Published online Apr 6, 2021. doi: 10.12998/wjcc.v9.i10.2238
Peer-review started: December 17, 2020
First decision: January 6, 2021
Revised: January 13, 2021
Accepted: January 26, 2021
Article in press: January 26, 2021
Published online: April 6, 2021
Processing time: 102 Days and 20.4 Hours
Four-liter polyethylene glycol (PEG) solutions are effective for bowel cleansing, but their large volume might hinder patient compliance. Due to the unique features of Asians, 4 L PEG might be a suboptimal bowel preparation in predominantly ethnically Asian countries. In view of this, a balance should be achieved between the volume and effectiveness. The ideal bowel cleansing regimen for a colonoscopy has yet to be determined in a Chinese population.
To compare the cleansing efficacy of 3 L PEG plus simethicone with 4 L PEG.
A total of 291 patients were randomly allocated to two groups: Group 1 (n = 145) received 4 L split-dose PEG (4-P); group 2 (n = 146) received 3 L split-dose PEG plus simethicone (3-PS). Bowel-cleansing efficacy was evaluated by endoscopists using the Boston bowel preparation scale (BBPS) and the bubbles score.
Although there were no significant differences in the total BBPS score or the adequate rate of bowel preparation between the two groups, the BBPS score of the right-side colon was significantly higher in the 3-SP group (2.37 ± 0.54 vs 2.21 ± 0.78; P = 0.04). Moreover, the use of simethicone significantly reduced bubbles in all colon segments (P < 0.001). The mean withdrawal time was significantly shorter in the 3-PS group (8.8 ± 3.4 vs 9.6 ± 2.3; P = 0.02). Furthermore, significantly more proximal adenomas were detected in the 3-PS group (53.6% vs 45.7%; P = 0.03). In addition, the proportions of patients with nausea and bloating were significantly lower in the 3-SP group (P < 0.01 for both). More patients in the 3-PS group expressed willingness to repeat the bowel preparation (87.7% vs 76.6%, P = 0.01).
Three-liter PEG shows satisfactory bowel cleansing despite the decrease in dosage, and addition of simethicone with better bubble elimination and enhanced patient acceptance offers excellent potential impact on the detection of proximal adenomas in Chinese patients.
Core Tip: The incidence and mortality of colorectal cancer have been rapidly increasing in China over the last decade. A high-quality bowel preparation is a key determinant of the efficacy of colonoscopy to reduce the incidence of colorectal cancer, but 4 L polyethylene glycol might be a suboptimal bowel preparation in the Chinese population. In view of a balance between the volume and effectiveness, this study showed that 3 L polyethylene glycol had satisfactory bowel cleansing, and addition of simethicone with better bubble elimination and enhanced patient acceptance offered excellent potential impact on the detection of proximal adenomas in Chinese patients.
- Citation: Zhang H, Liu J, Ma SL, Huang ML, Fan Y, Song M, Yang J, Zhang XX, Song QL, Gong J, Huang PX, Zhang H. Impact of simethicone on bowel cleansing during colonoscopy in Chinese patients. World J Clin Cases 2021; 9(10): 2238-2246
- URL: https://www.wjgnet.com/2307-8960/full/v9/i10/2238.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i10.2238
Colorectal cancer (CRC) is a major cause of death worldwide. In spite of the reduction of its incidence in Western countries over the last decade, its incidence and mortality have been rapidly increasing in Asian countries, including China and Korea[1,2]. Currently, colonoscopy is a standard first-line tool for the screening, surveillance, and prevention of CRC because it enables removal of colorectal precancerous lesions[3,4]. A high-quality bowel preparation is a key determinant of its efficacy to reduce the incidence of CRC. Early diagnosis is associated with better patient survival and quality of life. Unfortunately, up to 25% of patients who undergo colonoscopy have been shown to have poor bowel preparation quality[5].
In the European and American guidelines, high-volume polyethylene glycol (PEG) solutions are currently recommended as the first-line choice for bowel preparation due to their excellent efficacy[5,6]. In contrast, lower volume bowel preparations, such as 2 L PEG, have been widely used in Chinese countries in recent years[7]. Although 2 L PEG preparations are gaining popularity and have shown better compliance among patients, their efficacy remains a priority in view of the adverse effects of inadequate preparation on the efficacy of CRC prevention.
A recent meta-analysis showed the superiority of split-dose high-volume (≥ 3 L) to low-volume PEG in terms of efficacy[8]. In addition, a multicenter randomized, controlled trial concluded that 3 L split-dose PEG is superior to 2 L PEG in improving safety and compliance in Chinese populations[9]. Simethicone is an effective antifoaming agent and is commonly used to eliminate bubbles during endoscopic procedures. A combination of simethicone and PEG has been shown to improve the mucosal visibility of the bowel during colonoscopies. A large volume (4 L) of PEG would ensure a better quality of bowel cleansing but might be poorly tolerated. Optimal bowel preparation with PEG solutions by reducing the volume of the solution without influencing its effectiveness that is most suitable for the Chinese population is still controversial. In consideration of achieving a balance between effectiveness and volume, we designed this prospective, randomized clinical study to compare the effectiveness and compliance with bowel cleansing between 3 L PEG plus simethicone and 4 L PEG.
This was a single-center, prospective, randomized, endoscopist-blinded study. Patients were randomly allocated to two groups by a computer-based randomization list: Split-dose of 4 L PEG (4-P) group or split-dose of 3 L PEG plus simethicone (3-PS) group. This study was conducted at the Central Hospital of Wuhan (Wuhan, China) from January 2019 to June 2019 and was approved by the Ethical Committee of the Central Hospital of Wuhan. All patients gave informed consent for their participation. This study included adult participants who underwent colonoscopy. The patients included were between age of 18 and 75 years. The exclusion criteria included pregnancy, gastrointestinal perforation or obstruction, active gastrointestinal bleeding, significant cardiac/renal/hepatic diseases, severe constipation or IBD, allergy to PEG or simethicone, and any mental illness. All eligible patients were randomized into the two groups by a computer-generated number list. After randomization, the patients were required to complete a bowel preparation questionnaire before the colonoscopy.
The bowel preparation regimens were PEG 4000 (each liter containing 64 g PEG 4000, 5.7 g sodium sulfate, 1.68 g sodium bicarbonate, 1.46 g sodium chloride, 0.75 g potassium chloride; Beaufour Ipsen Pharmaceutical Co, France) and simethicone (30 mL, 1200 mg, Menarini Pharmaceutical Co. Ltd., Italy). Colonoscopy was performed by experienced colonoscopists (> 2000 colonoscopies per year) who were blinded to the bowel preparation regimens that the patients had received. Olympus CF-H290I colonoscopes were used to perform all procedures in this trial.
All eligible patients were randomized to the two groups. Participants in the two groups received a split dose of PEG. Participants in the 4-P group were to begin to drink the dose at a rate of 250 mL every 15 min. Half the dose (2 L) was taken the night 19:00-21:00 before the colonoscopy, and on the day of the procedure, they took another 2 L 4-6 h before the colonoscopy. In the 3-PS group, patients were told to take 1 L PEG at 19:00 h the day before the procedure, and the remaining 2 L in the early morning 4-6 h before the scheduled colonoscopy. The dose of simethicone was consumed within half an hour to one hour after all of the PEG was consumed. Participants in the two groups were instructed to follow a low-residue diet on the day before the colonoscopy.
The primary efficacy endpoints were the Boston bowel preparation scale (BBPS)[10] and the bubbles score. Bowel cleansing was assessed by endoscopists who were blinded to the preparation method. The BBPS is a validated bowel preparation scoring system to evaluate the quality of bowel preparation. The BBPS was rated according to a 4-point scale (0-3) as follows: Unprepared (grade 0) = solid stool obscuring the colonic mucosa despite aggressive washing and clearing; fair (grade 1) = residual stool and opaque liquid obscuring the colonic mucosa leading to only a portion of the mucosa of the colon segment being visible; good (grade 2) = minor amount of turbid fluid or stool residue, but the colonic mucosa is seen as well; and excellent (grade 3) = the entire colonic mucosa is seen well, with no residual stool or opaque liquid. Each segment of the colon, including the left, transverse, and right segments, is rated from 0 to 3. The total score is a 9-point scale ranging from 0 to 9 (0 = very poor, 9 = excellent). Total scores of ≥ 6 were defined as adequate bowel preparation.
The bubbles score was used to evaluate its impact on colonic mucosal visibility and was rated according to a 4-point scale (0-3), as has been used in previous studies[11]: 0 (no bubbles): > 90% mucosa clear of bubbles not requiring irrigation; 1 (minimal bubbles): 75%-89% mucosa clear of bubbles not requiring irrigation; 2 (moderate bubbles): 50%-74% mucosa clear of bubbles and requiring irrigation; and 3 (severe bubbles): < 50% mucosa clear of bubbles and requiring irrigation. Each segment of the colon, including the left, transverse, and right segments, is rated from 0 to 3. The total score is a 9-point scale ranging from 0 to 9 (0 = excellent, 9 = very poor).
Secondary efficacy endpoints included the adenoma/polyp detection rate (ADR/PDR), cecal intubation time, and withdrawal time.
Tolerability was assessed by inquiring about the occurrence of adverse events such as nausea, vomiting, bloating, abdominal pain, and sleep disturbance during the process of bowel preparation. In addition, willingness to repeat the same bowel preparation in the future was also assessed.
The sample size calculation was designed to assess the superiority of 3 L PEG plus simethicone compared with 4 L PEG in bowel cleansing. Our primary outcome was adequate bowel cleansing rate defined as a total BBPS score ≥ 6 or higher. Based on a previous study performed in Canada[12], the adequate rate based on the BBPS was estimated to be 85% and 95% for 3 L PEG plus simethicone and 4 L PEG, respectively.
The sample size of 134 patients per group was determined using a power of 0.80, α of 0.05, and dropout rate of 5%, which was increased to approximately 300 patients in total. Associations between the categorical variables and the continuous variables were assessed using the chi-squared test and t-test. A P value less than 0.05 was regarded as statistically significant. Statistical analyses were performed using SPSS statistical software (version 17.0, SPSS Inc., Chicago, IL, United States).
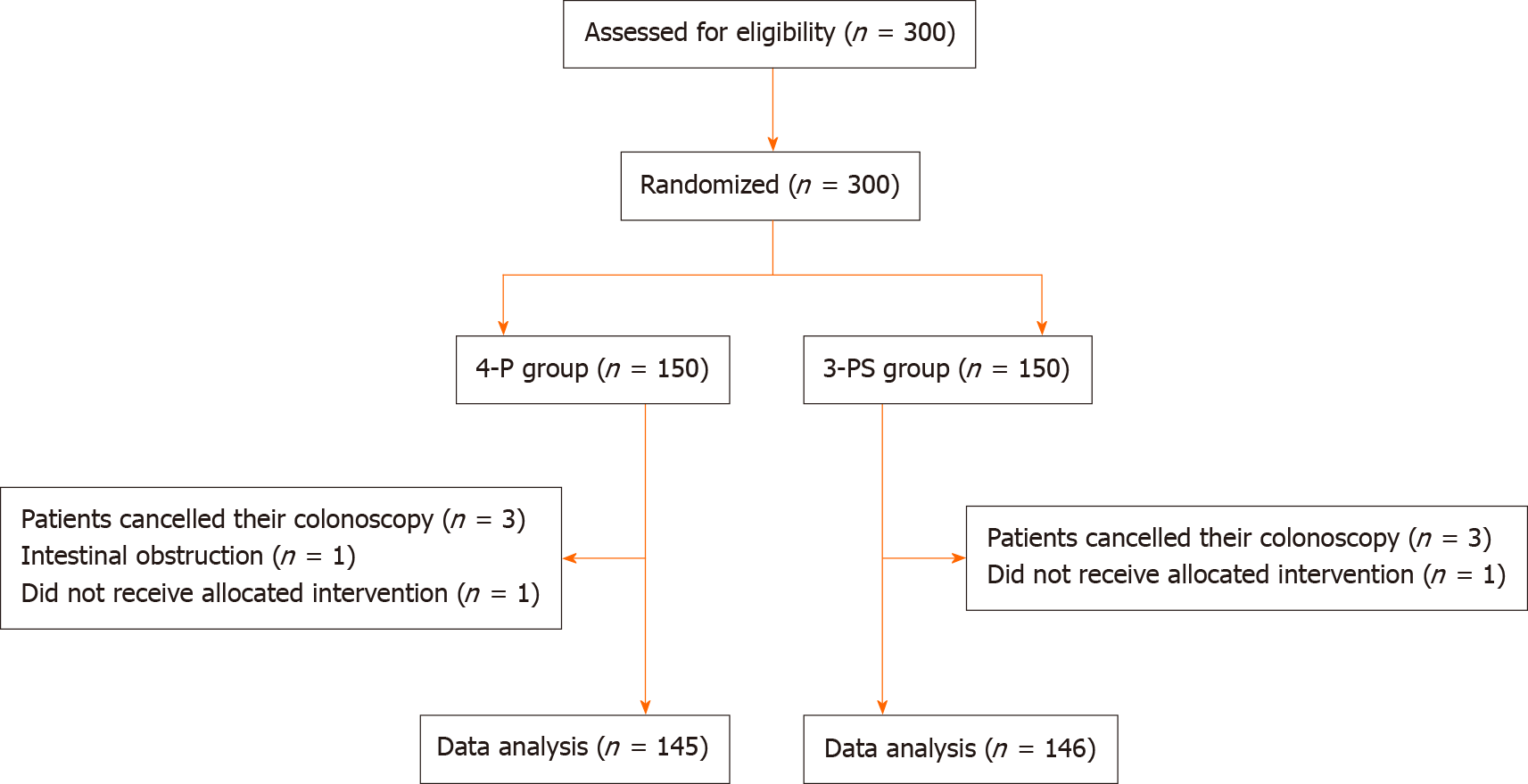
A total of 300 patients aged 18 to 75 years old were randomly allocated to the 4-P group (n = 145) or the 3-PS group (n = 146) between January 2019 and June 2019. Nine patients were excluded from the analysis (patient refusal in 6, intestinal obstruction in 1, and no allocated intervention in 2). Finally, 145 participants in the 4-P group and 146 in the 3-PS group underwent colonoscopy and were included. The baseline characteristics of the patients are shown in Table 1, and there were no statistically significant differences in baseline characteristics between the two groups (Figure 1).
| Variable | 4-P (n = 145) | 3-PS (n = 146) | P value1 |
| Age, yr, (mean ± SD) | 48.3 ± 12.1 | 47.9 ± 13.5 | 0.79 |
| Male, n (%) | 74 (51.0) | 70 (47.9) | 0.60 |
| Diabetes, n (%) | 12 (8.3) | 9 (6.2) | 0.49 |
| Indication for colonoscopy, n (%) | |||
| Rectal bleeding | 23 (15.9) | 27 (18.5) | 0.55 |
| Diarrhea | 22 (15.2) | 28 (19.2) | 0.37 |
| Constipation | 18 (12.4) | 14 (9.6) | 0.44 |
| Abdominal discomfort | 46 (31.7) | 34 (23.3) | 0.11 |
| Surveillance/screening | 20 (13.8) | 30 (20.5) | 0.13 |
| Polypectomy/resection | 12 (8.3) | 10 (6.8) | 0.65 |
| Other | 4 (2.7) | 3 (2.1) | 0.70 |
BBPS and bubble scores: The efficacy of bowel preparation is shown in Table 2. The total BBPS score was 7.11 ± 1.52 in the 4-P group and 7.06 ± 1.73 in the 3-PS group, and there was no significant difference between the two groups (P = 0.79). However, in the right-side colon, the BBPS score in the 3-PS group was significantly higher than that in the 4-P group (P = 0.04). No differences were found in terms of BBPS scores for the transverse and left colon segments. In addition, the adequate rate of bowel preparation was 89.6% in the 4-P group and 86.9% in the 3-PS group (odds ratio = 0.77, 95% confidence interval: 0.38-1.58, P = 0.48). The use of simethicone added to 3 L PEG reduced bubbles in all colon segments, which suggested a higher quality of bowel mucosal visibility in the 3-PS group. There was a statistically significant difference in bubbles between the two groups (P < 0.001). Although the mean cecal intubation time was similar between the two groups, there was a significant difference with regard to withdrawal time (P = 0.02).
| Variable | 4-P (n = 145) | 3-PS (n = 146) | P value1 |
| Cecal intubation success, % | 100 | 100 | 1 |
| Cecal intubation time (mean ± SD), min | 7.6 ± 1.9 | 7.8 ± 1.9 | 0.37 |
| Withdrawal time (mean ± SD), min | 9.6 ± 2.3 | 8.8 ± 3.4 | 0.02 |
| Adenoma, n (%) | 22 (15.2) | 24 (16.4) | 0.77 |
| Polyp, n (%) | 46 (31.7) | 51 (35.0) | 0.56 |
| Colitis, n (%) | 13 (9.0) | 16 (11.0) | 0.57 |
| Normal, n (%) | 61 (42.1) | 57 (39.0) | 0.60 |
| Others, n (%) | 7 (4.8) | 5 (3.4) | 0.55 |
| BBPS | |||
| Total score (mean ± SD) | 7.11 ± 1.52 | 7.06 ± 1.73 | 0.79 |
| Right colon (mean ± SD) | 2.21 ± 0.78 | 2.37 ± 0.54 | 0.04 |
| Transverse colon (mean ± SD) | 2.56 ± 0.50 | 2.44 ± 0.77 | 0.12 |
| Left colon (mean ± SD) | 2.34 ± 0.72 | 2.25 ± 0.84 | 0.33 |
| BBPS ≥ 6, n (%) | 136 (93.8) | 132 (90.4) | 0.29 |
| Bubble score, mean (SD) | 2.85 ± 1.91 | 1.21 ± 1.57 | < 0.001 |
| Left colon2 | 0.68 ± 0.80 | 0.27 ± 0.50 | < 0.001 |
| Transverse colon | 0.64 ± 0.75 | 0.25 ± 0.51 | < 0.001 |
| Right colon3 | 1.52 ± 1.06 | 0.66 ± 0.96 | < 0.001 |
| Total number of adenomas | 35 | 56 | 0.009 |
| Adenoma location, n (%) | |||
| Proximal4 | 16 (45.7) | 30 (53.6) | 0.03 |
| Distal5 | 19 (54.3) | 26 (46.4) | 0.27 |
| Adenoma size, n (%) | |||
| ≤ 5 mm | 19 (54.3) | 32 (57.1) | 0.05 |
| > 5 mm | 16 (45.7) | 24 (42.9) | 0.18 |
| Willingness to repeat bowel preparation, n (%) | 111 (76.6) | 128 (87.7) | 0.01 |
ADR/PDR: Although the ADR and PDR were similar between the groups (16.4% vs 15.2%; 35.0% vs 31.7%), the total number of adenomas detected was significantly higher in the 3-PS group (35 vs 56; P = 0.009). Although the ADR for the adenomas with a size less than 5 mm was different with borderline statistical significance (P = 0.05), more proximal adenomas were detected in the 3-PS group (P = 0.03).
Willingness to repeat bowel preparation and patient tolerability: More patients in the 3-PS group expressed a willingness to repeat the bowel preparation (87.7% vs 76.6%, P = 0.01). No serious adverse events were found in the study population (Table 3). Although there were no significant differences between the two groups, fewer patients reported adverse events in the 3-PS group than in the 4-P group (39.7% vs 46.2%). The proportions patients with nausea (22.0% vs 36.6%, P = 0.006) and bloating (20.5% vs 40%, P = 0.001) were significantly lower in the 3-PS group than in the 4-P group, but symptoms such as abdominal pain, vomiting, and sleep disturbance were similar between the groups.
| Symptom | 4L (n = 145) | 3L + S (n = 146) | P value1 |
| Adverse events, n (%) | 67 (46.2) | 58 (39.7) | 0.26 |
| Nausea, n (%) | 53 (36.6) | 32 (22.0) | 0.006 |
| Abdominal pain, n (%) | 13 (9.0) | 12 (8.2) | 0.82 |
| Vomiting, n (%) | 18 (12.4) | 12 (8.2) | 0.24 |
| Bloating, n (%) | 58 (40) | 30 (20.5) | 0.0004 |
| Sleep disturbance, n (%) | 60 (41.4) | 50 (34.2) | 0.21 |
The effectiveness of a colonoscopy in significantly reducing the incidence and mortality of CRC[13] depends on adequate bowel preparation and removal of colorectal precancerous lesions[14]. Inadequate bowel preparation not only increases the economic cost and prolongs the procedure time but also increases the number of potential lesions being missed, especially those in the proximal colon[15]. A prospective observational study revealed a threefold higher miss rate for adenomas when bowel preparation was inadequate[16].
In the recent consensus statement by the Chinese Society for Gastrointestinal Endoscopy, 3-L split-dose PEG was strongly recommended as the preferred choice for bowel cleansing in the Chinese population[17]. In view of its cleansing efficacy, the results of our study demonstrated that the 3-PS group had a higher adequate rate of bowel preparation and was not inferior to the 4-P group. The noteworthy finding in this study was that the BBPS score in the right-side colon was significantly higher in the 3-PS group. Furthermore, the use of simethicone added to 3 L PEG could statistically reduce bubbles in the entire colon and had a higher quality of bowel mucosal visibility.
According to the European Society for Gastrointestinal Endoscopy, a minimum standard of more than 90% adequate bowel preparation has been recently recommended[18]. It is known that Asian populations have difficulty tolerating the 4 L PEG of bowel preparation that is commonly used in Western countries[9]. Our results showed that the adequate bowel preparation rate (BBPS > 6) in the 3-PS group was 90.4%, which was not inferior to that in the 4-P group (P = 0.29). We suggest that the addition of simethicone to 3 L split-dose PEG is a valuable option for bowel preparation and an alternative method when a large volume of PEG cannot be tolerated.
The ADR has been deemed to be the main indicator of the quality of bowel cleansing during colonoscopy[19]. The current international guidelines have recommended that the ADR should be ≥ 25% overall as the minimal requirement of surveillance colonoscopy[20]. A recent meta-analysis revealed a positive effect of simethicone with statistical significance in the low ADR group (< 25%). An interesting aspect of this analysis was that the populations of the included studies in the low ADR group were all from Asian countries[21]. This phenomenon might partly explain the increase in the incidence and mortality of CRC in Asian countries. Our study showed that the ADR was also less than 25%; therefore, simethicone might have a positive effect in combination with the PEG solution.
A previous study reported that CRC in Eastern China has undergone a rightward change in its site distribution in the past 2 decades[22]. Therefore, improving the effectiveness of right-sided colon cleansing plays a key role in improving compliance with screening programs, which is crucial for screening efficiency in CRC prevention. The most important finding in our study was that a significantly higher ADR in the proximal colon was confirmed in the 3-PS group. We noted better visualization of the whole large intestine, especially the right colon, probably due to the effect of simethicone. As bubbles are often present in the proximal colon, especially the ascending colon, the elimination of bubbles could enhance the ability to detect smaller proximal adenomas. At the same time, the ADR of adenomas less than 5 mm was different with borderline statistical significance. This result may be associated with the small number of patients included. Therefore, additional large clinical trials are necessary to confirm our results.
The presence of bubbles is an important factor that can interfere with mucosal visualization, leading to inadequate bowel preparation. Simethicone is an antifoam agent that not only decreases the amount of bubbles interfering with visualization but also relieves bloating and nausea. Our study is helpful to further improve bowel preparation by providing evidence to support the use of simethicone. In addition, patients in the 3-PS group expressed more willingness to repeat the same bowel preparation. This result seemed to be mainly due to the reduction in the incidence of bloating and nausea and the total fluid volume. Furthermore, split dosing was related to a higher proportion of patients willing to repeat the bowel preparation[8]. These results suggest that 3-PS may be a reliable bowel preparation for screening and surveillance colonoscopy.
Our study has some limitations. First, the study was a single-center trial, and multicenter trials are required to confirm our results. Second, the biochemical parameters after colonoscopy were not evaluated for patients with instability or imbalance. Third, although simethicone might have a positive effect when added to PEG solutions, the effectiveness of different doses of simethicone is still uncertain.
In conclusion, coadministration of simethicone with 3 L split-dose PEG was superior to 4 L PEG, with better bubble elimination and enhanced patient acceptance in bowel preparation. The addition of simethicone offers an excellent potential impact on the detection of proximal adenomas in the Chinese population, indicating that 3 L plus simethicone may be a reliable bowel preparation for screening and surveillance colonoscopy.
The incidence and mortality of colorectal cancer (CRC) have been rapidly increasing in China over the last decade.
A high-quality bowel preparation is a key determinant of the efficacy of colonoscopy to reduce the incidence of CRC, but an ideal bowel cleansing regimen for screening CRC has yet to be determined in a Chinese population.
Explore an ideal bowel cleansing regimen for a colonoscopy.
Bowel-cleansing efficacy was evaluated by endoscopists using the Boston bowel preparation scale (BBPS) and the bubbles score.
The BBPS score of the right-side colon was significantly higher, and significantly more proximal adenomas were detected in the 3 L polyethylene glycol (PEG) plus simethicone (3-PS) group. More patients in the 3-PS group expressed willingness to repeat the bowel preparation.
Three-liter PEG shows satisfactory bowel cleansing and addition of simethicone with better bubble elimination and enhanced patient acceptance offers an excellent potential impact on the detection of proximal adenomas in Chinese populations.
Three-liter plus simethicone may be a reliable bowel preparation for screening and surveillance colonoscopy.
| 1. | Ng SC, Wong SH. Colorectal cancer screening in Asia. Br Med Bull. 2013;105:29-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 2. | Shin A, Kim KZ, Jung KW, Park S, Won YJ, Kim J, Kim DY, Oh JH. Increasing trend of colorectal cancer incidence in Korea, 1999-2009. Cancer Res Treat. 2012;44:219-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 105] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 3. | Meester RG, Doubeni CA, Lansdorp-Vogelaar I, Jensen CD, van der Meulen MP, Levin TR, Quinn VP, Schottinger JE, Zauber AG, Corley DA, van Ballegooijen M. Variation in Adenoma Detection Rate and the Lifetime Benefits and Cost of Colorectal Cancer Screening: A Microsimulation Model. JAMA. 2015;313:2349-2358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, Zauber AG, de Boer J, Fireman BH, Schottinger JE, Quinn VP, Ghai NR, Levin TR, Quesenberry CP. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370:1298-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1251] [Cited by in RCA: 1664] [Article Influence: 138.7] [Reference Citation Analysis (1)] |
| 5. | Johnson DA, Barkun AN, Cohen LB, Dominitz JA, Kaltenbach T, Martel M, Robertson DJ, Boland CR, Giardello FM, Lieberman DA, Levin TR, Rex DK; US Multi-Society Task Force on Colorectal Cancer. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the US multi-society task force on colorectal cancer. Gastroenterology. 2014;147:903-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 320] [Article Influence: 26.7] [Reference Citation Analysis (1)] |
| 6. | Hassan C, East J, Radaelli F, Spada C, Benamouzig R, Bisschops R, Bretthauer M, Dekker E, Dinis-Ribeiro M, Ferlitsch M, Fuccio L, Awadie H, Gralnek I, Jover R, Kaminski MF, Pellisé M, Triantafyllou K, Vanella G, Mangas-Sanjuan C, Frazzoni L, Van Hooft JE, Dumonceau JM. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2019. Endoscopy. 2019;51:775-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 407] [Cited by in RCA: 404] [Article Influence: 57.7] [Reference Citation Analysis (6)] |
| 7. | Chinese Society for Gastrointestinal Endoscopy. Chinese consensus on bowel preparation before endoscopy. Zhonghua Xiaohua Neijing Zazhi. 2013;33:705-707. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Martel M, Barkun AN, Menard C, Restellini S, Kherad O, Vanasse A. Split-Dose Preparations Are Superior to Day-Before Bowel Cleansing Regimens: A Meta-analysis. Gastroenterology. 2015;149:79-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 173] [Article Influence: 15.7] [Reference Citation Analysis (1)] |
| 9. | Zhang S, Li M, Zhao Y, Lv T, Shu Q, Zhi F, Cui Y, Chen M. 3-L split-dose is superior to 2-L polyethylene glycol in bowel cleansing in Chinese population: a multicenter randomized, controlled trial. Medicine (Baltimore). 2015;94:e472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009;69:620-625. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 930] [Cited by in RCA: 988] [Article Influence: 58.1] [Reference Citation Analysis (1)] |
| 11. | Bai Y, Fang J, Zhao SB, Wang D, Li YQ, Shi RH, Sun ZQ, Sun MJ, Ji F, Si JM, Li ZS. Impact of preprocedure simethicone on adenoma detection rate during colonoscopy: a multicenter, endoscopist-blinded randomized controlled trial. Endoscopy. 2018;50:128-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Brahmania M, Ou G, Bressler B, Ko HK, Lam E, Telford J, Enns R. 2 L versus 4 L of PEG3350 + electrolytes for outpatient colonic preparation: a randomized, controlled trial. Gastrointest Endosc 2014; 79: 408-416. e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Citarda F, Tomaselli G, Capocaccia R, Barcherini S, Crespi M; Italian Multicentre Study Group. Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut. 2001;48:812-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 511] [Cited by in RCA: 500] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 14. | Rex DK, Schoenfeld PS, Cohen J, Pike IM, Adler DG, Fennerty MB, Lieb JG 2nd, Park WG, Rizk MK, Sawhney MS, Shaheen NJ, Wani S, Weinberg DS. Quality indicators for colonoscopy. Gastrointest Endosc. 2015;81:31-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 649] [Cited by in RCA: 875] [Article Influence: 79.5] [Reference Citation Analysis (0)] |
| 15. | Froehlich F, Wietlisbach V, Gonvers JJ, Burnand B, Vader JP. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc. 2005;61:378-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 642] [Cited by in RCA: 707] [Article Influence: 33.7] [Reference Citation Analysis (2)] |
| 16. | Clark BT, Protiva P, Nagar A, Imaeda A, Ciarleglio MM, Deng Y, Laine L. Quantification of Adequate Bowel Preparation for Screening or Surveillance Colonoscopy in Men. Gastroenterology. 2016;150:396-405; quiz e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 161] [Article Influence: 16.1] [Reference Citation Analysis (1)] |
| 17. | Chinese Society for Gastrointestinal Endoscopy. Chinese consensus on bowel preparation before endoscopy. Zhonghua Neike Zazhi. 2019;7:485-495. |
| 18. | Kaminski MF, Thomas-Gibson S, Bugajski M, Bretthauer M, Rees CJ, Dekker E, Hoff G, Jover R, Suchanek S, Ferlitsch M, Anderson J, Roesch T, Hultcranz R, Racz I, Kuipers EJ, Garborg K, East JE, Rupinski M, Seip B, Bennett C, Senore C, Minozzi S, Bisschops R, Domagk D, Valori R, Spada C, Hassan C, Dinis-Ribeiro M, Rutter MD. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2017;49:378-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 526] [Article Influence: 58.4] [Reference Citation Analysis (0)] |
| 19. | Corley DA, Levin TR, Doubeni CA. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370:2541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 20. | Rex DK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, Levin TR, Lieberman D, Robertson DJ. Colorectal Cancer Screening: Recommendations for Physicians and Patients From the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017;153:307-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 538] [Article Influence: 59.8] [Reference Citation Analysis (0)] |
| 21. | Yeh JH, Hsu MH, Tseng CM, Chen TH, Huang RY, Lee CT, Lin CW, Wang WL. The benefit of adding oral simethicone in bowel preparation regimen for the detection of colon adenoma: A systematic review and meta-analysis. J Gastroenterol Hepatol. 2019;34:830-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (1)] |
| 22. | Zhang S, Cui Y, Weng Z, Gong X, Chen M, Zhong B. Changes on the disease pattern of primary colorectal cancers in Southern China: a retrospective study of 20 years. Int J Colorectal Dis. 2009;24:943-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Manes G S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Yuan YY