Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3601
Peer-review started: March 3, 2020
First decision: April 24, 2020
Revised: May 27, 2020
Accepted: July 16, 2020
Article in press: July 16, 2020
Published online: August 26, 2020
Processing time: 175 Days and 0.4 Hours
Coronary artery spasm is a major cause of myocardial ischemia. Although coronary artery spasm has been known for a long time, its mechanism has not yet been identified. Many clinicians, especially young clinicians pay less attention to coronary artery spasm, which may lead to some patients not being appropriately diagnosed and treated in time. We report a patient with spontaneous multivessel coronary artery spasm for more than 30 years diagnosed with intravascular ultrasound (IVUS) imaging.
A 66-year-old Chinese male patient had chest squeezing at rest for more than 30 years. He had a history of cigarette smoking for more than 40 years and hypertension for 10 years. Before presenting at our institution, the patient had undergone coronary angiography 4 times and percutaneous transluminal coronary angioplasty procedures twice at other hospitals without a diagnosis of coronary artery spasm. However, his chest symptoms worsened. Spontaneous multivessel coronary artery spasm occurred during IVUS without provocation testing, and the IVUS image was recorded. Thus, the diagnosis of multifocal spontaneous coronary artery spasm was confirmed. The patient was placed on oral diltiazem, isosorbide mononitrate, and nicorandil to suppress coronary artery spasms. All medications were given at the maximum dosages tolerated by the patient. He was discharged after 5 d without complications. During the six-month follow-up period, the patient was symptom-free.
Coronary artery spasm is still prevalent in Eastern countries. It is essential for clinicians to be aware of coronary artery spasm, which may be hard to detect and can be lethal, in order to diagnose and treat patients appropriately.
Core tip: Coronary artery spasm is an important cause of myocardial ischemia. Although coronary artery spasm has been known for a long time, its mechanisms have not yet been identified. Coronary artery spasm is prevalent in Asian countries, but many clinicians, especially young clinicians, pay less attention to coronary artery spasm, which may result in misdiagnosis and mistreatment. It is essential for clinicians to be aware of coronary artery spasm, which may be hard to detect but can be lethal, in order to diagnose and treat patients appropriately.
- Citation: Wu HY, Cao YW, Chang FJ, Liang L. Spontaneous multivessel coronary artery spasm diagnosed with intravascular ultrasound imaging: A case report. World J Clin Cases 2020; 8(16): 3601-3607
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3601.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3601
Coronary artery spasm is an important cause of myocardial ischemia. It may be associated with the pathogenesis of several cardiac diseases including sudden cardiac death, angina pectoris, acute myocardial infarction, fatal arrhythmias, and other diseases[1]. Coronary artery spasm is thought to result from endothelin dysfunction, which impairs vasodilatation. However, under rare conditions, it may relate to multiple coronary vessels, and medical treatments may be ineffective. Variant angina is a discrete form of angina pectoris, which typically occurs during normal activity or at rest, without evident classical triggers such as exercise. In this syndrome, episodes usually occur at night or in the early hours of the morning[2]. The diagnosis of variant angina can be challenging and it can easily be mistaken for diffuse coronary artery disease.
Previous intravascular ultrasound (IVUS) and optical coherence tomography (OCT) studies have reported the morphological features of vasospastic lesions[3,4]. However, most of the data were obtained in a spastic lesion that was artificially induced by the administration of acetylcholine or ergonovine. In this report, we present the case of a 66-year-old male who had chest symptoms at rest for more than 30 years. Before presenting at our institution, the patient had undergone coronary angiography 4 times and percutaneous transluminal coronary angioplasty procedures twice at other hospitals without a diagnosis of coronary artery spasm. However, his chest symptoms worsened. Spontaneous multivessel coronary artery spasm occurred during IVUS without provocation testing, and the IVUS image was recorded.
A 66-year-old male had chest squeezing at rest for more than 30 years.
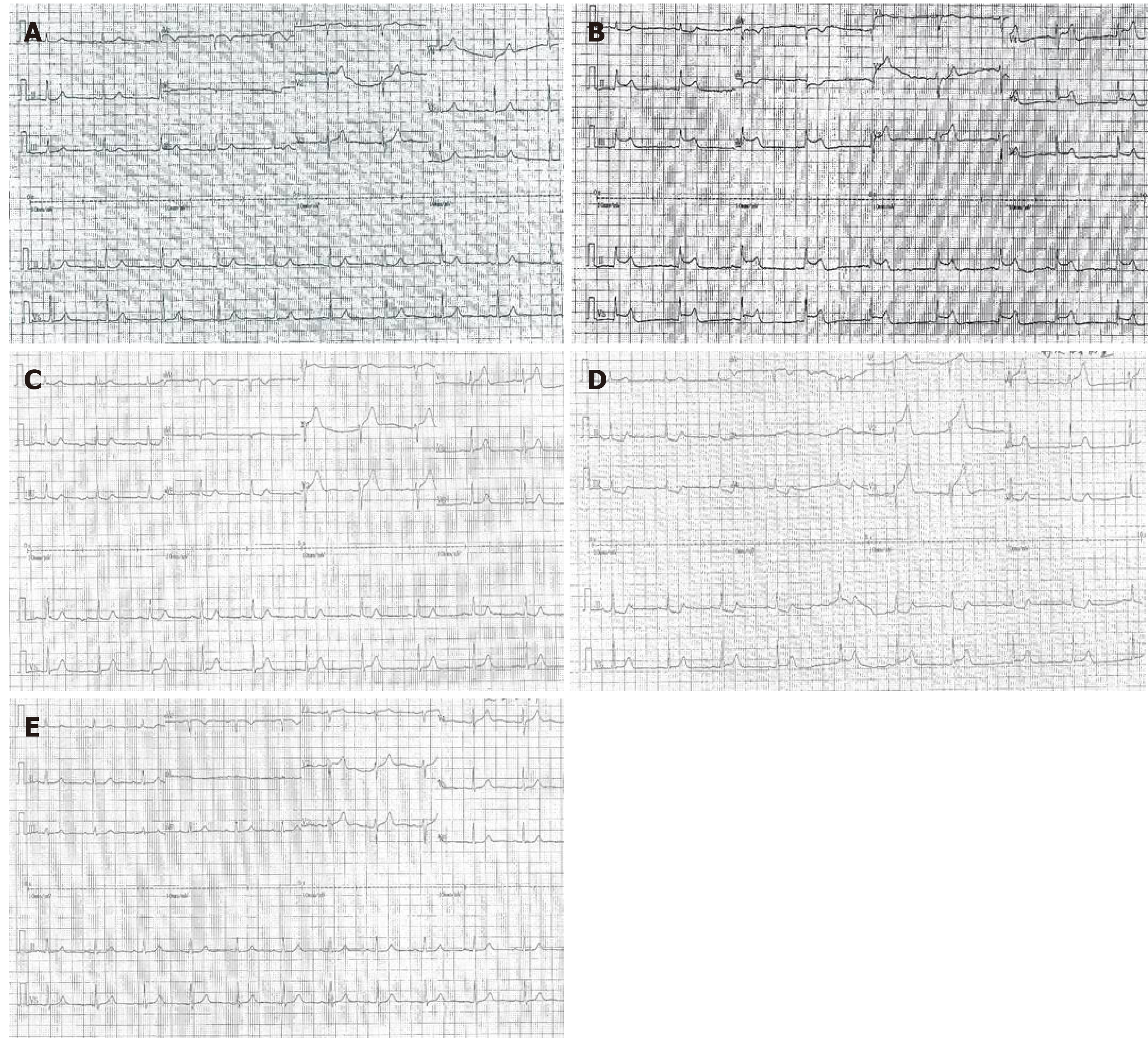
Thirty years ago, the patient had chest squeezing at rest which occurred most often from midnight to early morning lasting from 5 to 15 min, and was not usually induced by exercise in the daytime. Over the preceding 13 years, he had undergone coronary angiography 4 times and percutaneous transluminal coronary angioplasty procedures twice at other hospitals without a diagnosis of coronary artery spasm. In July 2006, 70% stenosis was found in the ostial left anterior descending artery and 90% stenosis was found in the mid left circumflex. The left circumflex was dilated by balloon without a stent as the left circumflex was small according to the previous angiography report. The patient was given various medications, such as beta blocker, aspirin, angiotensin-converting-enzyme inhibitor, clopidogrel, and statin, but his chest symptoms were not relieved. Due to repeated similar complaints, angiography was performed again without percutaneous transluminal coronary angioplasty in November 2014 and August 2015. In August 2017, an electrocardiography was performed during a chest squeezing episode in the early morning at 6:08 in a hospital and ST-segment elevations in II, III, aVF and V2-V5 leads were observed. Subsequently, ST-segment depression in II, III and aVF, and ST-segment elevation in V2-V5 leads became apparent. The symptoms and ST-segment elevation or depression disappeared 3 min and 25 s after sublingual administration of nitroglycerin (Figure 1). However, the doctors did not realize that the symptoms were caused by coronary artery spasm. Coronary angiography was performed and showed severe stenosis in the proximal left circumflex which was dilated by balloon again without a stent. However, his chest symptoms occurred approximately 5 times/mo. The patient presented to the emergency room of our hospital with frequent chest squeezing episodes in March 2019.
The patient had a history of hypertension for 10 years.
The patient had a history of cigarette smoking for more than 40 years.
No family history of inherited diseases, autoimmune diseases or coronary heart disease was recorded.
Vital signs were stable and physical examination was unremarkable.
No elevation in high sensitivity troponin T was detected and the rest of his laboratory examinations were also completely normal.
Electrocardiography was performed during a chest pain episode and ST-segment elevations in I, aVL and V2-V3 leads were recorded which spontaneously resolved, accompanied by pain relief (Figure 2). Neither chest X-ray nor echocardiography showed any specific changes.
In order to evaluate the condition of the coronary artery, coronary angiography and IVUS were performed. An injection of acetylcholine into the coronary artery was administered to induce spasm. Coronary angiography was performed via right radial access. Intravenous injection of diltiazem and intracoronary injection of nitroglycerin were administered to prevent coronary artery spasm induced by the catheter or guidewire.
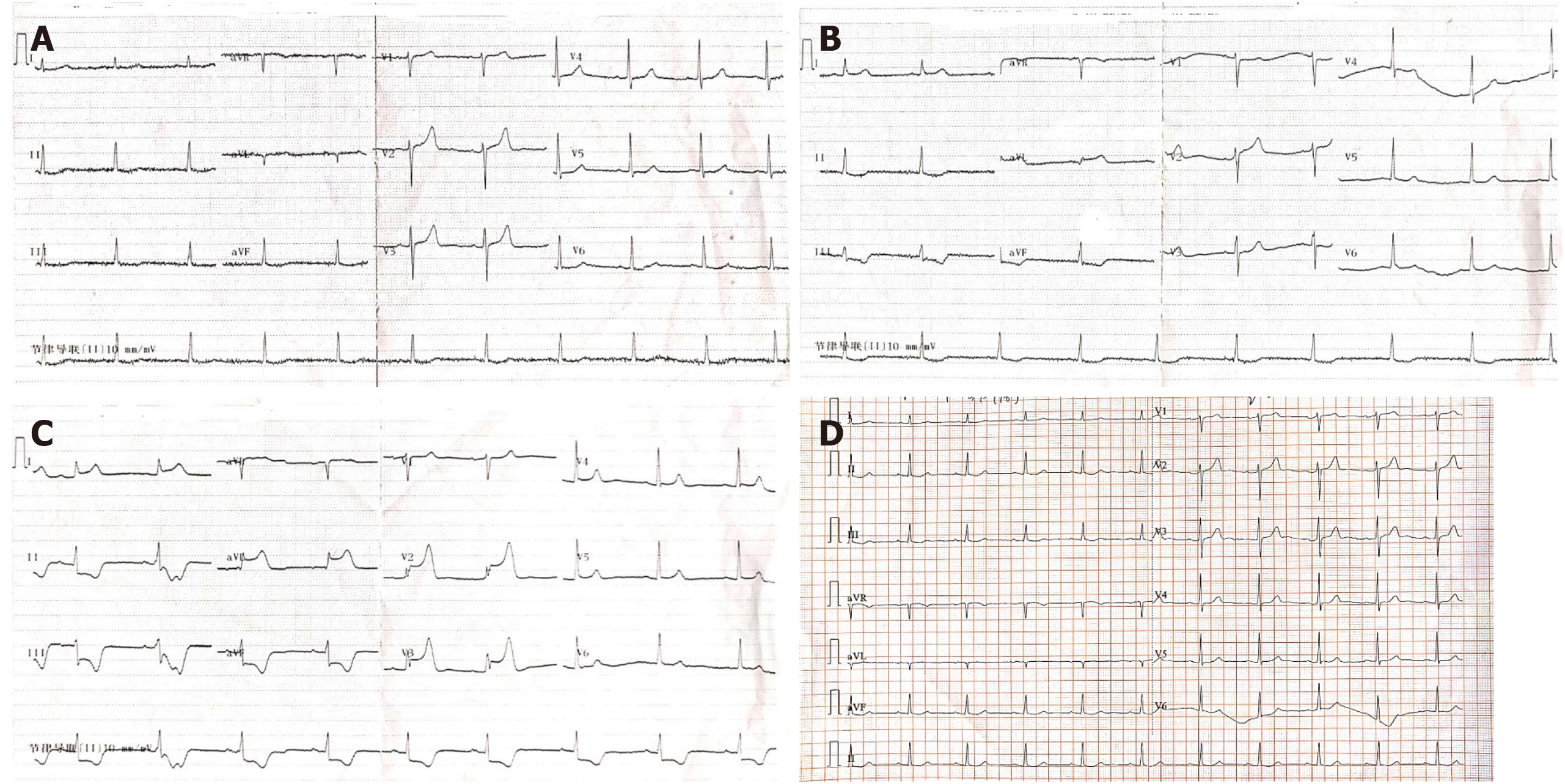
An initial coronary angiography showed mild atherosclerotic changes from the proximal to the mid segment in the right coronary artery. There were no obvious atherosclerotic changes in the left main trunk, left anterior descending coronary artery and left circumflex (Figure 3).
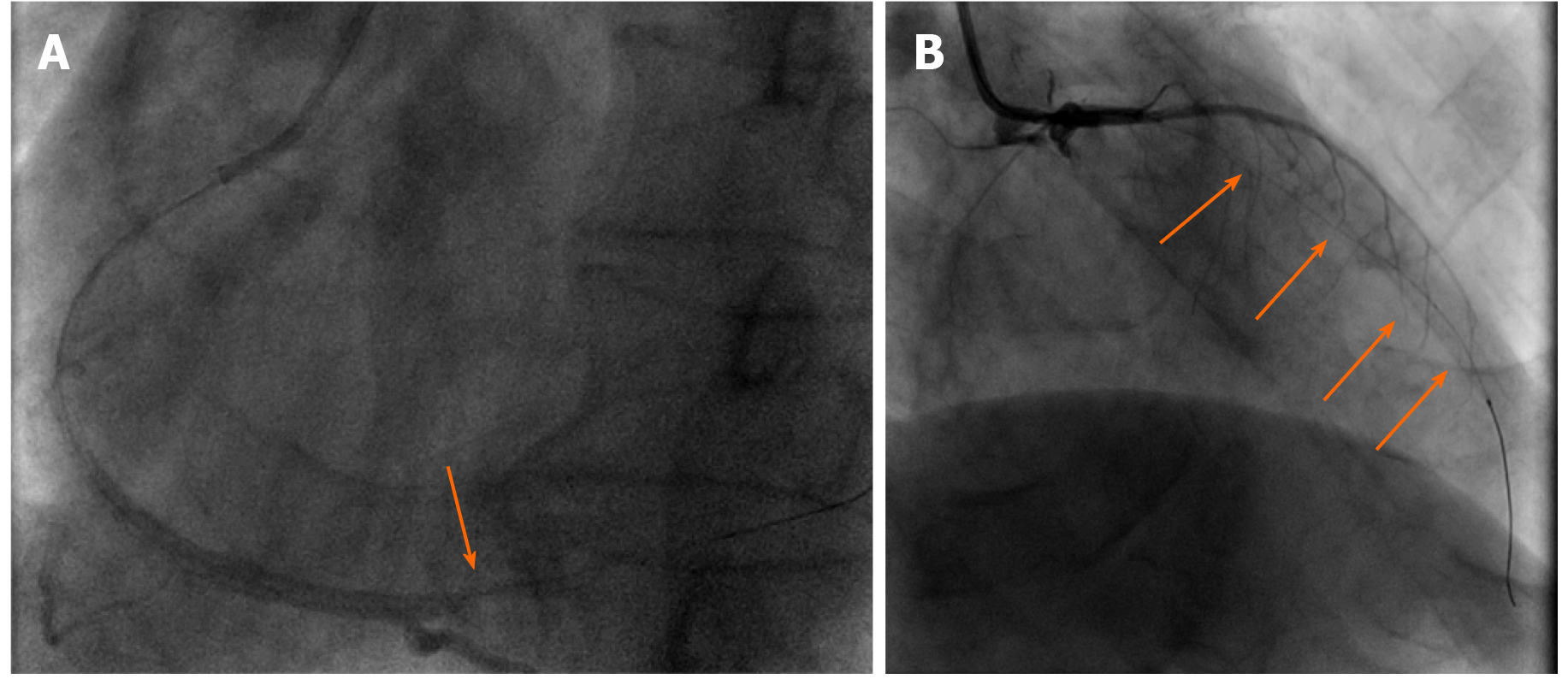
After intracoronary injection of 200 μg of nitroglycerin, each segment was examined using a mechanical IVUS system. During IVUS checking of the right coronary artery and left anterior descending coronary artery, the patient felt chest squeezing without the use of acetylcholine or ergonovine. Coronary angiography showed that a local coronary spasm occurred at the distal segment of the right coronary artery and a diffuse coronary spasm occurred at the proximal-distal segment of the left anterior descending coronary artery (Figure 4). Following an intracoronary injection of nitroglycerin (right coronary artery with 400 μg nitroglycerin and left coronary artery with 1000 μg nitroglycerin), the patient’s chest symptoms and coronary spasm were relieved (Figure 5).
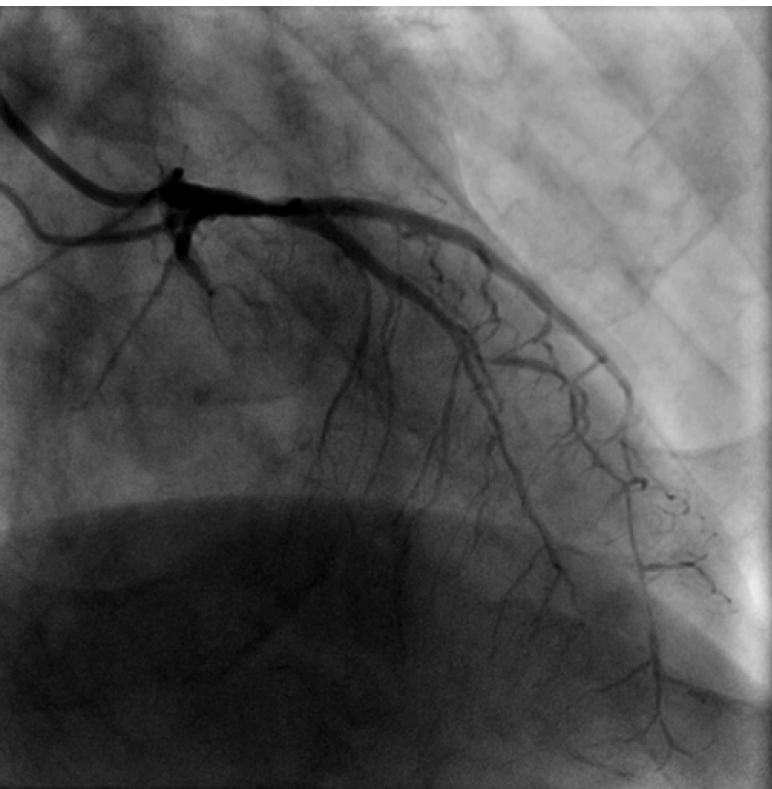
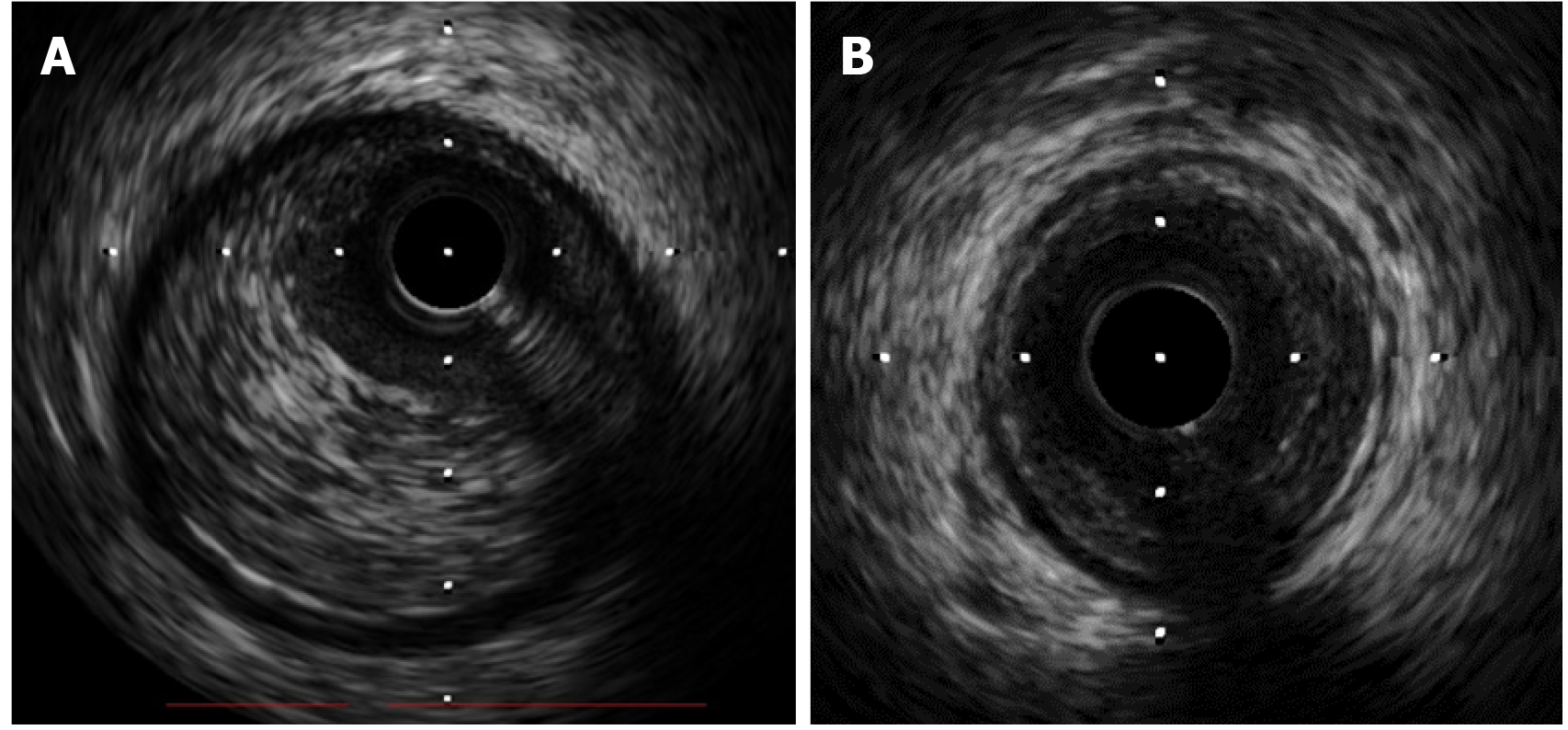
IVUS images showed that the right coronary artery and left anterior descending coronary artery demonstrated increased media thickness (Figure 6).
The diagnosis of multifocal spontaneous coronary artery spasm was confirmed.
Beta blocker was discontinued. The patient was placed on oral diltiazem, isosorbide mononitrate, and nicorandil to suppress coronary artery spasms. All medications were given at the maximum dosages tolerated by the patient.
The patient was discharged after 5 d without complications. During the six-month follow-up period, the patient was symptom-free.
We present the case of a patient with angina pectoris at rest for more than 30 years. According to electrocardiography at onset of chest symptoms, ST elevations were observed in the precordial (V2-V5), inferior (II, III, aVF) and lateral (I, aVL) leads. Before being diagnosed with variant angina at our hospital, the patient had undergone coronary angiography 4 times and percutaneous transluminal coronary angioplasty procedures twice at other hospitals without IVUS, OCT or fractional flow reserve. Spontaneous multivessel coronary artery spasm occurred during IVUS without provocation testing, and the IVUS image was recorded at our hospital. The patient was placed on oral diltiazem, isosorbide mononitrate, and nicorandil to suppress coronary artery spasms. The patient was free of symptoms during the six-month follow-up period. Thus, the diagnosis of multifocal spontaneous coronary artery spasm was confirmed.
IVUS and OCT studies have reported the morphological features of vasospastic lesions. However, most of the data were obtained in a spastic lesion that was artificially induced by the administration of acetylcholine or ergonovine. In the present study, spontaneous multivessel coronary artery spasm occurred during IVUS without provocation testing, and the IVUS image was recorded. Tanaka A used provocation testing to assess coronary artery spasm with OCT. The results showed that the spasm lesion demonstrated an increased maximum media thickness[3]. Our patient also showed increased media thickness in the spastic coronary artery.
Coronary artery spasm is mainly a disease of middle-aged and elderly men. Smoking is a significant risk factor for coronary artery spasm. Our patient with multifocal spontaneous coronary artery spasm had a history of cigarette smoking for more than 40 years. A significantly higher proportion of patients with coronary artery spasm angina are smokers than those with stable effort angina, suggesting that the pathogenesis of coronary artery spasm may be different to the pathogenesis of coronary atherosclerosis. As cigarette smoking is an important risk factor for coronary artery spasm, a high smoking rate may be one of the factors associated with the high incidence of coronary artery spasm in Asian countries (e.g., Japan)[5].
Although obstructive coronary artery disease is frequently considered to be the cause of symptoms, vasospasm should be considered in some clinical settings[6]. Many conventional drugs are ineffective in patients with coronary artery spasm and this may result in fatal arrhythmia or sudden death. It is essential for clinicians to be aware of coronary artery spasm, which may be hard to detect but can be fatal. Further studies are required to determine the pathogenesis of coronary artery spasm and develop more effective and long-lasting treatments for this disease.
| 1. | Sueda S. Young Vasospastic Angina Patients Less Than 20 Years Old. Circ J. 2019;83:1925-1928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Iranirad L, Sadeghi MS. A rare case of spontaneous and simultaneous multivessel coronary artery spasm leading to multisite myocardial infarction and ventricular fibrillation. ARYA Atheroscler. 2018;14:41-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 3. | Tanaka A, Shimada K, Tearney GJ, Kitabata H, Taguchi H, Fukuda S, Kashiwagi M, Kubo T, Takarada S, Hirata K, Mizukoshi M, Yoshikawa J, Bouma BE, Akasaka T. Conformational change in coronary artery structure assessed by optical coherence tomography in patients with vasospastic angina. J Am Coll Cardiol. 2011;58:1608-1613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Tsujita K, Sakamoto K, Kojima S, Kojima S, Takaoka N, Nagayoshi Y, Sakamoto T, Tayama S, Kaikita K, Hokimoto S, Sumida H, Sugiyama S, Nakamura S, Ogawa H. Coronary plaque component in patients with vasospastic angina: a virtual histology intravascular ultrasound study. Int J Cardiol. 2013;168:2411-2415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Takaoka K, Yoshimura M, Ogawa H, Kugiyama K, Nakayama M, Shimasaki Y, Mizuno Y, Sakamoto T, Yasue H. Comparison of the risk factors for coronary artery spasm with those for organic stenosis in a Japanese population: role of cigarette smoking. Int J Cardiol. 2000;72:121-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 78] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Li D, Li Y, Wang X, Wu Y, Cui XY, Hu JQ, Li B, Lin Q. Diagnosis of myocardial infarction with nonobstructive coronary arteries in a young man in the setting of acute myocardial infarction after endoscopic retrograde cholangiopancreatography: A case report. World J Clin Cases. 2019;7:3062-3068. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Falconi M S-Editor: Zhang L L-Editor: Webster JR P-Editor: Li JH