Published online Oct 15, 2025. doi: 10.4251/wjgo.v17.i10.110302
Revised: June 11, 2025
Accepted: August 28, 2025
Published online: October 15, 2025
Processing time: 132 Days and 21.4 Hours
The concept of “duodenal-type follicular lymphoma (FL)” has already been established as a disease entity. On the other hand, because FL that develops in the colorectum is a rare disease, its clinical characteristics, including its treatment and outcome, are poorly understood.
To clarify the characteristic clinical features of colorectal FL.
We identified 5 patients with FL from December 2010 to July 2022 whose co
The median age of the patients was 70 years (range 62-74 years, 3 males and 2 females), and 2 patients were considered to have systemic FL lesions. Endoscopic findings revealed elavated lesions in all 5 patients (polypoid 3, flat elavated 1, papular 1). Only 1 patient underwent therapeutic intervention, and 4 patients chose watchful waiting. Except for 1 patient in which the lesion spontaneously regressed, the disease recurred or progressed in 4 patients, 3 of whom eventually achieved near complete remission with the administration of rituximab and bendamustine (± polatuzumab vedotin). The 5 patients in this study were still alive or exhibited long-term survival before death; the survival time ranged from 8-29 years after the onset of lymphoma.
In the present study, colorectal FL progressed slowly, and overall survival was good because it was sensitive to anticancer drugs even after the disease pro
Core Tip: Follicular lymphoma (FL) occurring in the duodenum has already been established as a disease concept within the category of FL. In response to this, clinical characteristics of the colorectal FL, including its treatment and long-term outcome, are poorly understood owing to the rarity. This study aimed to clarify the characteristic clinical features of the colorectal FL. In the present study, colorectal FL progresses indolently, as with cases of nodal or duodenal lesions, and the overall survival was good because it was sensitive to chemotherapy with administration of bendamustine and rituximab even after the disease progressed without initial treatment.
- Citation: Saito M, Kanaya M, Miyashita N, Yokoyama E, Izumiyama K, Mori A, Morioka M, Kondo T. Colorectal follicular lymphoma: A single-center retrospective study. World J Gastrointest Oncol 2025; 17(10): 110302
- URL: https://www.wjgnet.com/1948-5204/full/v17/i10/110302.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i10.110302
Follicular lymphoma (FL) is the most common indolent B-cell lymphoma[1,2]. Although FL often occurs in the lymph nodes[1,2], it can also develop in the gastrointestinal tract, with most cases originating in the duodenum[3,4]. The characteristic endoscopic findings are numerous whitish granules near the papilla of Vater[5-7]. In contrast, FL that develops in the colorectum is considered rare[4,8], and to date, most reports have focused on endoscopic findings[8,9]; moreover, the actual clinical features, such as its treatment and long-term outcomes, remain largely unknown. To clarify the characteristics of this disease, we report on a series of patients with FL in the colorectum with follow-up at our institution.
This was a retrospective study at our center.
Five patients with FL who had colorectal lesions proven by endoscopic biopsy or endoscopic submucosal dissection (ESD) were identified at our hospital from December 2010 to July 2022. The diagnosis of FL was made histopathologically, but the detection of IgH-BCL2 by fluorescence in situ hybridization was considered equally important. As part of routine clinical care, patients underwent esophagogastroduodenoscopy, contrast-enhanced computed tomography (CT), positron emission tomography-CT, and bone marrow aspiration to determine the extent of the lesion.
In this study, we retrospectively examined the clinical features and characteristics of 5 patients. A survey on the following points was used: (1) Whether FL was the first occurrence or recurrence for the patient; (2) Whether the colorectum was the primary lesion or whether systemic lesions were present; (3) Whether nodal lesions were present; (4) Whether duodenal lesions were present; (5) What site of the colorectum (cecum, colon, rectum) was affected and how many lesions (single or multiple) were present; (6) The endoscopic morphology (details below); (7) The content of initial treatment and its short-term changes; (8) The subsequent clinical course including pathological changes and treatment; and (9) The final outcome (years of survival from the initial onset of lymphoma).
The endoscopic morphology was divided into three subtypes according to the classification by Iwamuro et al[8]: (1) Polypoid-type tumors; (2) Flat elevated-type tumors forming an elevated planar area; and (3) Papular-type tumors resembling lymphoid follicle hyperplasia.
Because this study was conducted as part of a standard clinical treatment under the Japanese health insurance system, no special tests or treatments specific to this study were performed.
The clinical characteristics of the patients are shown in Table 1. The median age of the 5 patients was 70 years (range 62-74 years), 3 were males, 2 were females, and 3 patients had recurrent FL. In all 3 patients in whom the colorectum was thought to be the primary site, the cecum and ascending colon were involved, and 2 of these patients had multiple lesions. Nodal lesions were observed in 2 patients. In both patients, the nodal tumor burden was greater than the single rectal lesion burden, so rectal lymphoma was considered to involve systemic FL.
| No. | Age | Sex | First occurrence/recurrence (initial site) | Primary/systemic | Nodal lesions | Duodenal lesions | Colorectal site/number | Endoscopic morphology |
| 1 | 62 | M | First occurrence | Primary | (-) | (-) | C, A, R/multiple | Polypoid |
| 2 | 74 | M | First occurrence | Primary | (-) | (-) | C, A/multiple | Polypoid |
| 3 | 70 | F | Recurrence (intraperitoneal LN) | Systemic | (+) | (-) | R/single | Polypoid |
| 4 | 71 | M | Recurrence (stomach) | Systemic | (+) | (-) | R/single | Flat elavated |
| 5 | 65 | F | Recurrence (duodenum) | Primary | (-) | (+)1 | C, A (continous)/single | Papular |
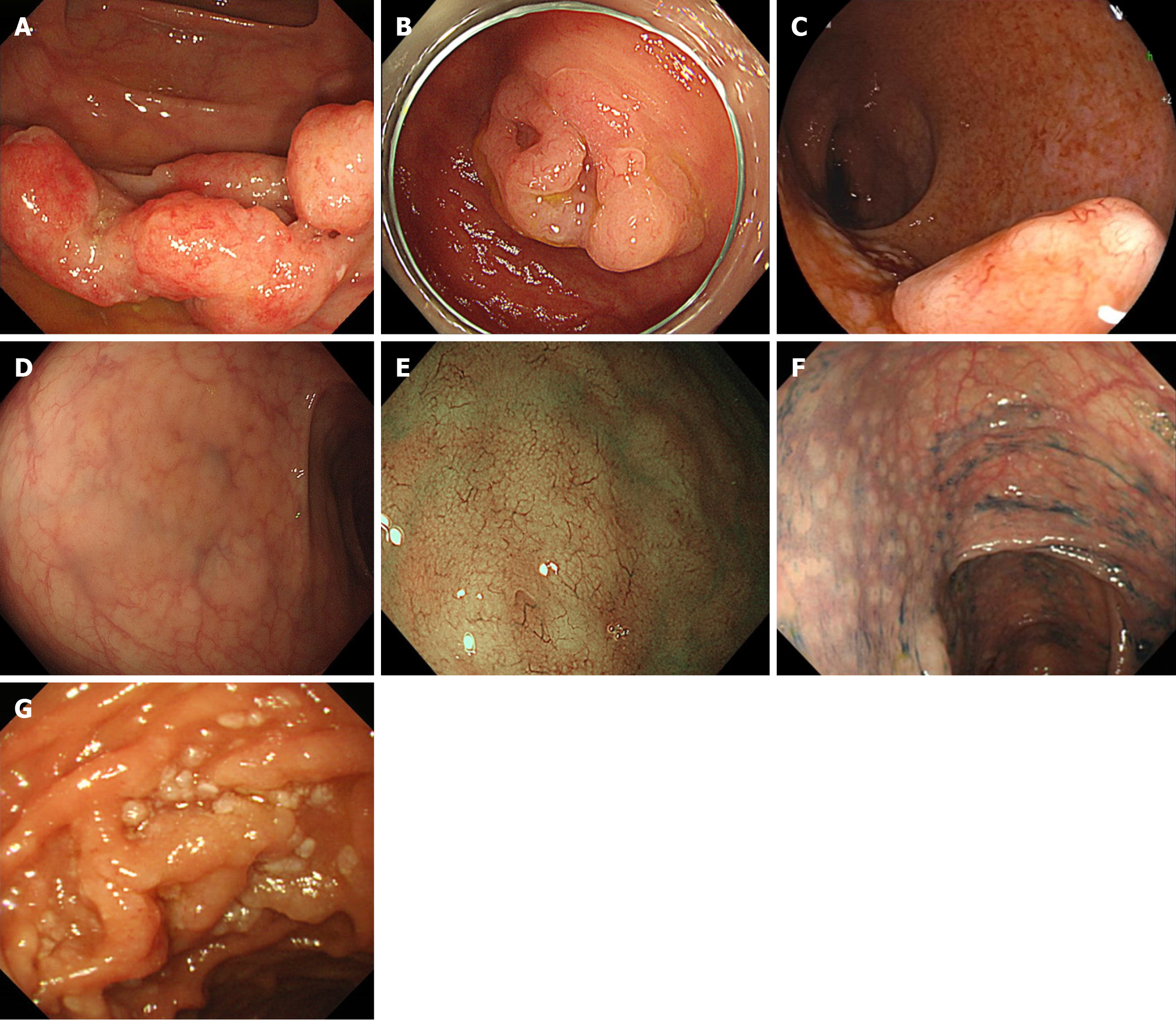
Endoscopic findings are shown in Figure 1. All patients presented with elevated lesions, and 3 patients (case 1, case 2 and case 3) with polypoid lesions (Figure 1A-C) and 1 patient (case 4) with a flat elevated lesion (Figure 1D) presented with dilated superficial blood vessels (Figure 1E). One patient (case 5) presented with papular lesions (Figure 1F) from the cecum to the ascending colon continuously, which were recurrent after achieving complete remission (CR) of “duodenal-type FL” (Figure 1G). None of the other 4 patients had duodenal lesions.
Table 2 shows the clinical course from initial treatment to the final outcome. Only 1 patient (case 1) underwent chemotherapy after the diagnosis was confirmed, and the other 4 patients chose to undergo watchful waiting. In 2 of these patients, diagnosis via biopsy was difficult, so the lesions were removed en bloc via ESD, and after the diagnosis was confirmed, rituximab was administered only twice. In addition, in the case of colorectal recurrence of “duodenal-type FL” (case 5), the lesion regressed spontaneously, and no recurrence has been observed to date. In the other 4 patients, the disease had recurred or progressed, and in 2 patients (case 1 and case 3), histopathological or imaging findings suggested transformation to diffuse large B-cell lymphoma. Three patients (case 1, case 3 and case 4) subsequently achieved an almost CR with the administration of bendamustine and rituximab (BR) (± polatuzumab vedotin). Finally, 5 patients with colorectal FL identified at our institution were alive or had been alive for a long time, ranging from 8-29 years after the initial onset of lymphoma. The causes of death in 2 patients were pneumonia (case 1) and general weakness after corona virus disease 2019 infection (case 4), and were not directly related to FL.
| No. | Initial treatment | Short-term changes | Subsequent clinical course | Final outcome (years of survival) |
| 1 | R-CVP, BR, R-R | CR | 5 years later, intra-colorectal recurrence and transformed into DLBCL after watching for 8 years, and CR was achieved with Pola-BR | Death from other diseases (14 years) |
| 2 | ESD, watch1 | PR | 5 years later, intra-colorectal recurrence, and under watchful waiting without treatment | Alive with disease (8 years) |
| 3 | Watch | SD | 1 year later, nodal lesions were suggested to have transformed into DLBCL, and CR was achieved with Pola-BR etc. | Alive with disease-free (20 years) |
| 4 | ESD, watch1 | SD | 3 years later, the disease recurred throughout the body, and reached CR with BR | Death from other diseases (29 years) |
| 5 | Watch | CR | No recurrence for 10 years | Alive with disease-free (15 years) |
FL arising in the second portion of the duodenum has some distinct clinical features that differ from those of its nodal counterpart[5]. It was referred to as “duodenal-type FL” in the revised 4th and 5th editions of the World Health Organization classification as one of the variants of FL[6,7]. In contrast, as Takata et al[4] noted, colorectal involvement is considered to be less common in patients with FL. They reported that, among 125 patients with primary intestinal FL, 111 (89%) had duodenal involvement, 50 (40%) had jejunal involvement, and 28 (22%) had ileal involvement, whereas only 2 (2%) had cecal involvement, 1 (1%) had colonic involvement, and 2 (2%) had rectal involvement.
In recent years, reports regarding endoscopic findings of colorectal FL lesions have increased[8-10]. Iwamuro et al[8] reported that all patients were observed to have elevated lesions, whereas Yachida et al[11] reported that the lesions were classified into various types, including not only polypoid types but also ulcerative types and diffuse types. None of the lesions in the 5 cases we examined in this study showed ulcers or erosions, and all presented elevated lesions that could be classified into the three subtypes proposed by Iwamuro et al[8] (polypoid, flat elevated, and papular). In case 4, a flat elevated lesion was recognized under normal observation, and the microvascular structure on the tumor surface was observed via narrow-band light imaging[12]. Finally, the lesion was resected en bloc via ESD, and the diagnosis was confirmed histopathologically. Case 5 was a patient with duodenal-type FL who initially had numerous whitish granules in the duodenum, which recurred 4 years later as papular-type colorectal FL. Recently, a case of a duodenal-type FL in the rectum, which had a polypoid morphology, was reported[10]. Whether duodenal-type FL and colorectal FL can be considered essentially the same pathological condition requires further investigation by increasing the number of cases.
With respect to the treatment of advanced-stage nodal FL with a low tumor burden, watchful waiting has previously been shown to be not disadvantageous in terms of overall survival compared with starting treatment immediately after diagnosis[13-15] and is also recommended in the Japanese guidelines[16]. At our institution, we follow this policy and often choose watchful waiting for newly diagnosed cases. With respect to treatment intervention, we administer BR therapy, which has been shown to be more effective than cyclophosphamide, doxorubicin, vincristine and prednisolone (R-CHOP) therapy (median progression-free survival: BR therapy 69.5 months vs R-CHOP therapy 31.2 months; hazard ratio = 0.58; P < 0.0001)[17].
Additionally, regarding duodenal-type FL, the validity of observation without treatment has been recently reported[18]. As presented here, the treatment of colorectal FL, similar to nodal or duodenal-type FL, starts with watchful waiting, and after the disease worsens and progresses, BR (± polatuzumab vedotin) chemotherapy is performed; its favorable therapeutic effects have made it possible to achieve long-term survival. However, 2 patients developed life-threatening infections after completing treatment. Notably, immunosuppression continues even after completion of the BR regimen in elderly FL patients[19,20].
The limitations of this study include: (1) The small sample size; (2) The retrospective study design, which may introduce bias and affect the reliability of the conclusions; and (3) The study’s focus on a rare disease, colorectal FL, making it more difficult to obtain broad insights. However, evaluating the impact of postchemotherapy immunosuppression on infection rates and overall survival in elderly patients may be useful for clinical management practice.
In the present study, colorectal FL progressed indolently, as in cases of nodal or duodenal FL, and the overall prognosis was good because it was highly sensitive to chemotherapy with the BR regimen even after the disease progressed without initial treatment. It will be necessary to accumulate more patients and examine whether colorectal FL can be considered essentially the same pathology as duodenal-type FL.
We would like to thank the doctors at the Department of Cancer Pathology at Hokkaido University, Faculty of Medicine for the histopathological diagnosis of this case series.
| 1. | Muto R, Miyoshi H, Sato K, Furuta T, Muta H, Kawamoto K, Yanagida E, Yamada K, Ohshima K. Epidemiology and secular trends of malignant lymphoma in Japan: Analysis of 9426 cases according to the World Health Organization classification. Cancer Med. 2018;7:5843-5858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 2. | Dada R. Diagnosis and management of follicular lymphoma: A comprehensive review. Eur J Haematol. 2019;103:152-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 3. | Yoshino T, Miyake K, Ichimura K, Mannami T, Ohara N, Hamazaki S, Akagi T. Increased incidence of follicular lymphoma in the duodenum. Am J Surg Pathol. 2000;24:688-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 150] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Takata K, Okada H, Ohmiya N, Nakamura S, Kitadai Y, Tari A, Akamatsu T, Kawai H, Tanaka S, Araki H, Yoshida T, Okumura H, Nishisaki H, Sagawa T, Watanabe N, Arima N, Takatsu N, Nakamura M, Yanai S, Kaya H, Morito T, Sato Y, Moriwaki H, Sakamoto C, Niwa Y, Goto H, Chiba T, Matsumoto T, Ennishi D, Kinoshita T, Yoshino T. Primary gastrointestinal follicular lymphoma involving the duodenal second portion is a distinct entity: a multicenter, retrospective analysis in Japan. Cancer Sci. 2011;102:1532-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 112] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 5. | Yoshino T, Chott A. Duodenal-type follicular lymphoma. In: WHO Classification of Tumours, 5th ed. Digestive System Tumours. Lyon, France: IARC press, 2019: 383-385. |
| 6. | Jaffe ES, Harris NL, Swerdlow SH, Ott G, Nathwani BN, de Jong D, Yoshino T, Spagnolo D, Gascoyne RD. Duodenal-type follicular lymphoma (in Follicular lymphoma). In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Arber DA, Hasserjian RP, Le Beau MM, Orazi A, Siebert R. WHO Classification of Tumours of Haematopietic and Lymphoid Tissues, Revised 4th ed. Lyon, France: IARC press, 2017: 276-277. |
| 7. | Karube K, Herfarth K, Lorsbach RB, Raderer M. Weigert O: Duodenal-type follicular lymphoma. In: WHO Classification of Tumours, 5th ed. Haematolymphoid Tumours Part B., Lyon, France: IARC press, 2024: 437-439. |
| 8. | Iwamuro M, Okada H, Takata K, Takenaka R, Inaba T, Mizuno M, Kobashi H, Tanaka S, Yoshioka M, Kondo E, Yoshino T, Yamamoto K. Colorectal Manifestation of Follicular Lymphoma. Intern Med. 2016;55:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Tanaka S, Nagahara T, Hirakawa T, Ohta T, Fujimoto T, Takada R. Follicular lymphoma of the rectum. Intern Med. 2008;47:1277-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Huang P, Wang D, Liu W. Duodenal-Type Follicular Lymphoma in the Rectum. Am J Gastroenterol. 2024;119:1723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Yachida T, Matsuda T, Sakamoto T, Nakajima T, Kakugawa Y, Maeshima AM, Taniguchi H, Kushima R, Tobinai K, Kobara H, Masugata H, Masaki T, Saito Y. Endoscopic features of colorectal lymphoma according to histological type. JGH Open. 2022;6:257-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Fujiya M, Kashima S, Ikuta K, Dokoshi T, Sakatani A, Tanaka K, Ando K, Ueno N, Tominaga M, Inaba Y, Ito T, Moriichi K, Tanabe H, Saitoh Y, Kohgo Y. Decreased numbers of vascular networks and irregular vessels on narrow-band imaging are useful findings for distinguishing intestinal lymphoma from lymphoid hyperplasia. Gastrointest Endosc. 2014;80:1064-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Brice P, Bastion Y, Lepage E, Brousse N, Haïoun C, Moreau P, Straetmans N, Tilly H, Tabah I, Solal-Céligny P. Comparison in low-tumor-burden follicular lymphomas between an initial no-treatment policy, prednimustine, or interferon alfa: a randomized study from the Groupe d'Etude des Lymphomes Folliculaires. Groupe d'Etude des Lymphomes de l'Adulte. J Clin Oncol. 1997;15:1110-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 483] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 14. | Ardeshna KM, Smith P, Norton A, Hancock BW, Hoskin PJ, MacLennan KA, Marcus RE, Jelliffe A, Vaughan G, Hudson, Linch DC; British National Lymphoma Investigation. Long-term effect of a watch and wait policy versus immediate systemic treatment for asymptomatic advanced-stage non-Hodgkin lymphoma: a randomised controlled trial. Lancet. 2003;362:516-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 380] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 15. | Ardeshna KM, Qian W, Smith P, Braganca N, Lowry L, Patrick P, Warden J, Stevens L, Pocock CF, Miall F, Cunningham D, Davies J, Jack A, Stephens R, Walewski J, Ferhanoglu B, Bradstock K, Linch DC. Rituximab versus a watch-and-wait approach in patients with advanced-stage, asymptomatic, non-bulky follicular lymphoma: an open-label randomised phase 3 trial. Lancet Oncol. 2014;15:424-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 293] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 16. | Japanese Society of Hematology. Hematopoietic tumor treatment guidelines. [cited August 22, 2025]. Available from: https://www.jshem.or.jp/gui-hemali/index.html. |
| 17. | Rummel MJ, Niederle N, Maschmeyer G, Banat GA, von Grünhagen U, Losem C, Kofahl-Krause D, Heil G, Welslau M, Balser C, Kaiser U, Weidmann E, Dürk H, Ballo H, Stauch M, Roller F, Barth J, Hoelzer D, Hinke A, Brugger W; Study group indolent Lymphomas (StiL). Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: an open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet. 2013;381:1203-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 992] [Cited by in RCA: 1149] [Article Influence: 88.4] [Reference Citation Analysis (0)] |
| 18. | Alnughmush A, Fakih RE, Alyamany R, Bakshi N, Alhayli S, Aljurf M. Duodenal-type follicular lymphoma: comprehensive insights into disease characteristics and established treatment strategies. Curr Opin Oncol. 2024;36:577-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 19. | Gafter-Gvili A, Polliack A. Bendamustine associated immune suppression and infections during therapy of hematological malignancies. Leuk Lymphoma. 2016;57:512-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 20. | Franceschini E, Pellegrino M, Todisco V, Dolci G, Bettelli F, Meschiari M, Bedini A, Fregni-Serpini G, Grottola A, Guaraldi G, Pecorari M, Sarti M, Luppi M, Perno CF, Mussini C. Persistent SARS-CoV-2 infection with multiple clinical relapses in two patients with follicular lymphoma treated with bendamustine and obinutuzumab or rituximab. Infection. 2023;51:1577-1581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/