©The Author(s) 2025.
World J Clin Oncol. Dec 24, 2025; 16(12): 112443
Published online Dec 24, 2025. doi: 10.5306/wjco.v16.i12.112443
Published online Dec 24, 2025. doi: 10.5306/wjco.v16.i12.112443
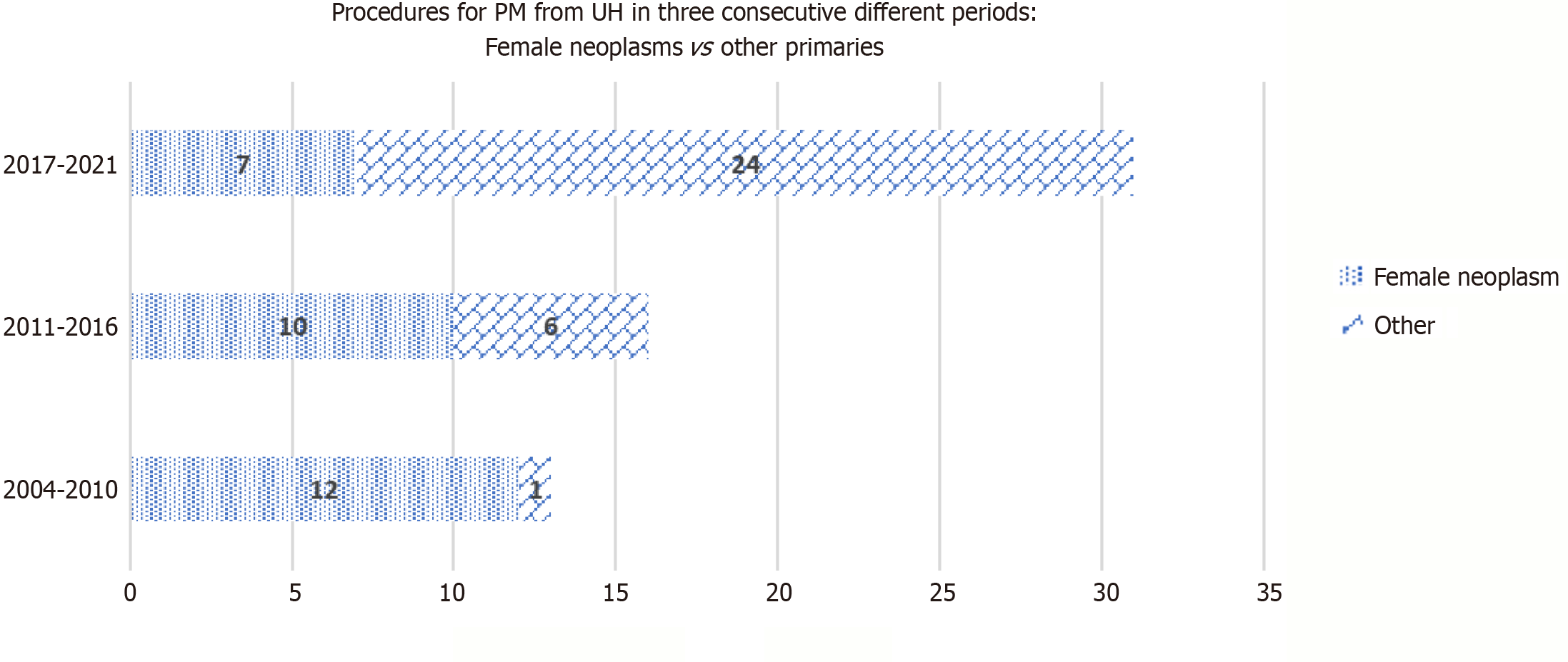
Figure 1 Distribution of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy procedures performed for peritoneal metastases from uncommon histologies across three consecutive periods (2004-2010, 2011-2016, 2017-2021), stratified by tumor origin.
Female neoplasms (breast and uterine cancer) were more common in earlier years, whereas procedures for other primary tumors increased over time. PM: Peritoneal metastases; UH: Uncommon histologies.
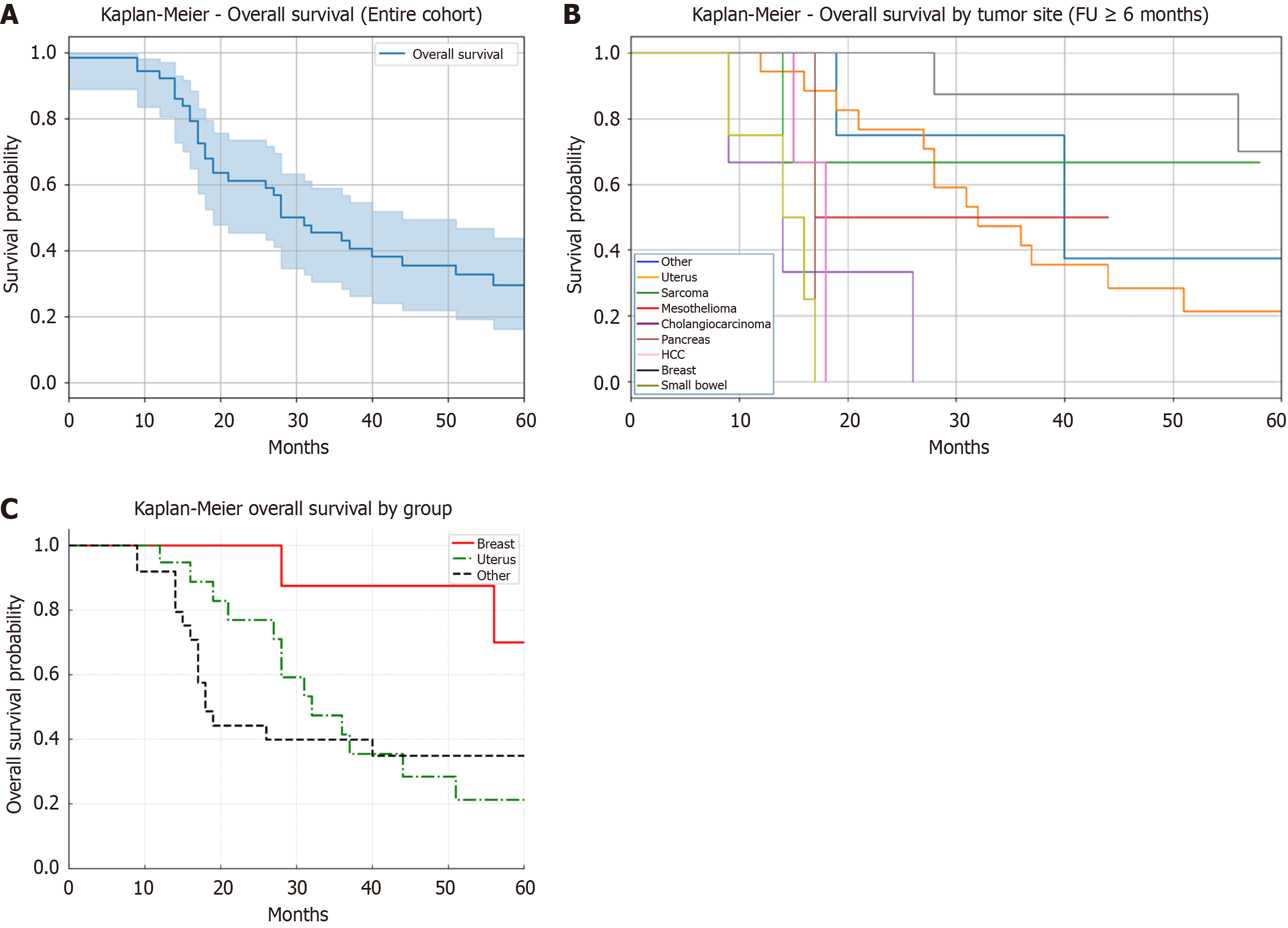
Figure 2 Kaplan-Meier curve showing overall survival.
A: The entire cohort of patients undergoing cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) for peritoneal metastases treated under uncommon indications. The median overall survival was 28 months. Shaded areas represent 95% confidence intervals; B: Stratified by tumor origin in patients treated with CRS and HIPEC for peritoneal metastases under uncommon indications. Only patients with ≥ 6 months of follow-up were included; C: Stratified by tumor group: Breast cancer, uterine cancer, and all other uncommon indications. Patients with breast cancer showed the most favorable survival, followed by those with uterine cancer, while patients with other tumor types experienced the poorest outcomes. HCC: Hepatocellular carcinoma; FU: Follow-up.
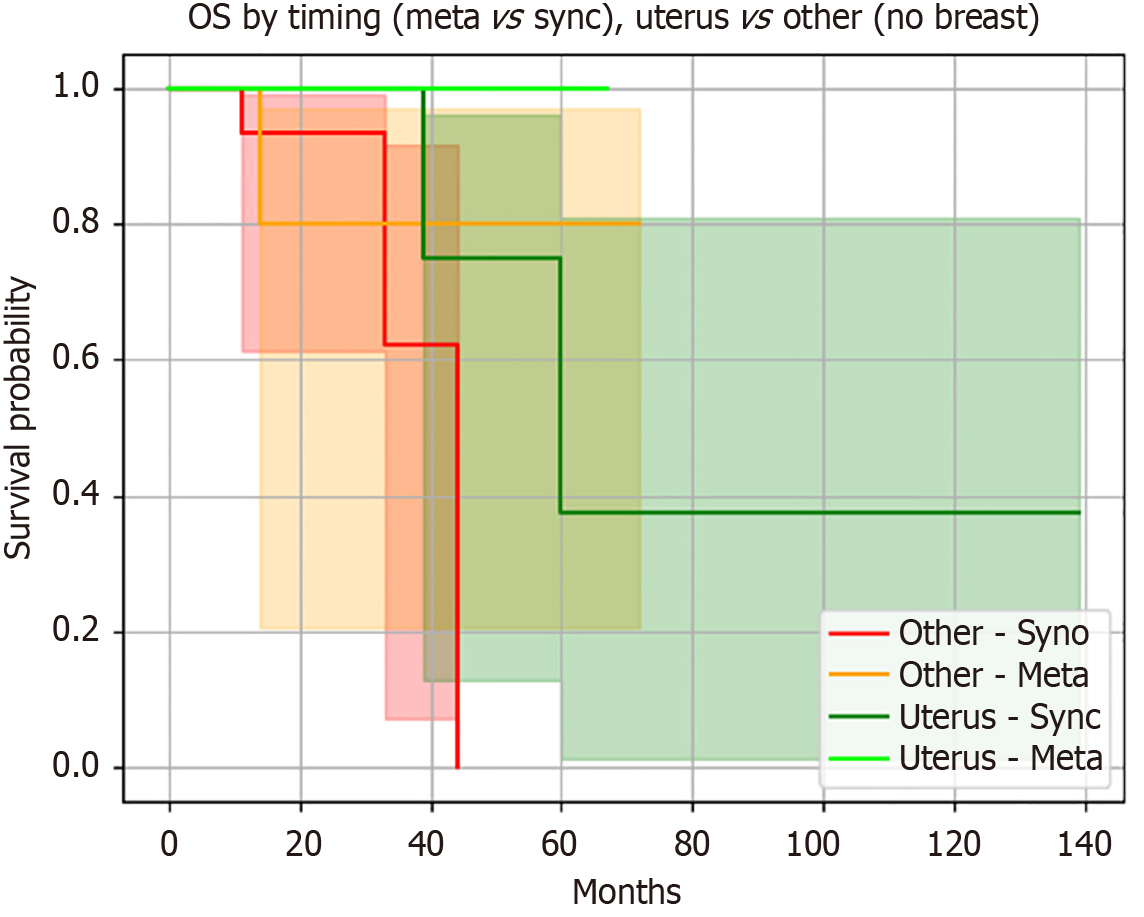
Figure 3 Overall survival stratified by tumor group (uterus vs other) and timing of peritoneal metastases (synchronous vs metach
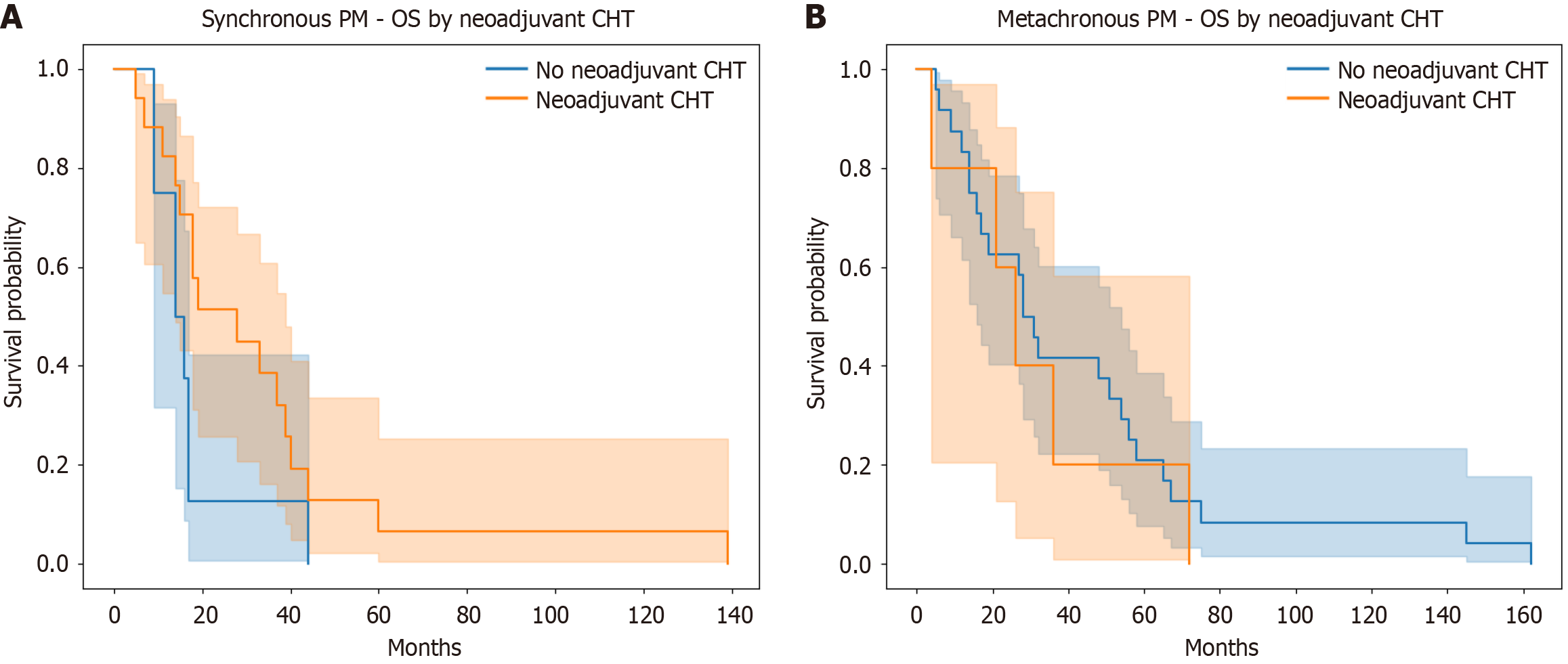
Figure 4 Overall survival by neoadjuvant chemotherapy in patients with peritoneal metastases.
A: In synchronous peritoneal metastases (PM), median overall survival (OS) was longer with neoadjuvant treatment (28.0 months vs 16.0 months), though not statistically significant; B: In metachronous PM, OS was similar regardless of neoadjuvant therapy. PM: Peritoneal metastases; OS: Overall survival; CHT: Chemotherapy.
- Citation: Framarini M, D'Acapito F, Lippolis PV, Di Giorgio A, Di Pietrantonio D, Sommariva A, Sammartino P. Expanding the role of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: A multicenter study on uncommon peritoneal malignancies. World J Clin Oncol 2025; 16(12): 112443
- URL: https://www.wjgnet.com/2218-4333/full/v16/i12/112443.htm
- DOI: https://dx.doi.org/10.5306/wjco.v16.i12.112443