.5 cm mass adjacent to the right levator ani muscle and vaginal cuff (Figure 1A). A whole-body positron emission tomography/CT scan revealed a solitary fluorodeoxyglucose-avid lesion confined to the right pelvic region, near the rectum and vagina (Figure 1B). Histopathology and immunohistochemistry: CT-guided biopsy confirmed poorly differentiated squamous cell carcinoma. Immunohistochemistry was positive for pancytokeratin and p40, and negative for p16, cytokeratin 7 and 20, GATA binding protein 3, and neuroendocrine markers (synaptophysin) (Figure 1C and D). These findings were inconsistent with the previously resected lung carcinoma.
The case was reviewed in a multidisciplinary tumor board involving radiation oncology, medical oncology, and radiology, and a consensus decision for chemoradiotherapy was made.
Pelvic squamous cell CUP.
The patient was treated with five cycles of 5-fluorouracil and mitomycin-C combined with concurrent pelvic radio
The patient tolerated the regimen well. Follow-up imaging at 6 months and 1 year confirmed complete resolution of the lesion without recurrence. The patient maintained good functional status throughout follow-up.
CUP of the pelvis implies the presence of cancer in the pelvis; however, the primary site of origin of the cancer is not known, and it is present in rare instances[1,6]. CUP origin, particularly squamous cell carcinoma, is typically found in the head and neck region or the inguinal region, although it can occasionally occur in the pelvis[6,8]. This type of cancer can have various cellular origins, including adenocarcinoma, squamous cell carcinoma, neuroendocrine tumors, lymphoma, melanoma, germ cell tumors, and more[1,6,8,9]. A biopsy and pathological evaluation usually gives an idea about the nature of the tumor, prompting further evaluation and investigation to look for the primary. The architecture associated with the immunohistochemistry helps identify the nature of the tumor[1,10]. The patient described in this case report has squamous cell cancer. Squamous cell cancer of the pelvis and an unknown primary site is known to be associated with HPV infection[11]. A thorough evaluation to identify the primary site has to be done by clinical evaluation of the anal and genital regions[12]. There are no standardized guidelines for evaluating an unknown primary in the pelvis; however, most authors utilize a workup similar to that for evaluating CUP presenting in the inguinal lymph nodes[13-15].
Limited case reports that have been published for CUP of squamous cell origin in the pelvis are known to have a higher association with HPV infection. HPV virus infection is most likely of anal-genital origin[16]. p16 expression results from the activation of tumor genes such as p53 and retinoblastoma protein by HPV infection[17]. In this patient, there was no lesion or induration to suggest a lesion in the anal and genital region. However, other limited case reports that have represented similar findings have had HPV-positive lesions[15-17]. Ovarian tumors can also occasionally present with squamous cell features[18]; however, the location and normal ovaries on imaging ruled that out in the patient.
There is limited data regarding the management and therapies for cisplatin, nivolumab, surgery, or chemoradiotherapy. However, no standardized guidelines have been established, given the rarity of this presentation[19-21]. Surgical resection has been reported to play a role; however, location, age, and morbidity of the surgery can be limiting factors[22]. Since the patient responded well to chemoradiotherapy, surgery was not considered in subsequent follow-up. The limited case reports which have been presented show a positive response to radiotherapy, as in our case.
Squamous cell CUP in the pelvis is an exceedingly rare condition with limited literature and no established treatment guidelines. A thorough and systematic diagnostic evaluation is essential. Our case illustrates that chemoradiotherapy may offer an effective and non-invasive treatment option in appropriately selected patients.
| 1. | Varadhachary GR. Carcinoma of unknown primary origin. Gastrointest Cancer Res. 2007;1:229-235. [PubMed] |
| 2. | Rassy E, Assi T, Pavlidis N. Exploring the biological hallmarks of cancer of unknown primary: where do we stand today? Br J Cancer. 2020;122:1124-1132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Califano J, Westra WH, Koch W, Meininger G, Reed A, Yip L, Boyle JO, Lonardo F, Sidransky D. Unknown primary head and neck squamous cell carcinoma: molecular identification of the site of origin. J Natl Cancer Inst. 1999;91:599-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 91] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Chiec L, Verma S, Kendler A, Abdel Karim N. Male pelvic squamous cell carcinoma of unknown primary origin. Case Rep Oncol Med. 2014;2014:953698. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Matylevich OP, Kurchankou MA, Kopsсhaj PA, Schmeler KM. HPV-related metastatic retroperitoneal pelvic squamous cell carcinoma of unknown primary origin in a patient previously treated for endometrial cancer. Int J Surg Case Rep. 2024;118:109624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Meng W, Gao Y, Pan L, Zhao G, Chen Q, Bai L, Zheng R. Pelvic squamous cell carcinoma of unknown primary origin with hydronephrosis and ureteral stricture: A case report. Medicine (Baltimore). 2024;103:e37057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Fizazi K, Greco FA, Pavlidis N, Daugaard G, Oien K, Pentheroudakis G; ESMO Guidelines Committee. Cancers of unknown primary site: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26 Suppl 5:v133-v138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 225] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 8. | Yan N, Zhang Y, Guo X, Yuan D, Tian G, Yang J. A Review on Cancer of Unknown Primary Origin: The Role of Molecular Biomarkers in the Identification of Unknown Primary Origin. Methods Mol Biol. 2020;2204:109-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Koge H, Hino A, Kakiuchi A, Yamamoto Y, Kanbe A, Kojima D, Horikawa A, Doiuchi T, Kurihara H. A case of pelvic squamous cell carcinoma of unknown primary origin that responded well to radiotherapy and nivolumab. Radiol Case Rep. 2024;19:1881-1885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Oien KA, Dennis JL. Diagnostic work-up of carcinoma of unknown primary: from immunohistochemistry to molecular profiling. Ann Oncol. 2012;23 Suppl 10:x271-x277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Dau GE, Brennan AK, Teschan NJ, Taylor JS, Winkler SS. A Curious Presentation of a Human Papillomavirus (HPV)-Driven Pelvic Squamous Cell Carcinoma of Unknown Primary: A Case Report. Cureus. 2025;17:e82134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Balci Topuz B, Seyyar M, Ozturk Iyilikci M, Ertunc G, Yumuk E, Uzun E. Aggressive Squamous Cell Carcinoma of Unknown Primary: Isolated Inguinal Metastasis and Uncommon Progression. Am J Case Rep. 2025;26:e946689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Pansari M, Lodin D, Gupta AK, Genuit T, Moseson J. Rare Case of a Transverse Colon Schwannoma. Cureus. 2020;12:e7604. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Gupta AK, Vazquez OA. Fallopian Tube Tumor Mimicking Primary Gastrointestinal Malignancy. Cureus. 2020;12:e9795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Zhu QZ, Li HJ, Li YQ, Yu XH, Shu KY. Pelvic metastatic squamous cell carcinoma of unknown primary site: A case report and brief literature review. Medicine (Baltimore). 2023;102:e36796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Isbell A, Fields EC. Three cases of women with HPV-related squamous cell carcinoma of unknown primary in the pelvis and retroperitoneum: A case series. Gynecol Oncol Rep. 2016;16:5-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | da Mata S, Ferreira J, Nicolás I, Esteves S, Esteves G, Lérias S, Silva F, Saco A, Cochicho D, Cunha M, Del Pino M, Ordi J, Félix A. P16 and HPV Genotype Significance in HPV-Associated Cervical Cancer-A Large Cohort of Two Tertiary Referral Centers. Int J Mol Sci. 2021;22:2294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 18. | Abid Z, Fatima M, Zehra D, Abid M, Khan SA. Primary Squamous Cell Carcinoma of the Ovary. Cureus. 2019;11:e5884. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Work Group; Invited Reviewers, Kim JYS, Kozlow JH, Mittal B, Moyer J, Olenecki T, Rodgers P. Guidelines of care for the management of cutaneous squamous cell carcinoma. J Am Acad Dermatol. 2018;78:560-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 343] [Article Influence: 42.9] [Reference Citation Analysis (0)] |
| 20. | Gupta AK, Vazquez OA, Lopez-Viego M. Pelvic Rectal Stercoral Perforation Resulting in Diffuse Pneumatosis. Cureus. 2020;12:e9146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 21. | Komura A, Taguchi A, Ikemura M, Nishijima A, Miyamoto Y, Tanikawa M, Sone K, Mori M, Oda K, Osuga Y. A case of refractory pelvic squamous cell carcinoma of unknown primary that responded to nivolumab. J Obstet Gynaecol Res. 2023;49:1300-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 22. | Shine RJ, Glyn T, Frizelle F. Pelvic exenteration: a review of current issues/controversies. ANZ J Surg. 2022;92:2822-2828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/