Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3608
Peer-review started: April 8, 2020
First decision: April 28, 2020
Revised: April 29, 2020
Accepted: July 14, 2020
Article in press: July 14, 2020
Published online: August 26, 2020
Processing time: 138 Days and 22.8 Hours
Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) have been widely used for the treatment of early gastrointestinal cancer. Endoscopic piecemeal mucosal resection (EPMR) is derived from the combination of EMR and ESD. Delayed perforation with peritonitis after colonic EPMR is a rare but severe complication, sometimes requiring surgery. There are some associated risk factors, including patient- (location, diameter, and presence of fibrosis) and procedure-related factors. Early recognition and timely treatment are crucial for its management.
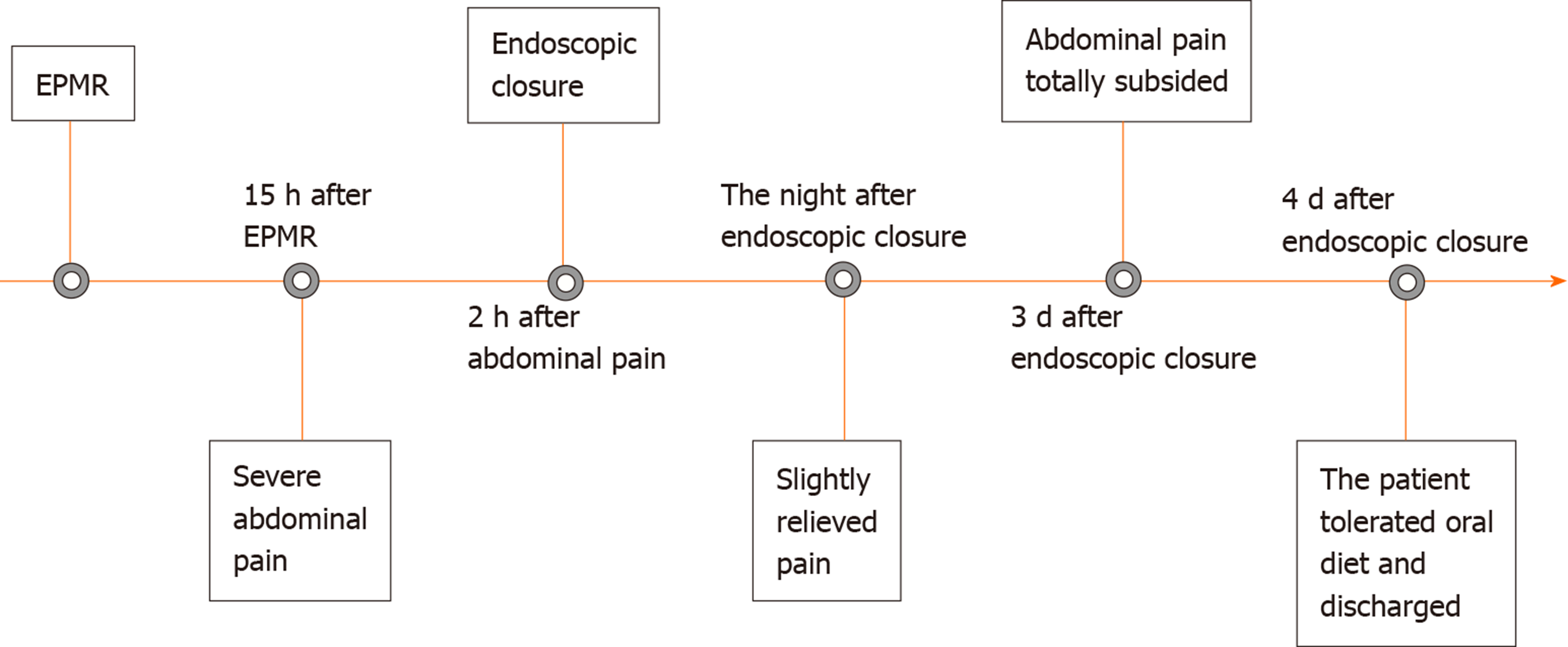
We report a case in which delayed perforation with peritonitis was treated using endoscopic closure. A 54-year-old man was diagnosed with a 30-mm-diameter laterally spreading tumor in the colonic hepatic curvature. Fifteen hours after endoscopic resection, peritonitis caused by delayed perforation occurred and gradually aggravated. Conservative treatment was ineffective and no obvious perforation was observed. After timely endoscopic closure, the patient was discharged on postoperative day 4.
In occasion of localized peritonitis aggravating without macroscopic perforation, endoscopic closure is an effective treatment for delayed perforation with stable vital signs in the early stage.
Core tip: We report a case in which delayed perforation occurred 15 h after colonic endoscopic resection of a laterally spreading tumor in the colonic hepatic curvature. Peritonitis aggravated progressively without macroscopic perforation and conservative treatment had no effect. Micro-perforation was successfully closed under endoscopy with clips to avoid worse complications and surgical intervention.
- Citation: Zhou GYJ, Hu JL, Wang S, Ge N, Liu X, Wang GX, Sun SY, Guo JT. Delayed perforation after endoscopic resection of a colonic laterally spreading tumor: A case report and literature review. World J Clin Cases 2020; 8(16): 3608-3615
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3608.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3608
Endoscopic mucosal resection (EMR) is a common treatment for gastrointestinal mucosal lesions worldwide. Developed on the basis of EMR, endoscopic submucosal dissection (ESD) makes en bloc resection possible and endoscopic piecemeal mucosal resection (EPMR) is suitable for large tumors. Endoscopic therapy requires complicated technology and is associated with a high risk of complications[1]. Perforation is one of the most severe complications; there is both intraoperative perforation and delayed perforation. The latter is often associated with severe systemic symptoms or signs once found; therefore, it requires immediate diagnosis and managements[2].
Here, we report a case in which delayed perforation occurred after colonic endoscopic resection of a laterally spreading tumor (LST) in the hepatic flexure of the colon and peritonitis aggravated progressively. This case is being reported because delayed perforation was identified in a timely fashion and endoscopic closure was performed without macroscopic perforation to avoid worse complications and surgical intervention. We discuss the clinical course of this rare case about micro-perforation and also review the relevant literature.
A 54-year-old man complained of aggravating abdominal pain 15 h after endoscopic resection of a colonic LST.
The patient was referred to our hospital for endoscopic resection of an LST measuring 30 mm that was diagnosed as an adenoma on pathology in the medial side of the colonic hepatic curvature. The patient was placed on a low-fiber diet on the day prior to endoscopic surgery. Adequate bowel preparation (BBPS: 3 points) was achieved using a spilt regimen of 4 L of polyethylene glycol solution and simethicone. During the procedure, our experienced team performed ESD for this lesion at first. When damage to the muscular layer caused by poor scope operability was observed, we changed into EPMR to quickly finish the operation. Prophylactic closure with clips was performed at the damage site. The tumor was removed without residue, and the wound was treated quite well without obvious perforation or hemorrhage. There was no abdominal pain after resection, and the patient was in a good condition. Routine antibiotics and intravenous nutrition were used in consideration of the large mucosal defect. Fifteen hours after endoscopic resection, the patient passed gas and then suddenly experienced severe abdominal pain that aggravated progressively over time without any alleviation.
The patient had a history of diabetes for 10 years without a regular oral hypoglycemic treatment. He had no history of other chronic diseases like cardiovascular disease and hypertension, and no history of trauma, surgery, or blood transfusion. He had no history of food and drug allergy.
The patient occasionally drank alcohol and denied a history of smoking. He had no family history of intestinal tumors.
Physical examination showed intolerable compression pain and rebound pain localized in the right abdomen, suggesting the presence of peritonitis.
Emergency blood analysis showed that neutrophil proportion increased slightly (79.9%) with normal white blood cell count, hemoglobin, and red blood cell count.
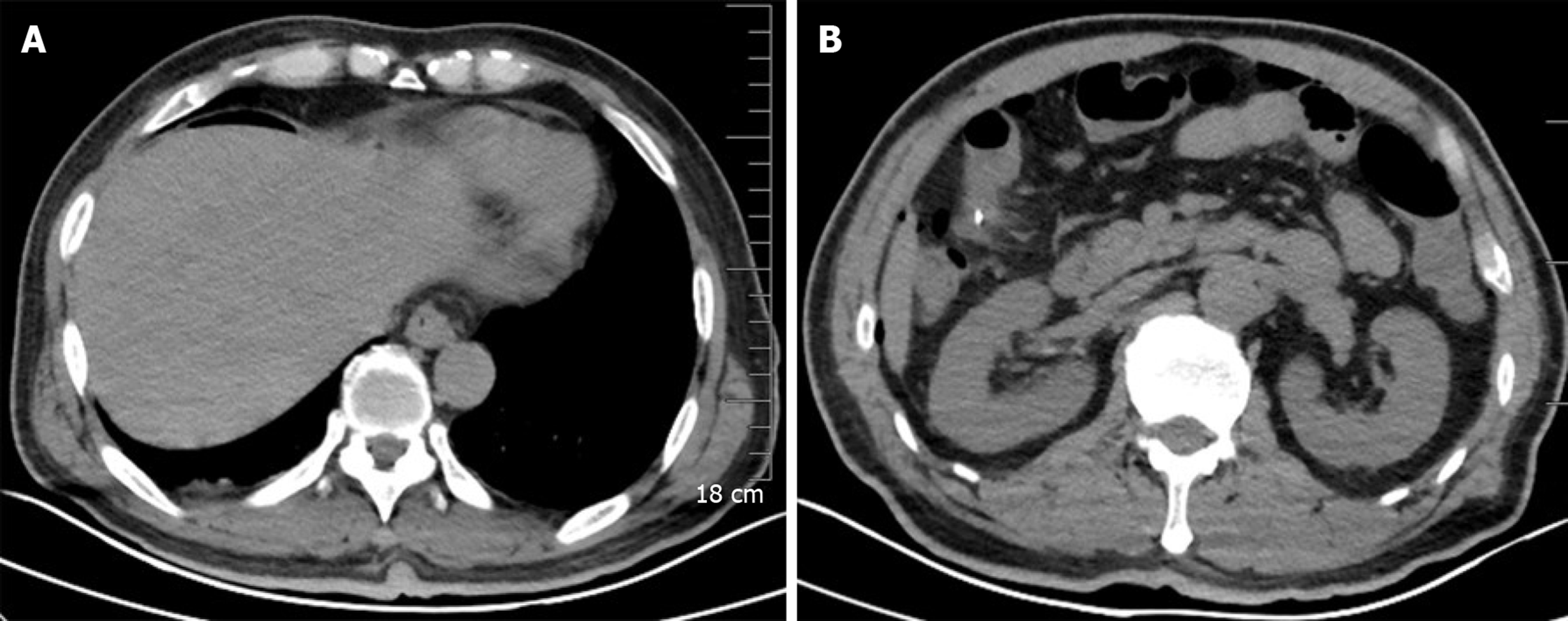
Emergency computed tomography (CT) revealed a small amount of pneumoperitoneum and substantial exudate (Figure 1).
The final diagnosis was a perforation after endoscopic resection.
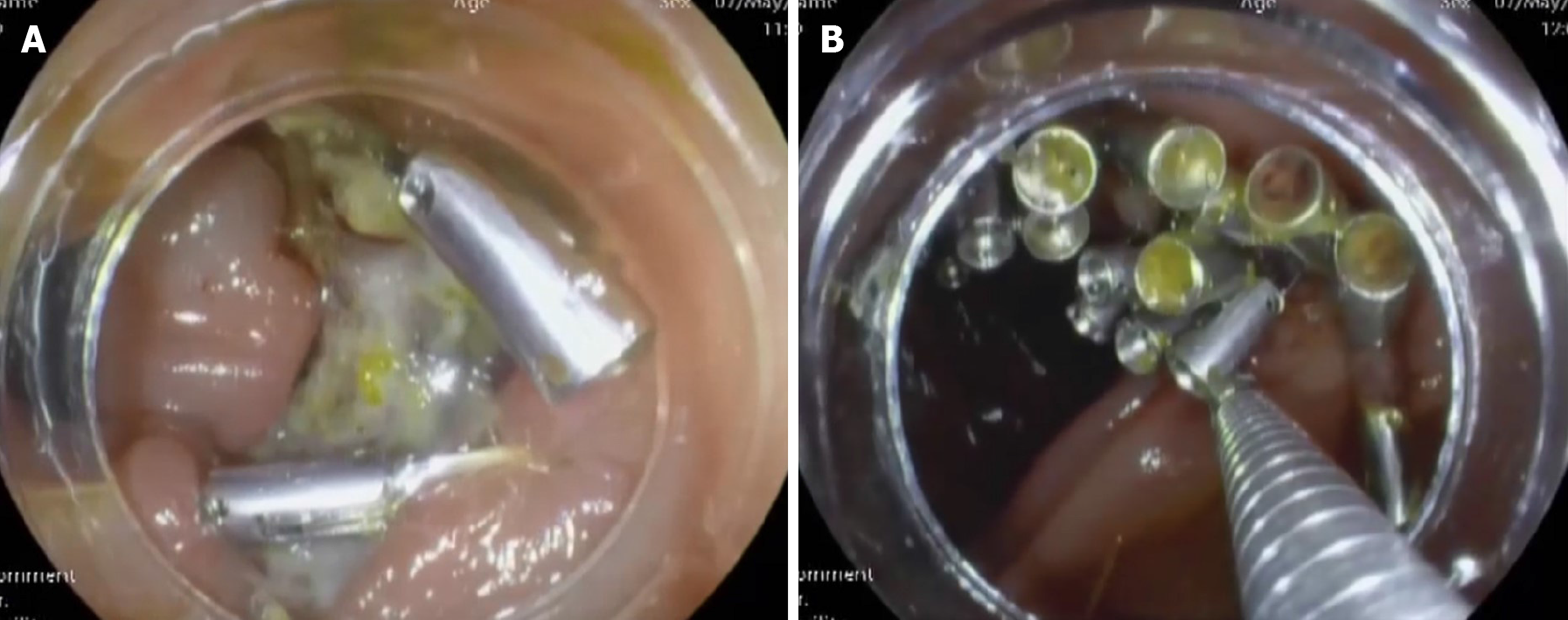
The attempt of placing gastrointestinal decompression did not relieve the symptoms. Emergent colonoscopy with carbon dioxide insufflation was performed. No obvious perforation was observed. We believed that there was a micro-perforation, and the wound was closed using clips (Figure 2). It only took 2 h from the beginning of abdominal pain to achieve successful endoscopic closure. The patient was asked to maintain a semi-recumbent position and was treated with fasting and broad-spectrum antibiotics.
During the night after endoscopic closure, the patient experienced a fever of 38.3°C, but the pain was slightly relieved. Three days after endoscopic closure, the patient’s abdominal pain totally subsided, and after tolerating oral diet, he was discharged on the 4th day after endoscopic closure (Figure 3).
No recurrence occurred in the follow-up. The patient was content with our timely treatment, and informed consent was obtained.
In the present case, delayed perforation occurred 15 h after colonic endoscopic resection of LST in the hepatic flexure of colon. Peritonitis aggravated progressively without obvious perforation and conservative treatment had no effect. Micro-perforation was successfully closed under endoscopy with clips, which had not been reflected in the previous cases ever.
EMR is effective for lesions < 20 mm, and ESD is recommended for lesions > 20 mm with limited submucosal invasion[3]. Nevertheless, there remain no definitive guidelines for treatment of lesions > 20 mm with no invasion or invasion limited in the mucosal layer. We were planning to perform ESD according to anticipatory judgment; however, poor scope operability causing damage to the muscular layer caused us to change to EPMR. Fortunately, no perforation or obvious hemorrhage occurred throughout the procedure, suggesting that our strategy was reasonable.
Perforation is considered one of the most serious complications of therapeutic colonoscopy. Because of intraperitoneal leakage of the intestinal fluid with digestive enzymes and fecal fluid with large amounts of bacteria, peritonitis caused by colorectal perforation is more serious than gastroesophageal perforation[4]. The probability of perforation after ESD is higher than that after EMR, accounting for 1.4%-14.0%[4-6]. Endoscopic perforation is classified as intraoperative and delayed perforation; the latter is even rarer, with reported rates of 0.3%-0.7%[7] and is defined as perforation within 48 h after endoscopic surgery. All previously reported ten cases occurred within 48 h after ESD or EMR[8-12], accompanied by peritonitis of various degrees. Delayed perforation in our case took place in 15 h and caused progressively increasing peritonitis, which is even rarer because of the aggravating peritonitis and our earlier recognition compared with previous case reports.
Several studies have demonstrated that many factors contribute to the occurrence of delayed perforation. Kang et al[13] reported that LSTs were the most common type of lesions causing endoscopic perforation. The most common location was the right colon, including the cecum, ascending colon, and transverse colon, because colonoscopy might be technically complicated there. Of the reported ten cases, 70% occurred in the right colon. The other risk factors include large tumor diameter, presence of fibrosis, and procedure-related factors[7,13]. Our present case is partly consistent with these reports in terms of tumor diameter and tumor location.
The mechanism of immediate colonic perforation is believed to be associated with unintended deep dissection. Delayed perforation is thought to result from thermal injury, that is to say, immoderate thermocoagulation damages both the submucosal and muscular layers, leading to small perforations over time[14,15]. In our present case, neither an obvious perforation nor a small perforation was observed during the subsequent emergent endoscopy. Therefore, we believed that there was a micro-perforation where there was deep dissection or thermal injury of the muscular layer during the procedure.
Several studies have emphasized that prompt and accurate diagnosis is essential for appropriate management and favorable prognosis after delayed perforation[2,15]. Symptoms and signs should be recorded and evaluated carefully. Abdominal pain is one of the earliest and most common symptoms, accompanied by peritoneal irritation signs. Abdominal distention, fever, tachycardia, tachypnea, and subcutaneous emphysema also raise the index of suspicion for delayed perforation. To obtain a definitive diagnosis, plain abdominal radiography or abdominal computed tomography is recommended to detect subdiaphragmatic free air and fluid leak with high accuracy. Laboratory indicators such as complete blood counts are useful to estimate the degree of abdominal contamination. In our case, when perforation was suspected, a CT scan was performed emergently, which finally indicated pneumoperitoneum and exudation, thereby confirming our suspicion.
Currently, there are no guidelines on the management of delayed perforation after colonic endoscopic resection. Delayed perforation after therapeutic colonoscopy is a rare event; however, it is severe, and emergent surgery is the most common treatment for this situation, especially in the context of peritonitis[12]. With the development of endoscopic techniques[11,16-19], timely endoscopic closure may be a good option, if delayed perforation occurs in the patient’s fasting period with local peritonitis. In the present case, although there was no obvious perforation, peritonitis increased over time and conservative treatment was ineffective. Micro-perforation was diagnosed and successfully closed using clips with carbon dioxide insufflation under colonoscopy. Fasting and intravenous broad-spectrum antibiotics were also administered to avoid the need for surgical rescue.
In the English literature, only five other reports (10 cases) of delayed perforation after EMR and ESD with non-surgical management have been reported[8-12] (Table 1). The decision to conduct an endoscopic operation also depends on the perforation size, endoscopist’s experience, and instruments available[2,15,20-23]. During endoscopic closure, carbon dioxide insufflation is generally preferred to prevent barotrauma because this gas is absorbed more quickly than air[24]. Inoki et al[9] reported a case in which delayed perforation after EMR was closed with endoscopic clips. Currently, increasing numbers of endoscopic techniques and equipment have been used. Both through-the-scope-clip and over-the-scope-clip are widely used for endoscopic repair, the former for smaller perforations and the latter for larger ones. Xiao et al[11] demonstrated an endoscopic method called the overtube approach. Nagami et al[10] demonstrated that polyglycolic acid sheets and fibrin glue were effective for endoscopic closure of delayed perforation. Subsequent conservative treatment after closure is indispensable, including fasting, intravenous antibiotics, gastrointestinal decompression, and nutrition support[25]. Kawashima et al[8] described completely conservative treatment, including transnasal decompression, as a method to manage delayed perforation. Nevertheless, not all cases can be treated endoscopically. Delayed perforation with general peritonitis, hemodynamic disorder, and failure in endoscopic closure require immediate surgical treatment[26].
| Ref. | Case | Age (yr) | Sex | Morphology | Location | Tumor diameter (mm) | Endoscopic therapy | Time of delayed perforation (h) | Perforation size (mm) | Treatment | Hospital stay (d) |
| Kawashima et al[8], 2018 | 1 | 66 | Male | LST | Cecum | 40 | ESD | Within 24 | 10 | Transnasal decompression, antibiotics | 26 |
| Inoki et al[9], 2016 | 2 | 73 | Male | LST | Transverse colon | 18 | EMR | Within 24 | NM | Endoscopic closure with clips, antibiotics | 9 |
| Nagami et al[10], 2019 | 3 | 81 | Male | LST | Ascending colon | 40 | ESD | Within 48 | NM | Endoscopic closure with clips, polyglycolic acid sheets and fibrin glue, antibiotics | 16 |
| Xiao et al[11], 2014 | 4 | 49 | Female | LST | Sigmoid colon | NM | ESD | Within 24-48 | 3 | Endoscopic closure with clips, overtube, nasobiliary tube, antibiotics | 29 |
| Xiao et al[11], 2014 | 5 | 77 | Male | LST | Ascending colon | NM | ESD | Within 24-48 | 6 | Endoscopic closure with clips, overtube, nasobiliary tube, antibiotics | 12 |
| Xiao et al[11], 2014 | 6 | 41 | Female | Polyp | Transverse colon | NM | EMR | Within 24-48 | 5 | Endoscopic closure with clips, overtube, nasobiliary tube, antibiotics | 7 |
| Iwatsubo et al[12], 2019 | 7 | 45 | Male | Protruded | Descending colon | 10 | ESD | 24 | NM | Conservative therapy, antibiotics | 13 |
| Iwatsubo et al[12], 2019 | 8 | 53 | Male | Flat | Transverse colon | 22 | ESD | 19 | NM | Conservative therapy, antibiotics | 12 |
| Iwatsubo et al[12], 2019 | 9 | 74 | Female | Protruded | Rectum | 110 | ESD | 14 | NM | Conservative therapy, antibiotics | 14 |
| Iwatsubo et al[12], 2019 | 10 | 58 | Male | Protruded | Ascending colon | 55 | ESD | 24 | NM | Conservative therapy, antibiotics | 13 |
Delayed perforation with peritonitis after endoscopic operation is an uncommon but serious complication. Endoscopists should operate carefully throughout the procedure, especially for LSTs in the right colon. If delayed perforation occurs and localized peritonitis exacerbates, even without macroscopic perforation, endoscopic closure is an alternative for patients with stable vital signs in the early stage.
| 1. | Hong SN, Byeon JS, Lee BI, Yang DH, Kim J, Cho KB, Cho JW, Jang HJ, Jeon SW, Jung SA, Chang DK. Prediction model and risk score for perforation in patients undergoing colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2016;84:98-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 2. | Paspatis GA, Dumonceau JM, Barthet M, Meisner S, Repici A, Saunders BP, Vezakis A, Gonzalez JM, Turino SY, Tsiamoulos ZP, Fockens P, Hassan C. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2014;46:693-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 190] [Article Influence: 15.8] [Reference Citation Analysis (1)] |
| 3. | Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 817] [Cited by in RCA: 956] [Article Influence: 86.9] [Reference Citation Analysis (0)] |
| 4. | Taku K, Sano Y, Fu KI, Saito Y, Matsuda T, Uraoka T, Yoshino T, Yamaguchi Y, Fujita M, Hattori S, Ishikawa T, Saito D, Fujii T, Kaneko E, Yoshida S. Iatrogenic perforation associated with therapeutic colonoscopy: a multicenter study in Japan. J Gastroenterol Hepatol. 2007;22:1409-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Saito Y, Fukuzawa M, Matsuda T, Fukunaga S, Sakamoto T, Uraoka T, Nakajima T, Ikehara H, Fu KI, Itoi T, Fujii T. Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc. 2010;24:343-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 438] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 6. | Tamegai Y, Saito Y, Masaki N, Hinohara C, Oshima T, Kogure E, Liu Y, Uemura N, Saito K. Endoscopic submucosal dissection: a safe technique for colorectal tumors. Endoscopy. 2007;39:418-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 202] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 7. | Isomoto H, Nishiyama H, Yamaguchi N, Fukuda E, Ishii H, Ikeda K, Ohnita K, Nakao K, Kohno S, Shikuwa S. Clinicopathological factors associated with clinical outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy. 2009;41:679-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 162] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 8. | Kawashima K, Hikichi T, Fujiwara T, Gunji N, Nakamura J, Watanabe K, Katakura K, Ohira H. Delayed perforation after endoscopic submucosal dissection for mucosal colon cancer: A conservatively treated case. Fukushima J Med Sci. 2018;64:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Inoki K, Sakamoto T, Sekiguchi M, Yamada M, Nakajima T, Matsuda T, Saito Y. Successful endoscopic closure of a colonic perforation one day after endoscopic mucosal resection of a lesion in the transverse colon. World J Clin Cases. 2016;4:238-242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Nagami Y, Fukunaga S, Kanamori A, Sakai T, Ominami M, Watanabe T, Fujiwara Y. Endoscopic closure using polyglycolic acid sheets for delayed perforation after colonic endoscopic submucosal dissection. Endoscopy. 2020;52:E11-E12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Xiao YF, Bai JY, Yu J, Lin XL, Zhao XY, Yang SM, Fan CQ. Endoscopic treatment of delayed colon perforation: the enteroscopy overtube approach. Endoscopy. 2014;46:503-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Iwatsubo T, Takeuchi Y, Yamasaki Y, Nakagawa K, Arao M, Ohmori M, Iwagami H, Matsuno K, Inoue S, Nakahira H, Matsuura N, Shichijo S, Maekawa A, Kanesaka T, Yamamoto S, Higashino K, Uedo N, Ishihara R. Differences in Clinical Course of Intraprocedural and Delayed Perforation Caused by Endoscopic Submucosal Dissection for Colorectal Neoplasms: A Retrospective Study. Dig Dis. 2019;37:53-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Kang DU, Choi Y, Lee HS, Lee HJ, Park SH, Yang DH, Yoon SM, Kim KJ, Ye BD, Myung SJ, Yang SK, Kim JH, Byeon JS. Endoscopic and Clinical Factors Affecting the Prognosis of Colorectal Endoscopic Submucosal Dissection-Related Perforation. Gut Liver. 2016;10:420-428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Ko YB, Lee JM, Kim WS, Kwak MS, Lee JW, Shin DY, Yang DH, Byeon JS. Unexpected Delayed Colon Perforation after the Endoscopic Submucosal Dissection with Snaring of a Laterally Spreading Tumor. Clin Endosc. 2015;48:570-575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Alsowaina KN, Ahmed MA, Alkhamesi NA, Elnahas AI, Hawel JD, Khanna NV, Schlachta CM. Management of colonoscopic perforation: a systematic review and treatment algorithm. Surg Endosc. 2019;33:3889-3898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Nunes G, Marques PP, Patita M, Allen M, Gargaté L. EUS-guided recanalization of complete colorectal anastomotic stenosis using a lumen-apposing metal stent. Endosc Ultrasound. 2019;8:211-212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Guo J, Sun S. EUS-guided gallbladder drainage and gallbladder interventions in China. Endosc Ultrasound. 2018;7:83-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 18. | Wang G, Liu X, Wang S, Ge N, Guo J, Sun S. Endoscopic Ultrasound-guided Gastroenterostomy: A Promising Alternative to Surgery. J Transl Int Med. 2019;7:93-99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Theerasuwipakorn N, Tasneem AA, Kongkam P, Angsuwatcharakon P, Ridtitid W, Navicharern P, Kitisin K, Wangrattanapranee P, Rerknimitr R, Kullavanijaya P. Walled-off Peripancreatic Fluid Collections in Asian Population: Paradigm Shift from Surgical and Percutaneous to Endoscopic Drainage. J Transl Int Med. 2019;7:170-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | de'Angelis N, Di Saverio S, Chiara O, Sartelli M, Martínez-Pérez A, Patrizi F, Weber DG, Ansaloni L, Biffl W, Ben-Ishay O, Bala M, Brunetti F, Gaiani F, Abdalla S, Amiot A, Bahouth H, Bianchi G, Casanova D, Coccolini F, Coimbra R, de'Angelis GL, De Simone B, Fraga GP, Genova P, Ivatury R, Kashuk JL, Kirkpatrick AW, Le Baleur Y, Machado F, Machain GM, Maier RV, Chichom-Mefire A, Memeo R, Mesquita C, Salamea Molina JC, Mutignani M, Manzano-Núñez R, Ordoñez C, Peitzman AB, Pereira BM, Picetti E, Pisano M, Puyana JC, Rizoli S, Siddiqui M, Sobhani I, Ten Broek RP, Zorcolo L, Carra MC, Kluger Y, Catena F. 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation. World J Emerg Surg. 2018;13:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 21. | Sun S, Wang C, Wang S. Remember, interventional EUS is performed using an elevator-containing scope as well. Endosc Ultrasound. 2018;7:73-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 22. | Ge N, Hu J, Sun S, Linghu E, Jin Z, Li Z. Endoscopic Ultrasound-guided Pancreatic Pseudocyst Drainage with Lumen-apposing Metal Stents or Plastic Double-pigtail Stents: A Multifactorial Analysis. J Transl Int Med. 2017;5:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Ge N, Sun S. Endoscopic ultrasound: An all in one technique vibrates virtually around the whole internal medical field. J Transl Intern Med. 2014;2:104-106. |
| 24. | Dellon ES, Hawk JS, Grimm IS, Shaheen NJ. The use of carbon dioxide for insufflation during GI endoscopy: a systematic review. Gastrointest Endosc. 2009;69:843-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 113] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 25. | Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, Hisabe T, Yao T, Watanabe M, Yoshida M, Kudo SE, Tsuruta O, Sugihara KI, Watanabe T, Saitoh Y, Igarashi M, Toyonaga T, Ajioka Y, Ichinose M, Matsui T, Sugita A, Sugano K, Fujimoto K, Tajiri H. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015;27:417-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 456] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 26. | Cho SB, Lee WS, Joo YE, Kim HR, Park SW, Park CH, Kim HS, Choi SK, Rew JS. Therapeutic options for iatrogenic colon perforation: feasibility of endoscopic clip closure and predictors of the need for early surgery. Surg Endosc. 2012;26:473-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Coffin CS, Kato M S-Editor: Wang JL L-Editor: Wang TQ P-Editor: Liu JH