Published online Feb 16, 2026. doi: 10.12998/wjcc.v14.i5.117384
Revised: January 5, 2026
Accepted: February 2, 2026
Published online: February 16, 2026
Processing time: 66 Days and 20 Hours
Buried or submucosally embedded double-J (DJ) stents present a rare but tech
A 72-year-old woman presented to the emergency department with a 2-day hi
On examination, she was febrile and clinically unwell, with left costovertebral angle tenderness. Laboratory tests revealed elevated inflammatory markers and leukocytosis. CT imaging demonstrated right-sided hydronephrosis despite the presence of a DJ stent, with the left kidney adequately decompressed through the nephrostomy tube. Urine and blood cultures were obtained, and intravenous antibiotics and hydration were initiated. Despite 48 hours of conservative treatment, the patient showed no clinical improvement. Given the persistent hydronephrosis and the need for source control, the decision was made to perform bilateral stent exchange.
Core Tip: Buried ureteral stents pose a significant challenge when dense fibrosis obscures the distal end, preventing retrograde retrieval. This case presents a novel combined antegrade-retrograde technique integrating fluoroscopy-guided wire placement with transurethral resection to safely expose and remove a completely embedded double-J (DJ) ureteral stent. By using the antegrade guidewire to precisely localize the intramural ureter, this approach minimizes tissue trauma and offers an effective solution for managing complex DJ stent embedding in patients with malignancy-related fibrosis.
- Citation: Deligiannis P, Katsimperis S, Kyriazis I, Angelopoulos P, Neofytou P, Kapsalos-Dedes SG, Triantafyllou P, Arseniou P, Katelani S, Papatsoris A. Fluoroscopy-guided transurethral resection with antegrade guidewire assistance for retrieval of a buried double-J stent: A case report. World J Clin Cases 2026; 14(5): 117384
- URL: https://www.wjgnet.com/2307-8960/full/v14/i5/117384.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v14.i5.117384
Double-J (DJ) ureteral stents play a critical role in managing obstructive uropathy, particularly in patients with locally advanced or metastatic malignancies[1]. Although routine stent exchanges are usually straightforward, various complications, such as encrustation, migration, or fibrosis, may impede access to the stent’s distal curl[2,3]. Such complications can range in severity from minor technical difficulties to clinically significant events, including recurrent urinary tract infections, pyelonephritis, and obstructive uropathy, which may progress to urosepsis or renal dysfunction if not promptly addressed[4,5]. Submucosal embedding of the distal stent segment is uncommon, but when present, it significantly increases procedural complexity and may require alternative strategies beyond conventional retrograde extraction.
Patients with bladder cancer, repeated endoscopic procedures, chronic inflammation, and prior radiotherapy or chemotherapy are at heightened risk of tissue overgrowth and fibrosis around the ureteral orifice. In such settings, a combined antegrade-retrograde approach can facilitate accurate localization and safe retrieval of a buried stent.
This report outlines a case in which fluoroscopy-guided antegrade wire placement, paired with transurethral resection of obstructing tissue, enabled complete and safe removal of a deeply embedded DJ stent.
A 72-year-old woman presented to the emergency department with a 2-day history of fever, nausea, and worsening malaise. She described progressive left flank discomfort and suprapubic pressure.
Symptoms started 2 days before presentation with fever and nausea.
Her medical history includes muscle-invasive bladder carcinoma with metastatic spread to the vertebral column, pelvic bones, and sacrum. She was receiving immunotherapy and had undergone multiple prior chemotherapy cycles. Bilateral ureteral DJ stents had been placed several months earlier due to malignant ureteral obstruction, and a left nephrostomy tube had subsequently been inserted following a prior obstructive episode.
The patient denied any family history of malignant tumours.
On examination, she was febrile and clinically unwell, with left costovertebral angle tenderness.
Laboratory tests revealed elevated inflammatory markers and leukocytosis.
Computed tomography (CT) imaging demonstrated right-sided hydronephrosis despite the presence of a DJ stent, with the left kidney adequately decompressed through the nephrostomy tube.
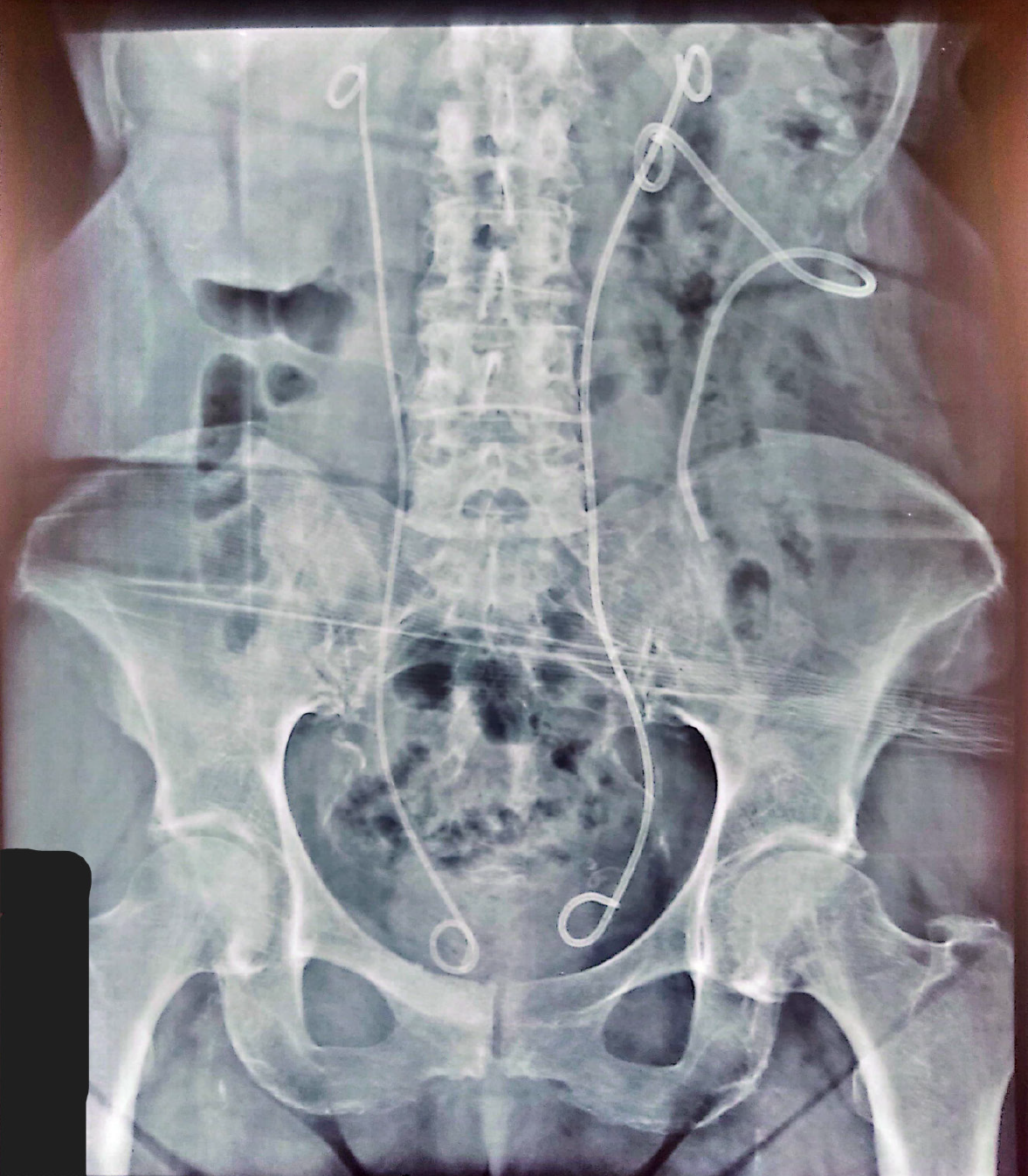
Buried distal left double-J ureteral stent with obliteration of the left ureteral orifice due to severe trigonal fibrosis secondary to chronic inflammation and tumor-related changes, successfully managed using a combined antegrade-retrograde endoscopic approach (Figure 1).
Under general anesthesia, the right ureteral stent was readily identified and exchanged without difficulty. However, cystoscopic examination of the left ureteral region revealed no visible ureteral orifice. The mucosa in the trigonal area appeared thickened and fibrotic, likely secondary to chronic inflammation, prior instrumentation, and tumor-related changes. The distal pigtail of the left DJ stent could not be located despite repeated attempts as it was buried (Figure 2). Due to the inability to access the stent, an antegrade approach was initiated. A hydrophilic guidewire was advanced through the existing left nephrostomy tube. Under continuous fluoroscopy, the wire was carefully manipulated down the ureter until it approached the intramural ureter. Simultaneously, using a transurethral resectoscope, gradual resection of the fibrotic tissue overlying the expected location of the ureteral orifice was performed. As the wire tip approached the bladder, fluoroscopy confirmed its position. Eventually, the advancing guidewire became visible endoscopically, enabling us to find the exact location of the buried stent. The embedded stent was then grasped and removed without resistance. A new one was placed over the antegrade wire, ensuring optimal drainage of the upper urinary tract.
The procedure was completed successfully without intraoperative complications. Postoperatively, the patient de
At follow-up, the patient remained clinically stable with preserved renal function and no recurrence of obstructive symptoms. Imaging confirmed appropriate stent position and adequate drainage of the left collecting system. A planned stent exchange strategy and close surveillance were instituted given the underlying fibrotic and tumor-related pathology.
The patient’s fever subsided within 24 hours, and her energy levels improved markedly. She was discharged with instructions for outpatient follow-up and stent management.
Buried or embedded ureteral stents, although uncommon, pose a significant challenge during endourological procedures[6]. They typically result from chronic inflammation, malignant obstruction, prolonged indwelling time, or prior oncologic treatments that alter the normal tissue architecture. In patients with bladder cancer, recurrent infections and repeated instrumentation can further promote mucosal thickening and fibrosis around the ureteral orifice, making retrograde stent retrieval difficult or impossible.
Preventive strategies include strict adherence to stent exchange intervals, careful documentation and follow-up of indwelling. Minimizing stent dwell time through strict adherence to scheduled exchange intervals, particularly in oncologic patients who may require long-term urinary drainage, implementation of stent-tracking systems, clear documentation of stent insertion and planned exchange dates.
In patients anticipated to require extended urinary diversion, alternative strategies such as percutaneous nephrostomy or early conversion to tandem ureteral stents may reduce chronic irritation at the ureterovesical junction. When long-term stenting is necessary, appropriate stent length selection and careful positioning of the distal curl within the bladder may help limit mucosal trauma and subsequent epithelial overgrowth. Additionally, minimizing repeated ureteral manipulation and ensuring prompt treatment of urinary tract infection or inflammation may further reduce the risk of sub
Early or preoperative diagnosis may be suggested by difficulty in visualizing the distal stent curl during cystoscopy, resistance encountered during attempted stent removal, or radiographic findings showing abnormal stent positioning or fixation. Preoperative imaging, particularly fluoroscopy or computed tomography scan, can help assess stent location and identify potential embedding. Awareness of this entity and a high index of suspicion in high-risk patients may facilitate early recognition and allow appropriate planning for combined or alternative retrieval techniques, thereby reducing procedural complications.
To the best of our knowledge, this is the first published case in which a buried DJ stent required a combined antegrade-retrograde approach specifically due to complete loss of access to the distal ureteral orifice. Previous reports have primarily described submucosal impaction of the proximal (upper) part of the stent, where the distal curl remained visible or accessible cystoscopically[7]. In contrast, our case was uniquely challenging because the lower ureter and distal pigtail were entirely obscured by dense fibrotic tissue, rendering conventional retrograde retrieval impossible. This anatomic limitation necessitated the use of an antegrade guidewire for localization and a targeted transurethral resection to expose the intramural ureter, highlighting an innovative strategy for managing extreme forms of stent embedding.
In such complex scenarios, combining antegrade access with retrograde endoscopic techniques offers distinct advantages. The antegrade guidewire provides a reliable means of identifying the intramural ureter and confirming the orientation of the embedded stent under fluoroscopic visualization. This reduces the need for blind exploration and allows the surgeon to work with a clear anatomical target.
Simultaneously, controlled transurethral resection of the overlying fibrotic tissue enables gradual and precise exposure of the buried stent. Because the resection is guided by both the visual confirmation of the wire and continuous imaging, tissue removal can be performed conservatively, with minimal disruption to the surrounding bladder structures. This combination enhances procedural safety, shortens operative time, and decreases the risk of ureteral trauma or per
The hybrid approach used in this case demonstrates how integrating antegrade and retrograde techniques can transform an otherwise complex retrieval into a safe and reproducible procedure. It highlights the importance of flexibility and creativity in endourological management, particularly in patients with altered anatomy due to malignancy or prior interventions.
| 1. | Pavlovic K, Lange D, Chew BH. Stents for malignant ureteral obstruction. Asian J Urol. 2016;3:142-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Tomer N, Garden E, Small A, Palese M. Ureteral Stent Encrustation: Epidemiology, Pathophysiology, Management and Current Technology. J Urol. 2021;205:68-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 3. | Breau RH, Norman RW. Optimal prevention and management of proximal ureteral stent migration and remigration. J Urol. 2001;166:890-893. [PubMed] |
| 4. | el-Faqih SR, Shamsuddin AB, Chakrabarti A, Atassi R, Kardar AH, Osman MK, Husain I. Polyurethane internal ureteral stents in treatment of stone patients: morbidity related to indwelling times. J Urol. 1991;146:1487-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 222] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 5. | Singh I, Gupta NP, Hemal AK, Aron M, Seth A, Dogra PN. Severely encrusted polyurethane ureteral stents: management and analysis of potential risk factors. Urology. 2001;58:526-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 128] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Damiano R, Oliva A, Esposito C, De Sio M, Autorino R, D'Armiento M. Early and late complications of double pigtail ureteral stent. Urol Int. 2002;69:136-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 137] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Ziauddin SAM, Devana SK, Sharma A, Chaudhary K. Submucosal impaction of a forgotten DJ stent: addressing the unexpected. BMJ Case Rep. 2021;14:e243580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/