Published online Feb 16, 2026. doi: 10.12998/wjcc.v14.i5.117610
Revised: January 6, 2026
Accepted: January 29, 2026
Published online: February 16, 2026
Processing time: 60 Days and 14.1 Hours
Delays in resolving diagnostic disagreements within the quantitative imaging analysis core can impede clinical workflow and compromise patient care. To ad
To evaluate the impact of a dedicated consult shift on diagnostic disagreement resolution times and operational efficiency.
This retrospective quality improvement study analyzed timestamp data from 1245 cases of diagnostic disagreement spanning the period from 2017 to 2025. Cases were stratified into two groups: Pre-implementation (2017-2022) and post-implementation (2023-2025). The primary metric was time to resolution in days. Both means and medians were compared using an independent samples t-test and a Mann-Whitney U test, respectively.
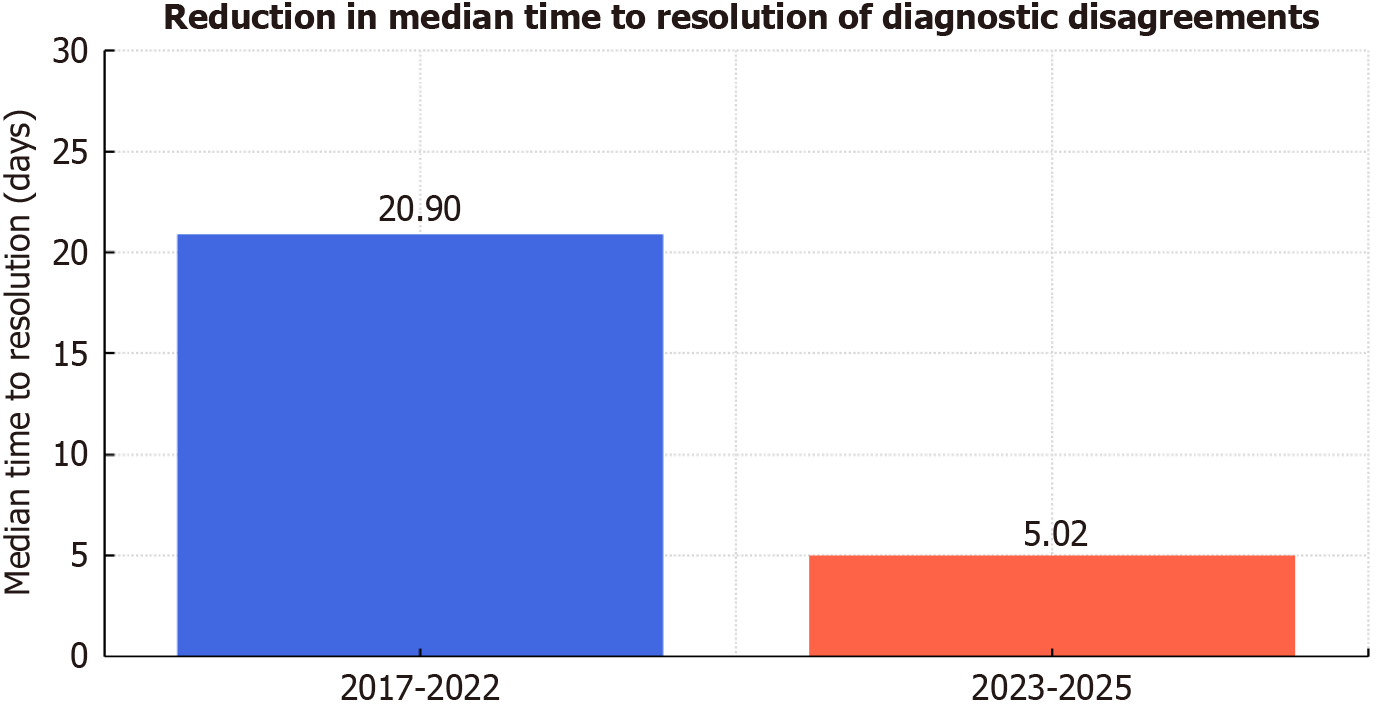
The average time to resolution significantly decreased from 100.58 days (2017-2022) to 33.05 days (2023-2025) (t = 10.02, P < 0.0001). Additionally, the median time to resolution dropped from 20.90 days to 5.02 days, a statistically significant reduction confirmed by the Mann-Whitney U test (U = 241577, P < 0.0001).
The introduction of a dedicated consult shift, supported by real-time dashboard tracking, led to a significant im
Core Tip: This study evaluates the implementation of a dedicated consult shift supported by real-time dashboard tracking, which improved resolution times for diagnostic disagreements. After implementation, average and median resolution times improved by more than 67% and 76%, respectively. These post-intervention improvements demonstrate the value of structured quality assurance interventions in enhancing operational efficiency and reducing delays in patient care and clinical trial reporting.
- Citation: Virarkar M, Altintas Taslicay C, Supsupin E, Bhosale H, Shah R, Hassan A, Guevara Tirado OA, Ortiz Cordero RG, Morani AC. Impact of a dedicated consult shift on reducing time to resolution of diagnostic disagreements: A quality improvement initiative. World J Clin Cases 2026; 14(5): 117610
- URL: https://www.wjgnet.com/2307-8960/full/v14/i5/117610.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v14.i5.117610
Diagnostic disagreements in radiology reporting pose a significant challenge for clinical trial operations, oncology care, and quality assurance across complex healthcare systems[1,2]. As cancer care has become increasingly evidence-driven and imaging-centric, the workflow for finalizing trial imaging reports must strike a balance between speed, accuracy, and collaborative oversight[3]. The quantitative imaging analysis core (QIAC) at major academic medical centers plays a central role in adjudicating imaging findings for oncology trials; its ability to rapidly resolve diagnostic disagreements is vital to maintaining the integrity and continuity of clinical research as well as informing real-time treatment decisions[4].
Historically, disagreement resolution in radiology departments has required a multi-step administrative process, including asynchronous communication between physicians and quality assurance teams, as well as periodic review cycles[5-7]. Such workflows are inherently subject to delays, especially when complex cases cross multiple subspecialties or involve ambiguous findings. Prolonged time to resolution can hinder trial progression, introduce bias in outcome adjudication, and delay patient management. Recent calls for operational innovation in radiology have highlighted the need for structured process improvements, real-time data tracking, and agile escalation protocols to address these bot
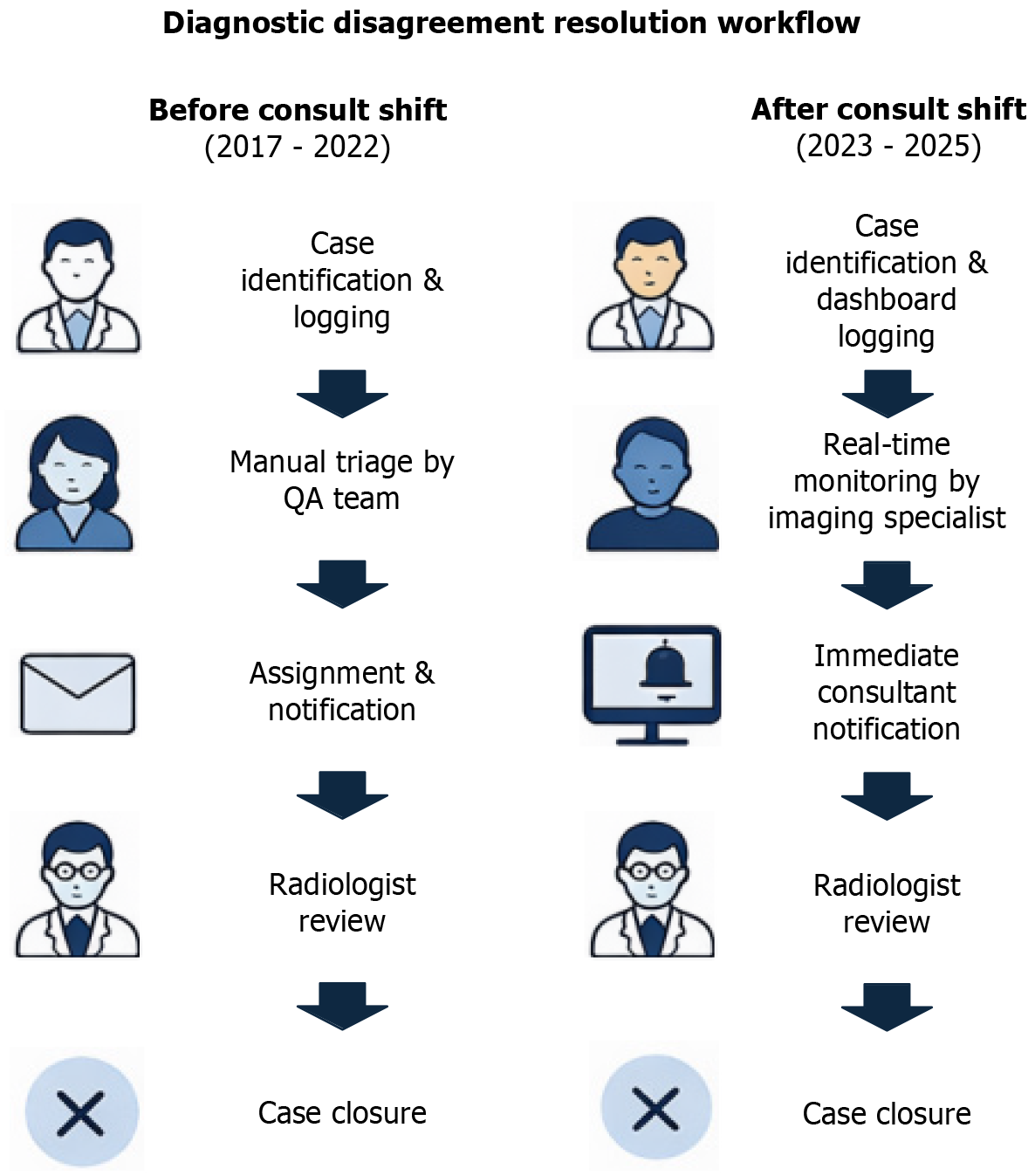
To address these limitations, the QIAC implemented a dedicated consult shift intervention in 2023. This formal workflow utilized real-time dashboard tracking of open disagreements, immediate case notification, and rapid in
This quality improvement study leverages the record of diagnostic disagreements reviewed by QIAC from 2017 to 2025, with robust timestamp analytics enabling calculation of resolution intervals for all finalized cases. This study evaluates the impact of a dedicated consult shift intervention on time to resolution of diagnostic disagreements in a high-volume academic radiology setting. These findings may inform broader workflow optimization, process standardization, and quality monitoring in radiology-driven clinical research.
This retrospective quality improvement study was conducted at a comprehensive cancer center, analyzing diagnostic disagreement cases reviewed by the QIAC between January 2017 and May 2025. The QIAC provides centralized imaging review and quality assurance for all cancer clinical trials at the institution. Due to the retrospective nature of this study, unaccounted confounding factors (e.g., staffing changes, case mix, dashboard modifications, or concurrent initiatives) may have influenced outcomes independent of the consult shift.
All formal diagnostic disagreements logged in the QIAC database during the study period were extracted. Each case entry included timestamps for disagreement initiation and resolution, the type of disagreement [physician/investigator (PI) or quality assurance (QA)], and the departmental source. Only cases with complete resolution data (both dis
A dedicated consult shift for resolving real-time imaging disagreements was implemented in January 2023. This intervention included a centralized dashboard that tracked all open disagreements. An on-call radiologist (“Consultant”) and imaging specialist facilitated immediate notification, review, and adjudication of newly raised disagreements as part of their routine activities. Comparisons were made between pre- (2017-2022) and post-intervention (2023-2025) periods.
The primary outcome was time to resolution, defined as the interval (in calendar days) between the disagreement date/time and resolution date/time. Secondary measures included the distribution of disagreement types and departmental patterns.
Disagreement cases were stratified into two periods: Pre- and post-intervention. Time-to-resolution was summarized using means, medians, standard deviations, and interquartile ranges. Differences between groups were evaluated by an independent samples t-test (mean) and a Mann-Whitney U test (median) due to non-normal data distribution. Effect size was calculated using Cohen’s d. Statistical significance was set at P < 0.05. Data analyses were performed using SPSS version 22.
This quality improvement initiative was conducted in accordance with institutional quality assurance and performance improvement guidelines, and a formal institutional review board review/waiver was obtained as indicated. All data were de-identified and managed in accordance with institutional standards for clinical audit and quality research.
The implementation of the dedicated consult shift intervention resulted in substantial improvements in the efficiency of resolving diagnostic disagreements within the QIAC workflow (Figure 1). Analysis of 1245 resolved cases from 2017 to 2025 revealed that the average time to resolve disagreements decreased dramatically after the intervention, from 100.6 days in the pre-implementation period (2017-2022) to just 33.0 days in the post-implementation era (2023-2025) (Figure 2). Notably, the median time to resolution decreased by 76%, from 20.9 days to 5.0 days, signifying a significant shift toward expedited case review and closure (Table 1).
| Metric | 2017-2022 | 2023-2025 |
| Number of cases | 601 | 643 |
| Mean (days) | 100.58 | 33.05 |
| Standard deviation (days) | 151.80 | 67.51 |
| Median (days) | 20.90 | 5.02 |
| Min-max (days) | 0.00-576.91 | 0.00-322.59 |
Both parametric and non-parametric statistical tests confirmed these findings were highly significant (t-test and Mann-Whitney U, P < 0.0001), and the effect size was moderate, demonstrating genuine operational impact (Table 2). The results suggest that real-time monitoring, structured escalation, and a formal consult workflow were associated with reduced diagnostic delays in complex radiology quality assurance environments. These workflow enhancements may accelerate clinical trial reporting and support rapid and reproducible quality improvement in high-volume academic imaging settings.
| Metric | 2017-2022 | 2023-2025 |
| Median (days) | 20.90 | 5.02 |
| Statistical test used | Mann-Whitney U | |
| U-statistic | 241577.0 | |
| P value | 2.21 × 10-14 |
This quality improvement initiative demonstrates that structured workflow interventions can significantly accelerate the resolution of diagnostic disagreements in high-volume cancer imaging core facilities. The implementation of a dedicated consult shift model, supported by real-time dashboard monitoring and immediate case escalation protocols, achieved a substantial 67%-76% reduction in time to resolution from a median of 20.9 days in the pre-implementation period (2017-2022) to 5.0 days in the post-implementation era (2023-2025), representing a clinically meaningful and operationally significant improvement.
The success of the QIAC consult shift intervention mirrors findings from other institutions that have implemented similar structured approaches to imaging workflow management and quality assurance. A 2025 study from Oman demonstrated that standardized operating procedures, formal triage systems, and regular interdepartmental case discussions improved overall turnaround time performance from 88% to 95% over a 10-month period, highlighting the critical importance of systematic processes and communication in achieving consistent quality metrics[9].
Similarly, previous groundbreaking work at MD Anderson Cancer Center demonstrated that implementing a web-based QIAC workflow platform reduced the turnaround time for quantitative tumor metric reports from 31.7 hours to 15.9 hours (P = 0.0005), representing a 50% improvement[10]. More recently, innovations such as dual digital alert systems and automatic radiologist rescheduling protocols have further streamlined QIAC report delivery, supporting timely therapeutic decision-making in oncology trials. These findings collectively support the notion that digital infrastructure, coupled with process redesign, drives sustainable operational improvements in radiology quality as
The reduction in variability observed in this study is particularly noteworthy and clinically important. The 55.5% decrease in standard deviation (from 151.80 days to 67.47 days) and the 85.3% decrease in interquartile range (from 141.49 days to 20.74 days) indicate that resolution times have become not only faster but also significantly more pre
In addition, adjunct operational models may help reduce delays, and the development of radiology e-consult services has been shown to reduce unnecessary imaging, decrease specialty referrals, and improve access to radiology expertise while simultaneously reducing workflow interruptions for radiologists[11]. These complementary approaches underscore the potential for multifaceted interventions to optimize radiology operations across multiple dimensions.
Data quality: The analysis relied on previously recorded operational data from a single center, which may be incomplete or inconsistently documented, potentially leading to issues with data quality and accuracy.
Selection bias: Only cases with complete timing information for both disagreement and resolution were included. This might exclude unresolved or delayed cases and could underestimate the true time to resolution or underrepresent more complex scenarios.
Confounding factors: Due to the study’s multi-year design, unmeasured changes in staffing, technology (e.g., dashboard enhancements), clinical trial complexity, or case mix over time could influence results independent of the consult shift intervention. Differences between pre- and post-implementation periods may be subject to temporal trends or other concurrent quality improvement measures, making attribution solely to the consult shift less certain.
Generalizability: Findings may be specific to the workflows, staffing, and consult shift procedures at our institution and may not be directly applicable to other centers with different structures or processes.
Outcomes and scope: The primary endpoint was operational (time to resolution), and the study did not systematically assess the clinical impact (patient outcomes, downstream care delays, etc.) of disagreement resolution timing. Additionally, the study did not incorporate systematic perceptions or satisfaction surveys from radiologists, referring clinicians, or patients relating to workflow changes and their impact.
The principles demonstrated in this work—real-time monitoring, structured escalation, interdisciplinary collaboration, and data-driven process improvement—extend well beyond QIAC operations and can be adapted for use in other high-volume radiology workflows, including emergency radiology departments, teleradiology networks, and community and private practice settings. Future research should investigate whether accelerated disagreement resolution directly translates into improved clinical trial outcomes, reduced protocol deviations, enhanced patient satisfaction, and more cost-effective metrics.
The implementation of a dedicated consult shift, supported by real-time dashboard monitoring and rapid escalation protocols, resulted in a significant and sustainable reduction in the time to resolution of diagnostic disagreements within the QIAC radiology workflow. Average and median resolution times improved by more than 67% and 76%, respectively, following the intervention, with robust statistical significance and a clinically meaningful effect size. These process improvements demonstrate the value of structured quality assurance interventions in enhancing operational efficiency and reducing delays in clinical trial reporting. The interpretation of these results is limited by the single-center, re
| 1. | Ritchie B, Summerville L, Sheng M, Choi M, Tirumani S, Ramaiya N. Impact of turnaround time in radiology: The good, the bad, and the ugly. Curr Probl Diagn Radiol. 2025;S0363-0188(25)00089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Soffa DJ, Lewis RS, Sunshine JH, Bhargavan M. Disagreement in interpretation: a method for the development of benchmarks for quality assurance in imaging. J Am Coll Radiol. 2004;1:212-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 71] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Flug JA, Stellmaker JA, Tollefson CD, Comstock EM, Buelna E, Truman B, Ponce L, Milosek A, McCabe J, Jokerst CE. Improving Turnaround Time in a Hospital-based CT Division with the Kaizen Method. Radiographics. 2022;42:E125-E131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Rao SH, Virarkar M, Yang WT, Carter BW, Liu TA, Piwnica-Worms D, Bhosale PR. Streamlining the Quantitative Metrics Workflow at a Comprehensive Cancer Center. Acad Radiol. 2021;28:1401-1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Zhang L, Wen X, Li JW, Jiang X, Yang XF, Li M. Diagnostic error and bias in the department of radiology: a pictorial essay. Insights Imaging. 2023;14:163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 25] [Reference Citation Analysis (0)] |
| 6. | FitzGerald R. Radiological error: analysis, standard setting, targeted instruction and teamworking. Eur Radiol. 2005;15:1760-1767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Kushner DC, Lucey LL; American College of Radiology. Diagnostic radiology reporting and communication: the ACR guideline. J Am Coll Radiol. 2005;2:15-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 82] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | More R, Dunn E, Dunwell S. Improving radiology: a whole-system opportunity. Clin Radiol. 2023;78:395-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Al Qassabi B, AlSukaiti R, Alajmi S, Omar AS, Ibrahim R, Banibakr AA, Al-Baimani K, Zribi A, AlDhahli SN, Majed M, AlGhaithi MM, AlBalushi SQ, AlHasni NS, Al Sheedi S, Al-Awaisi HS, Al-Riyami N, Ayaad O. Improving Turnaround Times and Operational Efficiency in Radiology Services: Quality Improvement Study in Oman. Asian Pac J Cancer Prev. 2025;26:1709-1718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Bhalde R, Taslicay CA, Virarkar M, Sun J, Burke SM, Nayak A, Rao S, Mayuresh S, Morani A, Bhosale P. Enhancing Clinical Trial Efficiency: The Impact of a Dual Digital Alert System on Quantitative Imaging Report Turnaround Time. J Comput Assist Tomogr. 2025;49:471-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Suresh K, Hill PA, Kahn CE Jr, Schnall MD, Rosen MA, Zafar HM, Trerotola SO, Cook TS. Quality Improvement Report: Design and Implementation of a Radiology E-Consult Service. Radiographics. 2023;43:e230139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/