Published online Dec 26, 2025. doi: 10.12998/wjcc.v13.i36.114956
Revised: October 30, 2025
Accepted: December 11, 2025
Published online: December 26, 2025
Processing time: 84 Days and 2.5 Hours
Patients who have undergone pancreaticoduodenectomy (Whipple procedure) often develop complex late complications that may be diagnostically challenging. We report a rare cause of recurrent fever and abdominal pain in such a patient: Fish bone-induced jejunal perforation. This case emphasizes the importance of maintaining suspicion for atypical, non-biliary causes in post-Whipple patients with recurrent symptoms, particularly when conventional tests suggest no biliary obstruction. A thorough linear diagnostic approach and multidisciplinary collaboration are essential. The delay in diagnosis highlights the challenges of inter
A 55-year-old female with a Whipple procedure history 10 years earlier presented with recurrent fever and severe abdominal pain. An initial extensive workup, including imaging and laboratory tests, was inconclusive. Only after detailed re-evaluation of the computed tomography images revealed a subtle linear hyper
Clinicians should consider gastrointestinal foreign body perforation in the differential diagnosis of recurrent fever and abdominal pain in patients with altered anatomy after Whipple procedure. Critical image review and advanced enteroscopic techniques are invaluable for diagnosing obscure causes in complex cases.
Core Tip: This case highlights the importance of considering atypical causes like gastrointestinal foreign body perforation in patients with altered postoperative anatomy presenting with recurrent fever and abdominal pain. Despite extensive workup, the cause remained elusive until deep push enteroscopy identified an embedded fish bone in the efferent jejunal limb of a post-Whipple patient. This was only possible after a thorough review of the computed tomography imaging, which showed a subtle linear hyperdensity. This case demonstrates the value of critical image review and advanced endoscopic techniques in diagnosing obscure gastrointestinal pathology in complex post-surgical patients.
- Citation: Taha R, Elsayed G, Mohamed L, Gadour E. Beyond biliary causes, fish bone perforation as a rare etiology of recurrent fever in a post-Whipple patient: A case report. World J Clin Cases 2025; 13(36): 114956
- URL: https://www.wjgnet.com/2307-8960/full/v13/i36/114956.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i36.114956
Pancreaticoduodenectomy, commonly referred to as the Whipple procedure, is frequently performed to address neo
Fever and severe abdominal pain.
Recurrent fever up to 39 °C, severe abdominal pain, and progressive weight loss over the past year. These symptoms have developed gradually and are causing significant concern, potentially indicating a complication related to her previous pancreatic surgery or a recurrence of her original condition.
Whipple surgery in 2015.
No family history of a similar condition. No other clinical history.
Apart from abdominal pain, surgical scars of the previous surgeries and recorded high temperatures, nothing else was remarkable.
The results of the laboratory examinations indicate cholangitis, Table 1.
| Test parameter | Reference range | January 25, 2025 | March 24, 2025 | April 28, 2025 |
| AST (SGOT) | 0-35 U/L | 51 | 21 | 29.60 |
| ALT (SGPT) | 0-45 U/L | 45 | 38 | 32.90 |
| ALP | 30-120 U/L | 83 | 21 | 99 |
| Total bilirubin | > 21 (μmol/L) | 5 | 8 | 4.55 |
| Direct bilirubin | > 7 (μmol/L) | 2 | 3 | 1.68 |
| Albumin | 40-60 g/L | 47 | 46 | 43.20 |
| Total protein | 64-83 g/L | 76 | 80 | 85.700 |
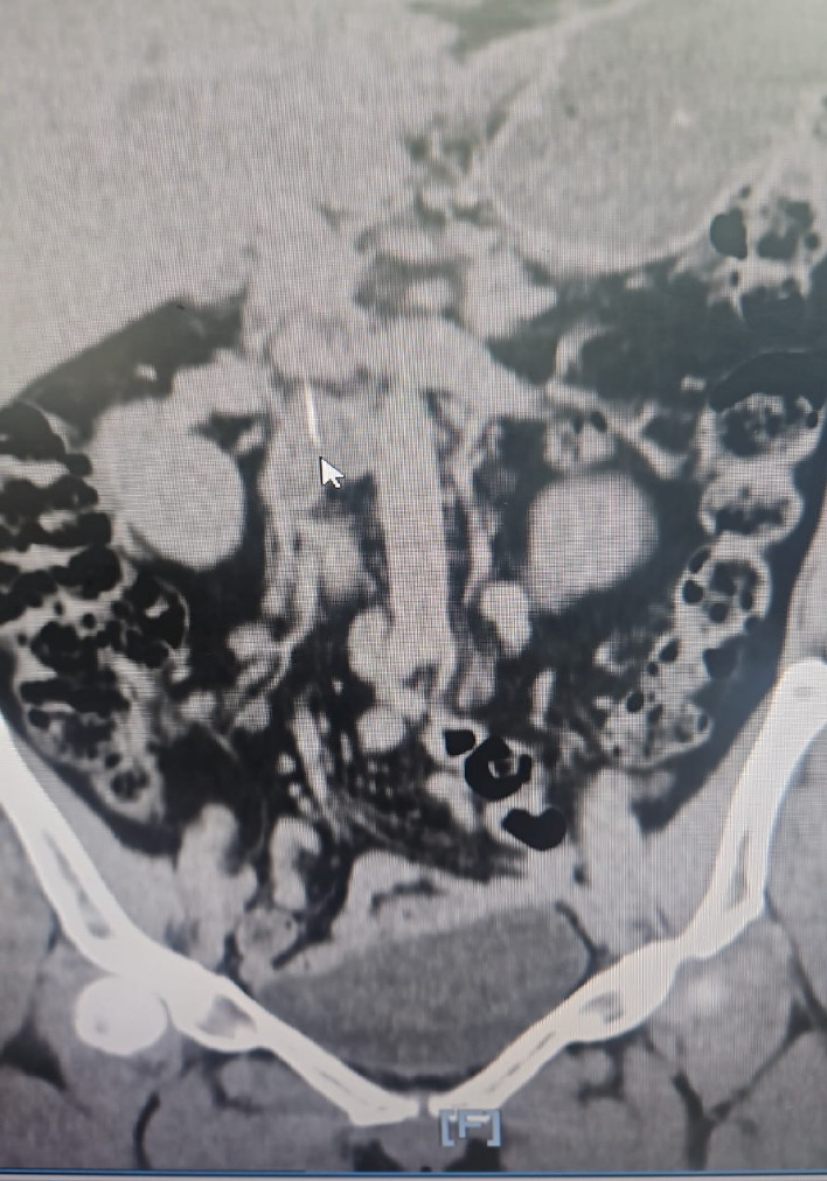
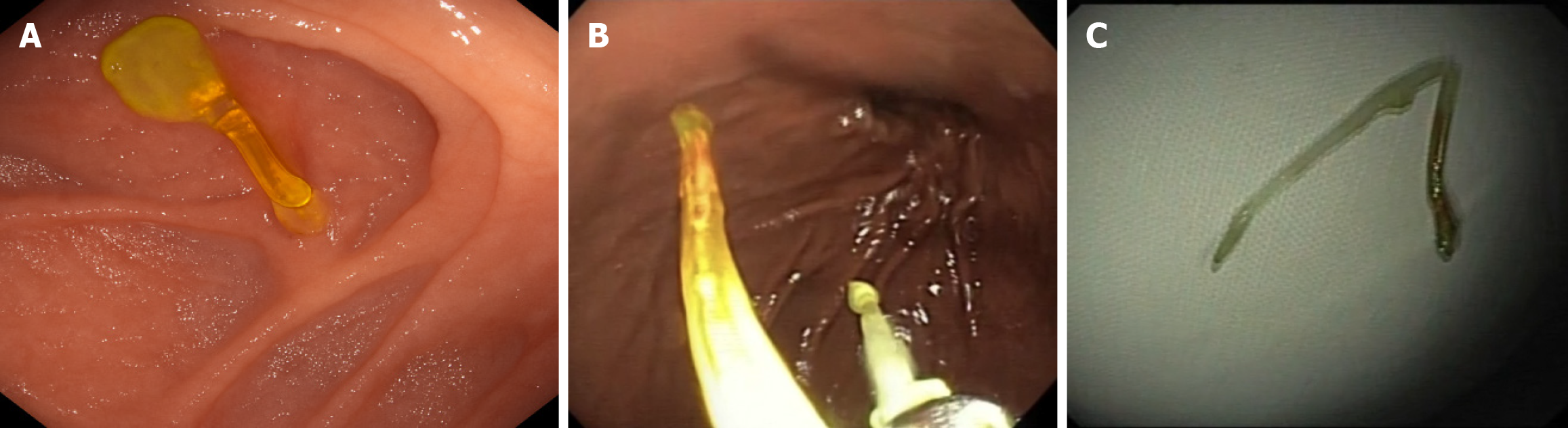
Magnetic resonance cholangiopancreatography (MRCP) showed no hepatico-jejunostomy stricture or biliary dilatation but revealed a 37-mm linear filling defect in the right intrahepatic duct, initially suspected as intrahepatic lithiasis. Percutaneous transhepatic cholangiography was planned but abandoned after ultrasound revealed no ductal dilation. An incidental right hydronephrosis prompted CT kidneys, ureters, and bladder (KUB), which, upon careful second review, demonstrated a subtle, linear hyperdense structure traversing the efferent jejunal limb toward the right renal vein, consistent with a fish bone (Figure 1). This clarified the previously ambiguous intrahepatic filling defect, which likely represented inflammatory changes secondary to jejunal perforation. Deep push enteroscopy using an Olympus PCFPH190 L pediatric colonoscope revealed a fish bone deeply embedded in the jejunal wall of the efferent limb (Figure 2A). The specimen was meticulously extracted intact using biopsy forceps (Figure 2B and C) (Video).
Recurrent cholangitis due to a fishbone perforation.
Endoscopic extraction of the fishbone and intravenous antibiotics.
Intravenous piperacillin-tazobactam was administered. The patient markedly improved with resolution of fever and abdominal pain. Subsequent outpatient follow-up demonstrated stable recovery with no further complications.
The present case illustrates the complexities involved in diagnosing recurrent abdominal pain and infection in indi
The delay in diagnosis can be attributed to several factors. First, the non-specific symptoms mimicked those of a biliary tract infection (cholangitis), which is a common post-Whipple complication. This similarity in presentation led to an initial misdiagnosis and delayed identification of the true cause. Second, normal liver function test results contradicted the clinical suspicion of biliary obstruction, leading to diagnostic uncertainty. This discrepancy between the clinical presentation and laboratory findings further complicates the diagnostic process.
The initial imaging interpretation focused on biliary pathology, overlooking subtle signs of gastrointestinal foreign bodies. The linear filling defect on MRCP was misinterpreted as intrahepatic lithiasis instead of localized inflammation and fistulization caused by a penetrating fish bone. This misinterpretation highlights the importance of considering non-biliary causes in patients with persistent symptoms, despite normal liver test results.
The pathophysiology linking jejunal perforation to the clinical picture provides insight into the patient presentation. The embedded fish bone caused localized perforation in the efferent jejunal limb with adjacent inflammation. This likely resulted in bacterial translocation, causing recurrent episodes of low-grade bacteremia and fever, clinically mimicking cholangitis. These inflammatory changes led to a pseudo-filling defect in the right intrahepatic duct due to extrinsic compression or inflammatory infiltration, accounting for the ambiguous imaging signs.
Lin et al[5] emphasized that "such complications may manifest months to years post-operatively and are often challenging to identify in the early stages due to their non-specific or intermittent nature". Recently, Kihara et al[6] highlighted that late postoperative cholangitis can develop even in the absence of strictures and may present with vague recurrent febrile episodes, further complicating the diagnosis.
The eventual discovery and extraction of a fish bone during enteroscopy, following an intensive review of recent imaging, was exceptionally useful in this case. This foreign object was located deeply embedded within the small bowel wall of the efferent limb, presumably inducing localized inflammation and contributing to recurrent episodes of bacteremia. Goh et al. reviewed a cohort of patients who experienced gastrointestinal perforations secondary to ingested foreign objects, "noting that fish bones were among the most frequently reported culprits"[7].
This case shows several important clinical implications. Maintaining a high index of suspicion for non-biliary causes is crucial when postoperative patients exhibit normal liver test results but persistent symptoms. A critical re-evaluation of imaging by experienced radiologists is necessary, especially in patients with anatomical alterations. Advanced endo
Successful endoscopic extraction resulted in clinical improvement, suggesting that the foreign body played a more pivotal role in her clinical presentation than initially presumed. This case highlights the efficacy of deep enteroscopy techniques and critical image reviews in cases of altered anatomy, leading to the identification of a non-biliary source of infection in complex postoperative scenarios. Balloon-assisted and double-balloon enteroscopy approaches have been shown to significantly enhance the diagnostic and therapeutic capabilities in patients with surgically altered gastrointestinal anatomy[8].
Our case emphasizes that, beyond common biliary complications, rare causes such as gastrointestinal foreign body perforations must be considered in post-Whipple patients with recurrent fever and abdominal pain. Meticulous imaging reviews and the utilization of advanced endoscopic techniques are indispensable. This case reinforces the importance of a broad differential diagnosis, early multidisciplinary evaluation, and vigilance for subtle imaging signs to avoid delayed diagnosis and optimize patient outcomes.
| 1. | Li Y, Zuo JL, Tang JS, Shen XY, Xu SH, Xiao JL. Primary nonkeratinizing squamous cell carcinoma of the scapular bone: A case report. World J Clin Cases. 2021;9:976-982. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Dopazo C, Diez I, Quintero J, Curell A, González-Junyent C, Caralt M, Pando E, Lázaro JL, Molino JA, Juamperez J, Castells L, Pérez M, Bilbao I, Segarra A, Charco R. Role of Biodegradable Stents as Part of Treatment of Biliary Strictures after Pediatric and Adult Liver Transplantation: An Observational Single-Center Study. J Vasc Interv Radiol. 2018;29:899-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Elsayed G, Mohamed L, Almasaabi M, Barakat K, Gadour E. Hepaticojejunostomy and long-term interventional treatment for recurrent biliary stricture after proximal bile duct injury: A case report. World J Clin Cases. 2025;13:104609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Arabi M, Alrehaili B, Salman R, Qazi S, Bashir O, Abdullah K, Almoaiqel M. Percutaneous Transhepatic Biodegradable Stent Placement for Benign Anastomotic Biliary Strictures: Short-Term Outcomes of a Single-Institution Experience. Arab J Intervent Radiol. 2019;3:19-22. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Lin JW, Cameron JL, Yeo CJ, Riall TS, Lillemoe KD. Risk factors and outcomes in postpancreaticoduodenectomy pancreaticocutaneous fistula. J Gastrointest Surg. 2004;8:951-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 289] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 6. | Kihara Y, Yokomizo H. The clinical features of late postoperative cholangitis following pancreaticoduodenectomy brought on by conditions other than cancer recurrence: a single-center retrospective study. BMC Surg. 2022;22:301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 7. | Goh BK, Chow PK, Quah HM, Ong HS, Eu KW, Ooi LL, Wong WK. Perforation of the gastrointestinal tract secondary to ingestion of foreign bodies. World J Surg. 2006;30:372-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 222] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 8. | Anvari S, Lee Y, Patro N, Soon MS, Doumouras AG, Hong D. Double-balloon enteroscopy for diagnostic and therapeutic ERCP in patients with surgically altered gastrointestinal anatomy: a systematic review and meta-analysis. Surg Endosc. 2021;35:18-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/