Published online Aug 26, 2020. doi: 10.12998/wjcc.v8.i16.3616
Peer-review started: March 21, 2020
First decision: April 22, 2020
Revised: May 6, 2020
Accepted: July 17, 2020
Article in press: July 17, 2020
Published online: August 26, 2020
Processing time: 156 Days and 20.5 Hours
We report a rare case of first branchial cleft anomaly (FBCA) accompanied by bony atresia of the external auditory canal, middle ear malformation, and location malformation of the facial nerve according to the intraoperative findings.
A 19-year-old male patient presented to our department with a mass behind the right earlobe and recurrent postauricular swelling and pain since childhood, he also had severe hearing loss in the right ear since birth. The patient underwent surgery including mass removal, mastoidectomy, and simultaneous meatoplasty and ossiculoplasty under microscopy. No facial palsy or recurrence was noted during postoperative follow-up.
FBCAs are rare, and to our knowledge, this is the first report of FBCA accompanied by external auditory canal bony atresia, middle ear malformation, and location malformation of the facial nerve. An effective postauricular approach under microscopy facilitated complete lesion removal and simultaneous otologic reconstruction.
Core tip: We report a rare case of first branchial cleft anomaly accompanied by bony atresia of the external auditory canal, middle ear malformation, and location malformation of the facial nerve according to the intraoperative findings. An effective treatment strategy including lesion excision, mastoidectomy, and simultaneous meatoplasty and ossiculoplasty was undertaken, which achieved a satisfactory outcome.
- Citation: Zhang CL, Li CL, Chen HQ, Sun Q, Liu ZH. First branchial cleft cyst accompanied by external auditory canal atresia and middle ear malformation: A case report. World J Clin Cases 2020; 8(16): 3616-3620
- URL: https://www.wjgnet.com/2307-8960/full/v8/i16/3616.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i16.3616
First branchial cleft anomalies (FBCAs) are rare, accounting for less than 8% of all branchial anomalies in the head and neck. FBCAs are usually classified as cysts, sinuses, and fistulas according to the clinical features[1,2]. In a few cases, FBCAs are accompanied by microtia, stenosis or atresia of the external auditory canal (EAC), and cholesteatoma[3-6]. In this study, we report a case of FBCA accompanied by bony atresia of the EAC, middle ear malformation, as well as location malformation of the facial nerve (FN) according to the intraoperative findings. To our knowledge, this is the first report of such a complex case. An effective treatment strategy including lesion excision, mastoidectomy, and simultaneous meatoplasty and ossiculoplasty under microscopy was undertaken, which achieved a satisfactory outcome. As the cyst was closely related to the FN, we performed the cystectomy with complete preservation of the parotid gland under the microscope to better protect the FN.
A 19-year-old male patient presented to our department in June 2019, with a mass behind the right earlobe and recurrent postauricular swelling and pain since childhood. He received abscess incision drainage three times in a local hospital. The patient also had severe hearing loss in the right ear since birth.
The patient had a mass behind the right earlobe and recurrent postauricular swelling and pain since childhood.
The patient had no other previous medical history.
A 2 cm × 3 cm fluctuant and tender mass in the postauricular area, and bony atresia of the EAC were observed.
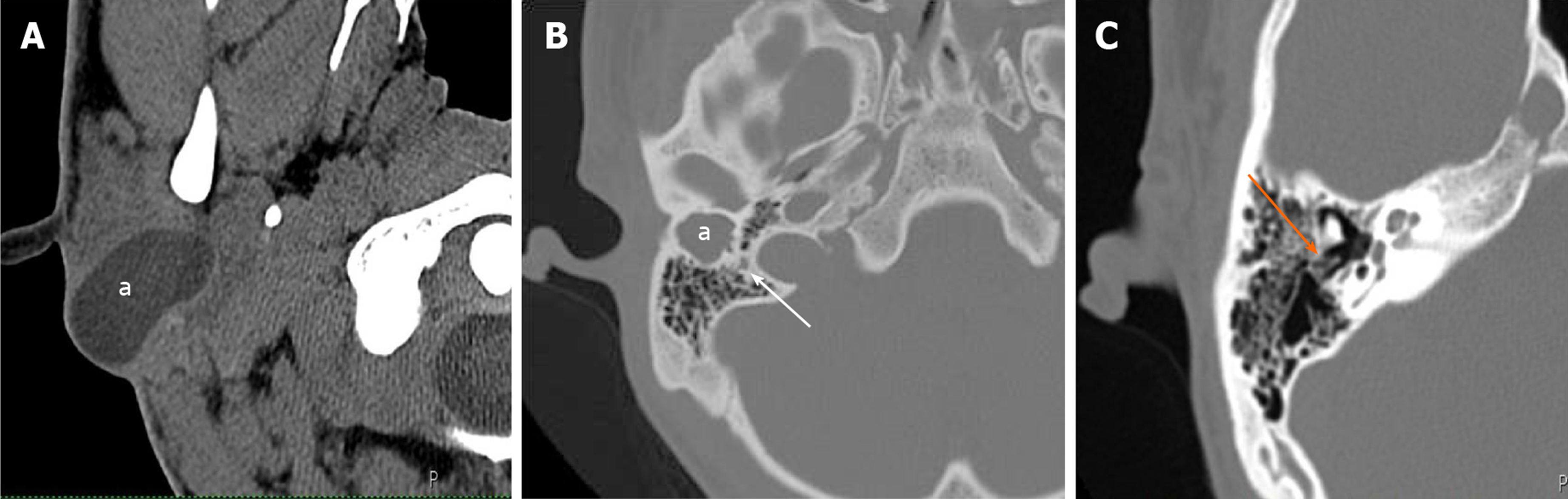
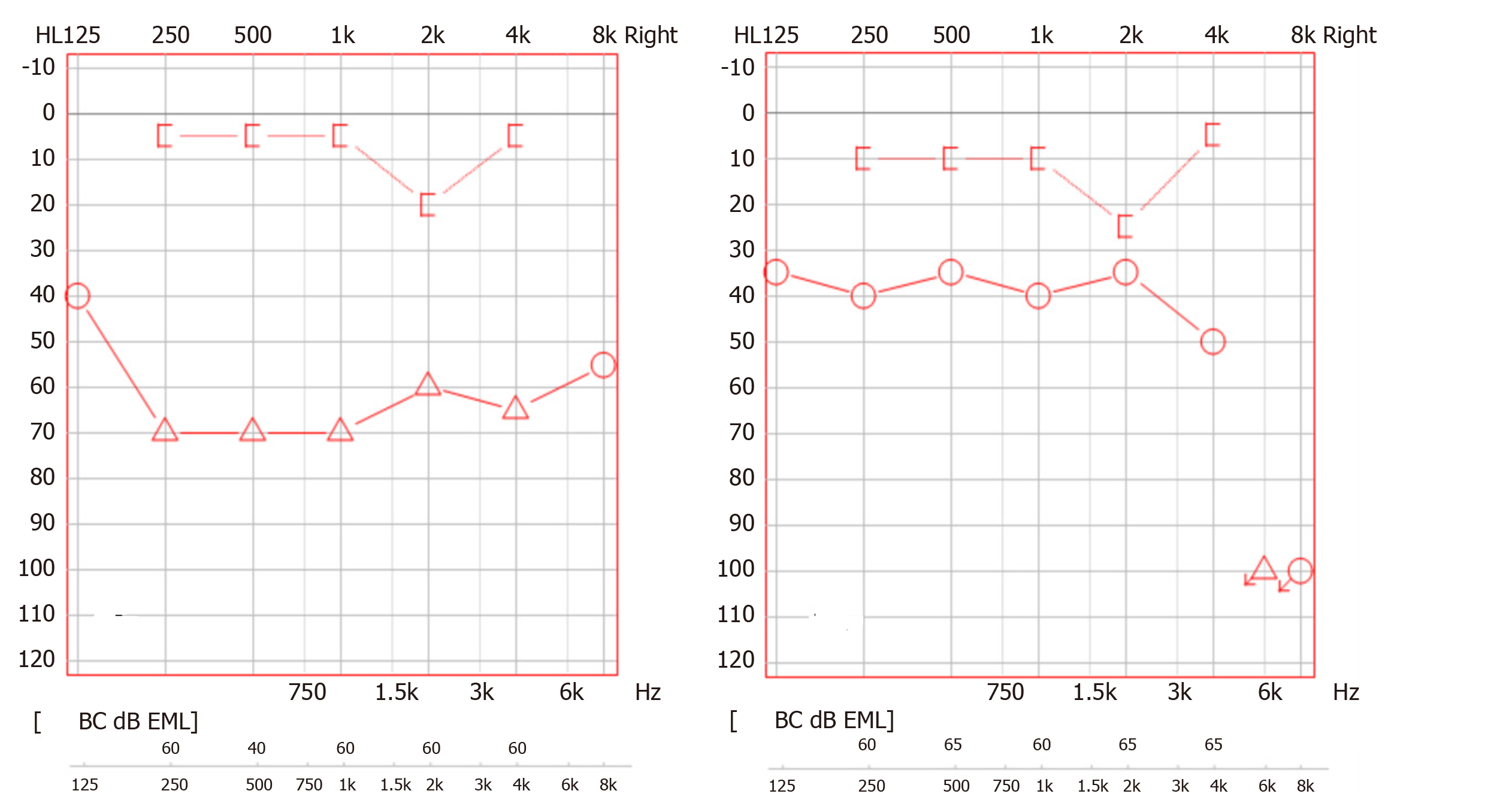
A computed tomography (CT) scan of the temporal bone showed a hypointense cystic mass protruding into the area of the atretic EAC (Figure 1). Color Doppler ultrasound showed a mucocele-like lesion with inhomogenous internal echoes. Pure-tone audiometry showed severe conductive hearing loss with an air-bone conduction gap of 56 decibels (dB).
The final diagnosis in this patient was FBCA accompanied by EAC atresia and middle ear malformation.
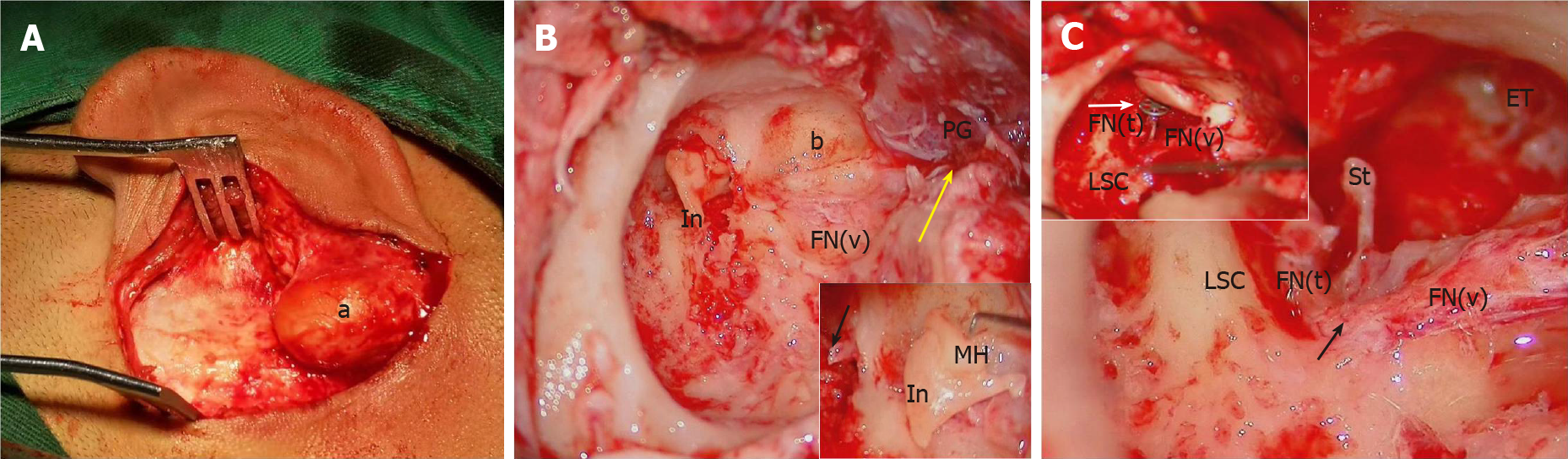
Under general anesthesia, mass excision, mastoidectomy, and simultaneous meatoplasty and tympanoplasty were performed under microscopy. A postauricular incision was performed, which showed that the mass originated from the stylomastoid foramen and adhered to the posterior surface of the parotid gland, invading the temporal bone. The lesion which tightly adhered to the stylomastoid foramen segment and the vertical segment of the FN was carefully removed with complete preservation of the parotid gland. Location malformation of the FN was observed, and the vertical segment was shifted to the anteposition and embedded in the lateral atresia bony plank of the tympanic cavity. We removed the bony structure to assess the tympanic cavity, and found that the ossicular chain was fused to the bony atresia plank, the malleus and incus were fused and fixed, and the stapes was normal with a mobile footplate. Tympanoplasty was performed with the tragus cartilage and a partial ossicular replacement prosthesis. A posterior occipital tissue flap and skin flap were used for meatoplasty (Figure 2).
The patient recovered well with an open EAC and improved hearing. The postoperative air-bone conduction gap was 21 dB, and the pure-tone average gain was 35 dB (Figure 3). No evidence of recurrence was found during follow-up at 6 mo postoperatively. No major complications, such as facial palsy and significant sensorineural hearing loss, occurred.
Generally, FBCAs are classified into Work I and Work II types according to the anatomical and histological features[7], Type I lesions are always present as soft cysts lined by squamous epithelium, and usually protrude into the EAC. Type II lesions usually present as a cyst, sinus, or fistula and are of ectodermal and mesodermal origin, containing either skin appendages or cartilage[6,8]. The histopathological examination of our case showed a soft cyst lined by squamous epithelium, the lesion was classified as Type 1, as previously reported[6], the soft mass also protruded into the bony atresia plank.
Most structures of the head and neck originate from the differentiation of branchial arches. The first arch develops into the EAC and tympanic membrane, and abnormal differentiation can induce FBCAs and aberrations of the EAC. Generally, EAC bony atresia means that the bony atresia plank has occupied the normal structure of the EAC. FBCA accompanied by external ear diseases are rare, and to date, only a few FBCA cases accompanied by congenital EAC stenosis or atresia, and cholesteatoma have been reported[4,9-11]. Banakis et al[4] reported a case of bilateral ear canal cholesteatomas in the setting of underlying FBCA. Hinson et al[10] reported the case of a 15-year-old female with a Type II first branchial cleft cyst presenting as a right neck mass and two main facial nerve trunks were found during surgery. However, to the best of our knowledge, this is the first report of a FBCA accompanied by EAC bony atresia, middle ear malformation and FN location malformation. The maldevelopment of the first and second branchial arches and the first gill ditch may cause malformation of the external and middle ear.
The diverse presentations and duplicated anomalies of FBCA pose a challenge for surgeons. As the lesions are usually very deep and often involved with the FN and parotid gland, especially in the condition of FBCA accompanied by aural stenosis or atresia, clinicians should be familiar with the otological and head and neck clinical features; surgical expertise must be available to remove the lesion completely, preserve FN function, and perform otologic reconstruction if necessary[12]. Traditionally, surgical removal of a FBCA involves either superficial or total parotidectomy for exposure[13], which might cause unnecessary trauma and the risk of FN injury[6,10]. Jang et al[11] reported a recurrent FBCA case, in which canal wall-up mastoidectomy and lesion removal under microscopy, with an effective postauricular approach, were performed.
In the present case, for EAC bony atresia, a postauricular approach was chosen for mastoidectomy. During the operation, the cyst was tightly adhered to the FN and parotid gland, lesion excision under microscopy reduced the risk of FN injury with preservation of the parotid gland. Interestingly, we found that the FN vertical segment was embedded outside the atretic bony plate of the tympanic cavity, we thus performed canaloplasty and ossiculoplasty at the same time. The patient had hearing improvement after surgery. To our knowledge, this is the first report of a FBCA accompanied by EAC bony atresia, middle ear malformation and FN location malformation, which were successfully treated with FBCA lesion removal, and simultaneous meatoplasty and tympanoplasty.
| 1. | LaRiviere CA, Waldhausen JH. Congenital cervical cysts, sinuses, and fistulae in pediatric surgery. Surg Clin North Am. 2012;92:583-597, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | Maithani T, Pandey A, Dey D, Bhardwaj A, Singh VP. First branchial cleft anomaly: clinical insight into its relevance in otolaryngology with pediatric considerations. Indian J Otolaryngol Head Neck Surg. 2014;66:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 3. | Abdollahi Fakhim S, Naderpoor M, Mousaviagdas M. First branchial cleft fistula associated with external auditory canal stenosis and middle ear cholesteatoma. Iran J Otorhinolaryngol. 2014;26:263-266. [PubMed] |
| 4. | Banakis Hartl RM, Said S, Mann SE. Bilateral Ear Canal Cholesteatoma with Underlying Type I First Branchial Cleft Anomalies. Ann Otol Rhinol Laryngol. 2019;128:360-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Yalçin S, Karlidağ T, Kaygusuz I, Demirbağ E. First branchial cleft sinus presenting with cholesteatoma and external auditory canal atresia. Int J Pediatr Otorhinolaryngol. 2003;67:811-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Magdy EA, Ashram YA. First branchial cleft anomalies: presentation, variability and safe surgical management. Eur Arch Otorhinolaryngol. 2013;270:1917-1925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Work WP. Newer concepts of first branchial cleft defects. Laryngoscope. 1972;82:1581-1593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 171] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | D'Souza AR, Uppal HS, De R, Zeitoun H. Updating concepts of first branchial cleft defects: a literature review. Int J Pediatr Otorhinolaryngol. 2002;62:103-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 99] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Ohki M, Baba Y, Ohata A. Temporal bone histopathology case of the month. First branchial cleft anomaly with an orifice in the bony external auditory canal accompanied by contralateral middle ear cholesteatoma. Otol Neurotol. 2015;36:e70-e72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Hinson D, Poteet P, Bower C. Duplicated facial nerve trunk with a first branchial cleft cyst. Laryngoscope. 2014;124:662-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Jang M, Dai C. An Effective Surgical Approach for the Management of Recurrent First Branchial Cleft Fistula with Cysts: A Case Report. J Int Adv Otol. 2017;13:419-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Chan KC, Chao WC, Wu CM. Surgical management of first branchial cleft anomaly presenting as infected retroauricular mass using a microscopic dissection technique. Am J Otolaryngol. 2012;33:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Guo YX, Guo CB. Relation between a first branchial cleft anomaly and the facial nerve. Br J Oral Maxillofac Surg. 2012;50:259-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mehrzad R S-Editor: Zhang L L-Editor: Webster JR P-Editor: Li JH