©The Author(s) 2025.
World J Gastroenterol. Dec 28, 2025; 31(48): 112972
Published online Dec 28, 2025. doi: 10.3748/wjg.v31.i48.112972
Published online Dec 28, 2025. doi: 10.3748/wjg.v31.i48.112972
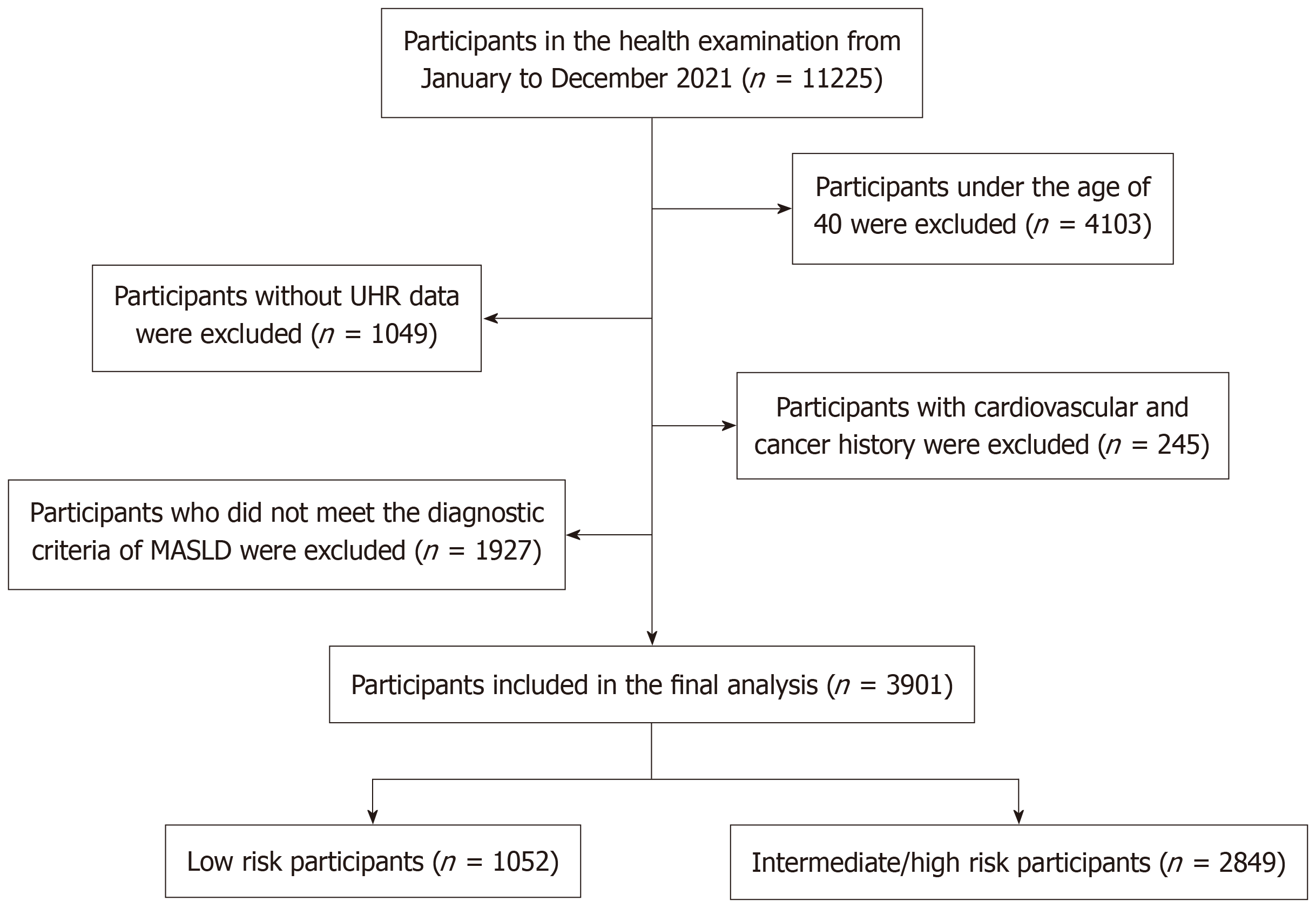
Figure 1 Participant selection flowchart.
UHR: Uric acid-to-high-density lipoprotein cholesterol ratio; MASLD: Metabolic dysfunction-associated steatotic liver disease.
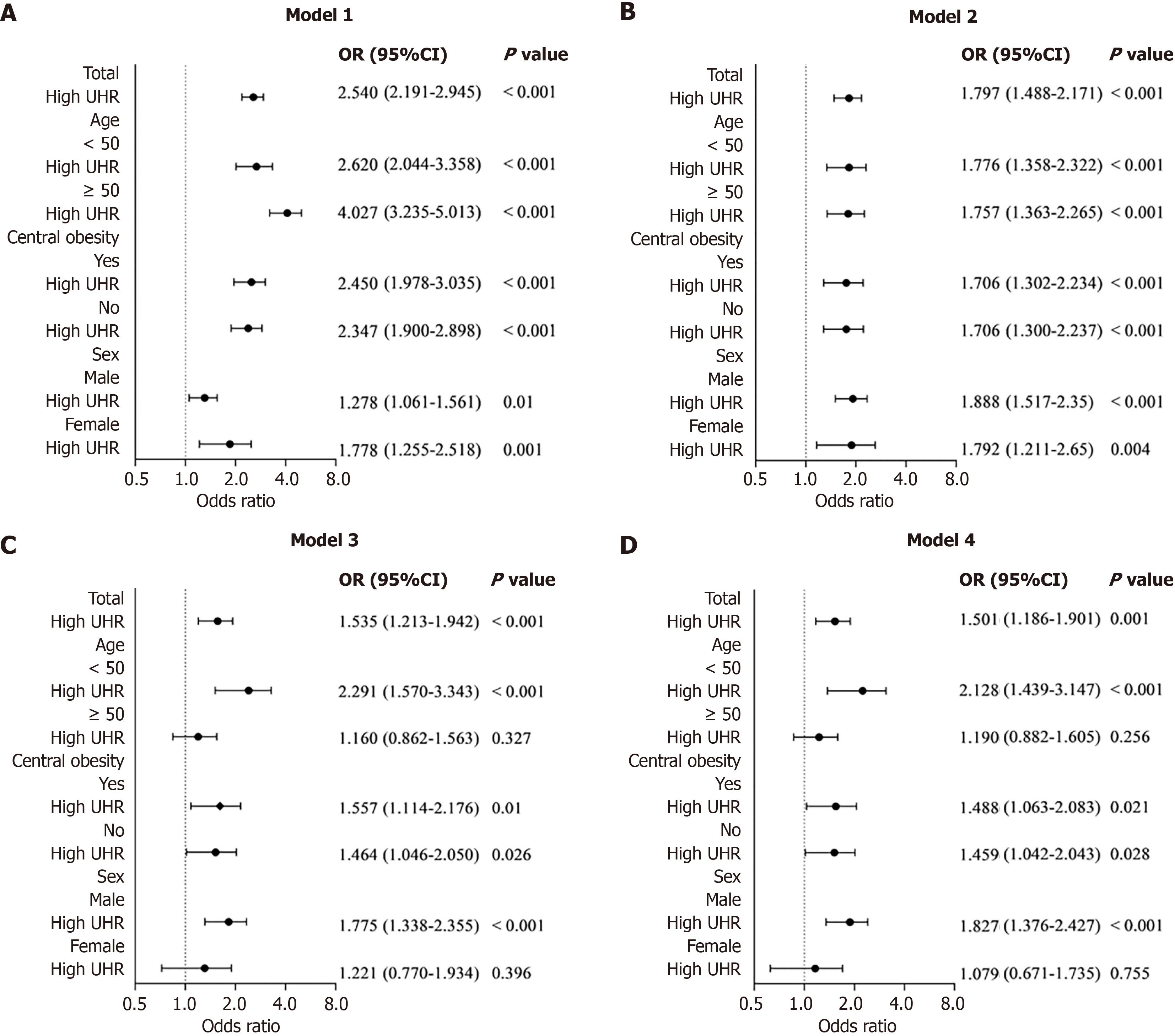
Figure 2 The forest plot depicts the association between high uric acid-to-high-density lipoprotein cholesterol ratio and high-risk Framingham risk score in the general population, along with subgroup analyses stratified by age, central obesity, and sex.
It shows the adjusted odds ratios for this association after controlling for multiple covariates. UHR: Uric acid-to-high-density lipoprotein cholesterol ratio; OR: Odds ratio; CI: Confidence interval.
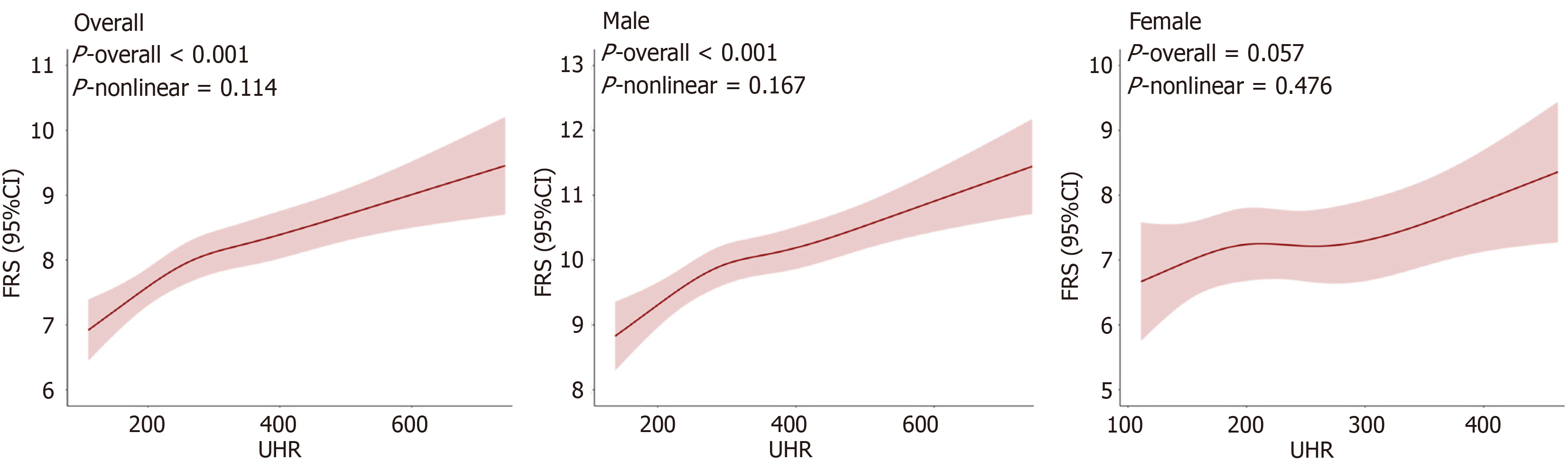
Figure 3 Adjusted dose-response curve of uric acid-to-high-density lipoprotein cholesterol ratio on predicted Framingham risk score in the overall population, males, and females.
The red line represents the curve fitting between the independent variable and the dependent variable, and the red area indicates the 95% confidence interval. Adjusted factors include sex, age, smoking, hypertension, central obesity, hyperlipidemia, body mass index, diabetes, metabolic syndrome, and metabolic dysfunction-associated steatotic liver disease. UHR: Uric acid-to-high-density lipoprotein cholesterol ratio; FRS: Framingham risk score; CI: Confidence interval.
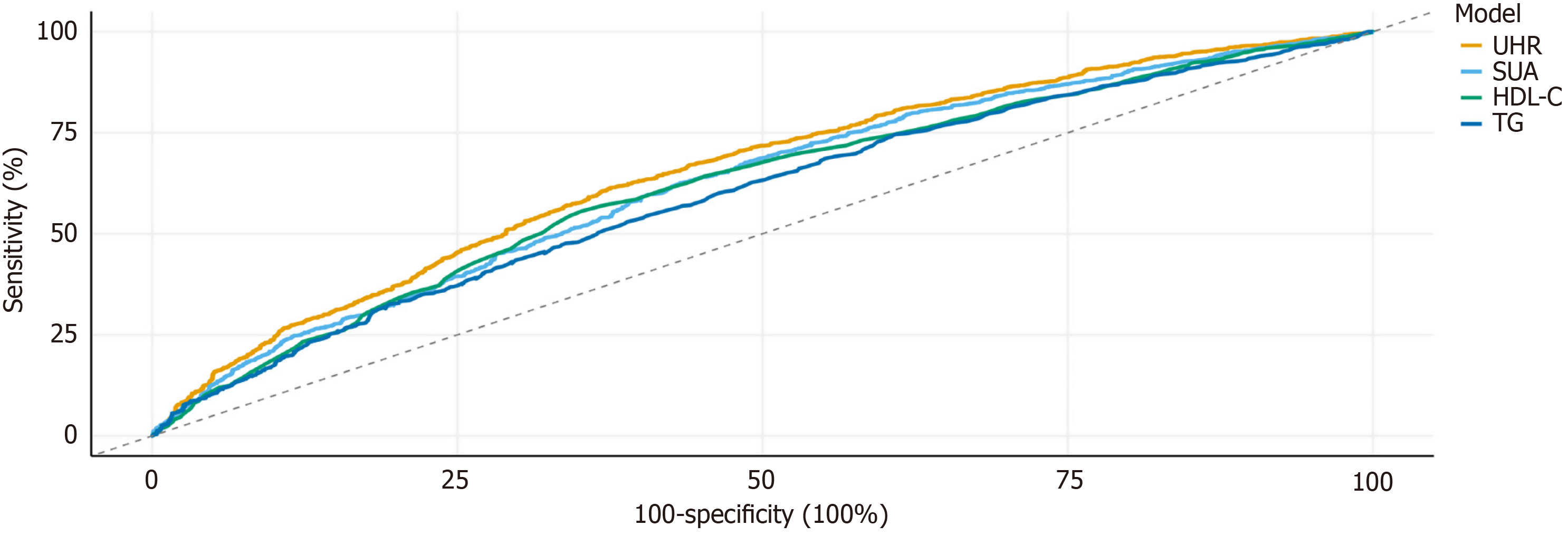
Figure 4 Receiver operating characteristic analysis of uric acid-to-high-density lipoprotein cholesterol ratio and traditional lipid parameters for predicting intermediate/high cardiovascular risk by Framingham risk score.
UHR: Uric acid to high-density lipoprotein cholesterol ratio; SUA: Serum uric acid; HDL-C: High-density lipoprotein cholesterol; TG: Triglycerides.
- Citation: Wang Y, Ma GH, Qu MY, Xu QS, Huang HX. Serum uric acid-to-high-density lipoprotein cholesterol ratio and cardiovascular risk in Asian patients with metabolic dysfunction-associated steatotic liver disease. World J Gastroenterol 2025; 31(48): 112972
- URL: https://www.wjgnet.com/1007-9327/full/v31/i48/112972.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i48.112972