Published online Dec 6, 2025. doi: 10.12998/wjcc.v13.i34.111668
Revised: August 3, 2025
Accepted: November 20, 2025
Published online: December 6, 2025
Processing time: 152 Days and 21.6 Hours
Low-grade appendiceal mucinous neoplasms are papillary or flat mucinous tum
We report a 54-year-old patient who presented with a 10-month history of cons
Low-grade appendiceal mucinous adenomas are rare tumors that are easily misd
Core Tip: We report a middle-aged patient who presented with persistent, dull abdominal distension and nausea, with symptoms persisting for 10 months. Imaging studies revealed a space-occupying lesion, and the patient subsequently underwent surgical resection. Histopathological examination confirmed the diagnosis of low-grade appendiceal mucinous neoplasm. Following surgery, the patient received intraperitoneal hyperthermic chemotherapy with cisplatin and was discharged in stable condition.
- Citation: Deng X, Lv LY, Jiang SX, Huang JX, Chen XY, Zhang MF, Qi J, Yang M. Low-grade appendiceal mucinous neoplasm: A case report. World J Clin Cases 2025; 13(34): 111668
- URL: https://www.wjgnet.com/2307-8960/full/v13/i34/111668.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i34.111668
Low-grade appendiceal mucinous neoplasm (LAMN) is rare disease constituting about 1% of all colorectal malignancies. The incidence of LAMN among appendectomy specimens is reported to be 0.3%-0.7%[1]. The incidence rate of LAMN is rising. The peak age of onset of LAMN is after 50 years old, slightly higher in females than males. The symptoms are not specific. Clinically, it is often diagnosed based on abdominal pain, abdominal mass or symptoms of acute appendicitis. The most serious complication is the perforation of the appendix, which leads to peritoneal seeding and forms peritoneal pseudomyxoma. The rupture of an otherwise asymptomatic and stable LAMN can seed the peritoneal cavity with mucin and neoplastic epithelium, subsequently giving rise to pseudomyxoma peritonei (PMP).
A 54-year-old female complained of constant dull distension in upper quadrant abdomen accompanied with nausea for 10 months.
She denied any other discomforts, such as fever, vomiting, abdominal pain. She received a gastroscopy at the local hospital, which showed chronic gastritis, and was treated with vonoprazan, mosapride. However, the symptoms were progressively worsening in 2 months.
There was no past illness.
There was no significant personal and family history.
At admission, physical examination noted abdominal distension, epigastric tenderness, and shifting dullness positive, while right lower quadrant tenderness, McBurney’s point tenderness, and peritonitis signs were negative.
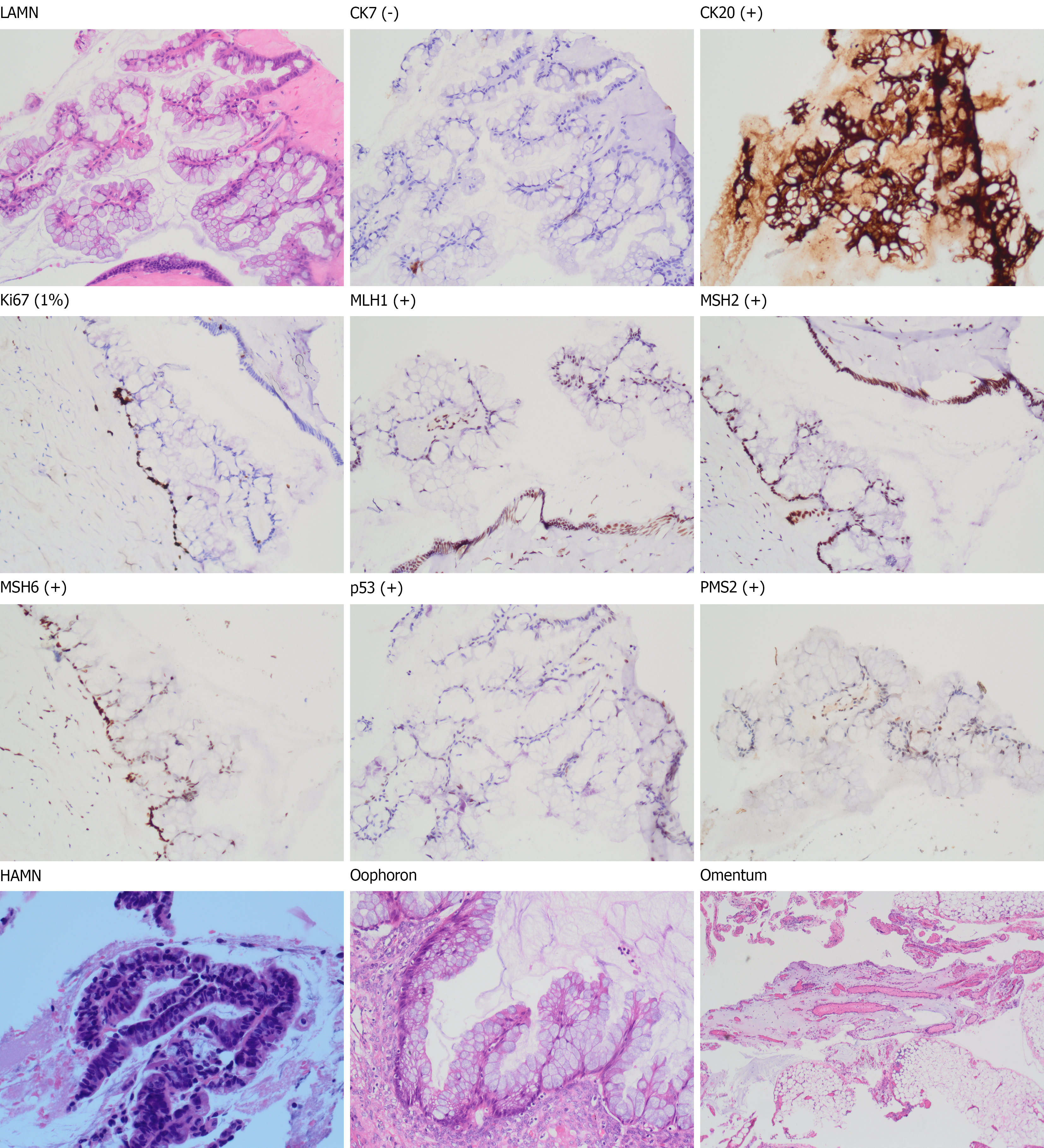
Labs showed carcinoembryonic antigen 19.72 ng/mL, cancer antigen (carbohydrate antigen 125) 72.05 U/mL. She underwent surgery and the pathology showed LAMN, and high-grade mucinous adenomas were present in focal areas (Figure 1).
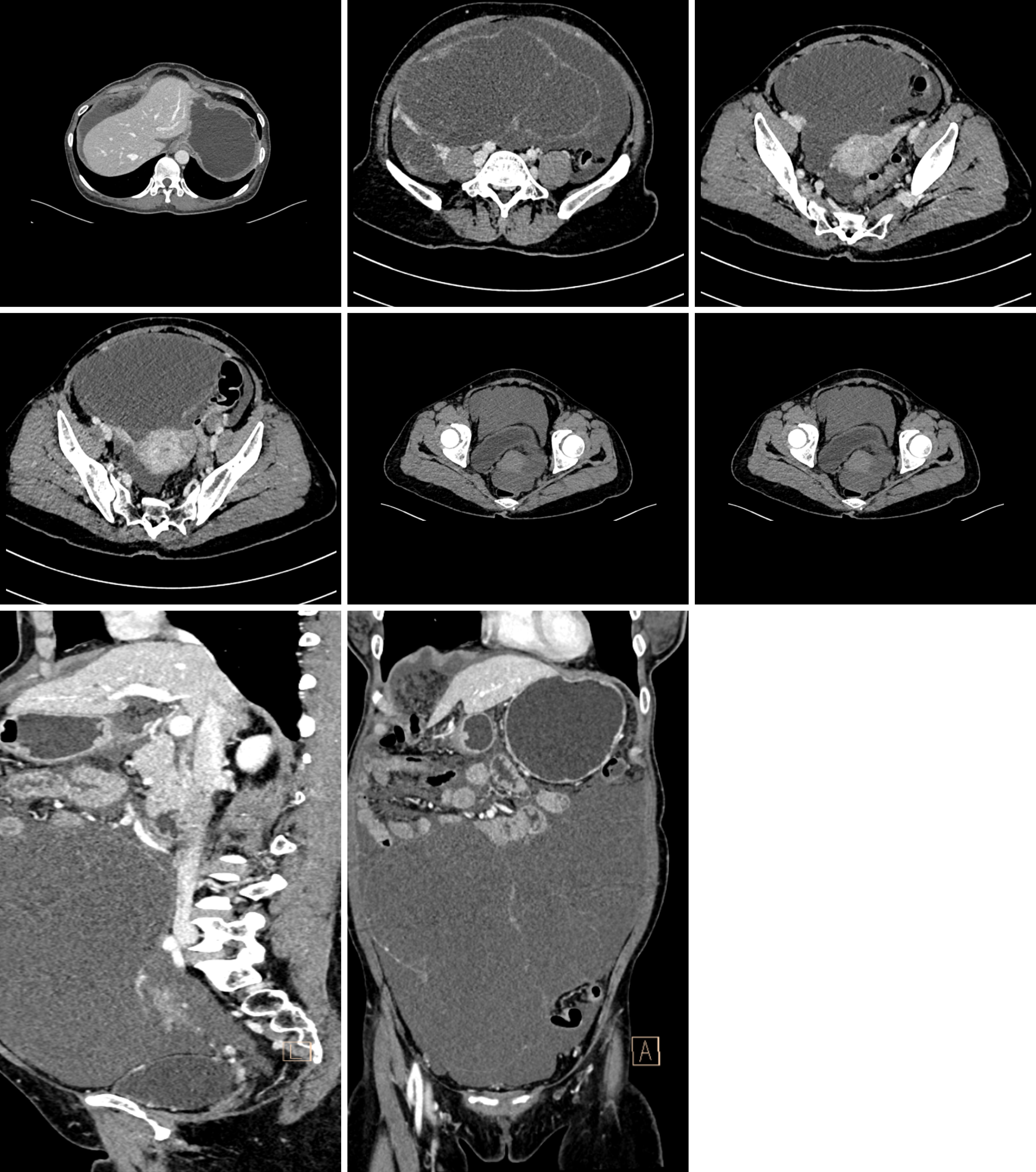
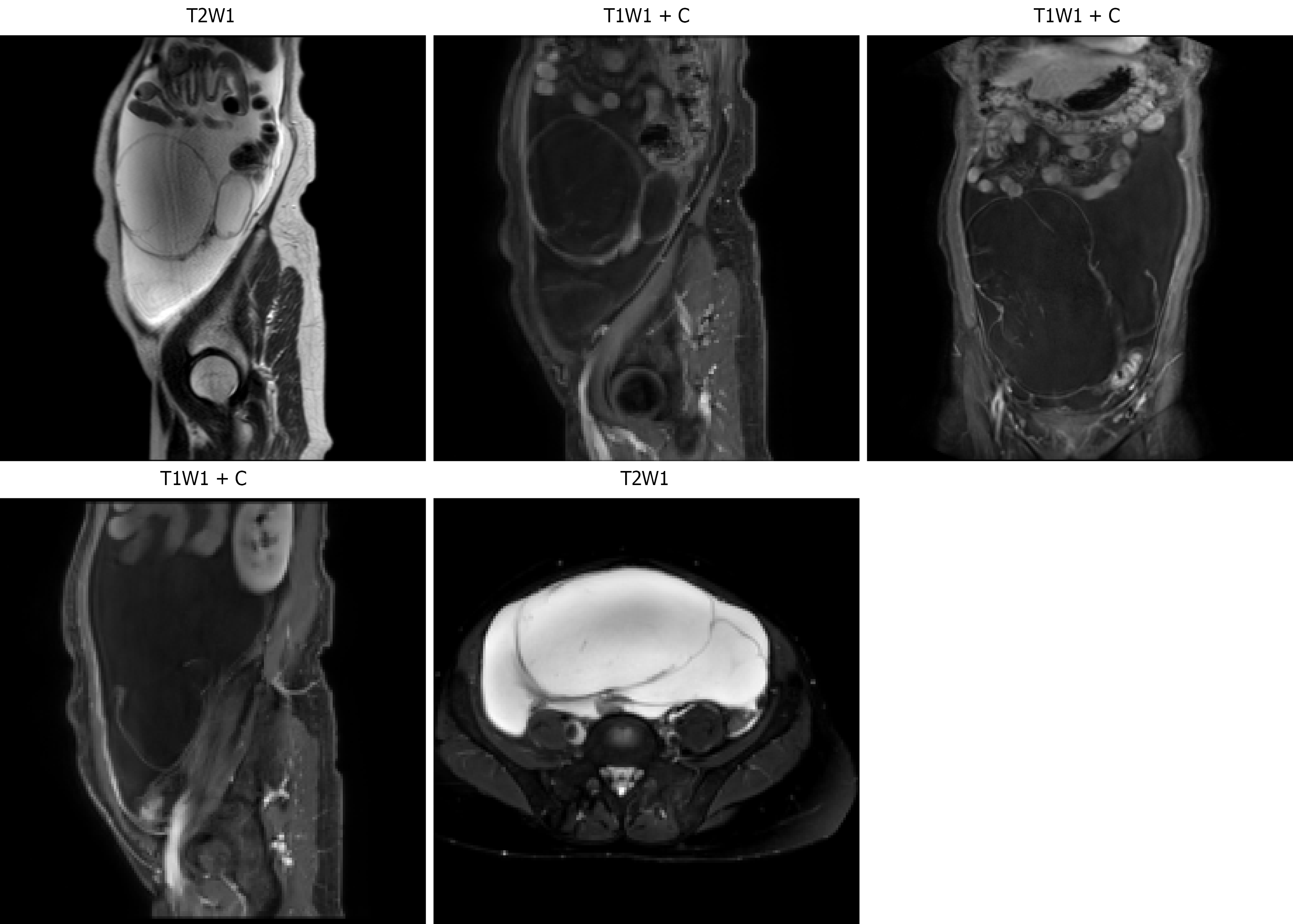
Computed tomography scan of abdomen with contrast showed a huge multilocular cystic mass (187 mm × 117 mm × 206 mm) in the abdomen and pelvic considered ovarian cystadenoma possible, and peritoneum is thickened and blurred, peritoneal metastases needed to be excluded (Figure 2). Magnetic resonance imaging suggested a high possibility of right ovarian cystadenoma. Transvaginal gynecological ultrasound showed a huge cystic mass in the abdominal cavity classified as ovarian-adnexal reporting and data system 5 type, which was considered originating from the right ovary and having ruptured possibly (Figure 3).
LAMN, staged as pT4aM1c.
A surgery of total hysterectomy, bilateral adnexectomy, appendectomy, greater omentectomy and right hemicolectomy were performed for diagnosis and treatment. After the surgery, she received hyperthermic intraperitoneal chemotherapy (HIPEC) with cisplatin.
She discharged from the hospital after HIPEC. However, a follow-up examination at the local hospital 3 months later suggested residual and recurrent tumor, and she underwent surgery again and recovered well after the operation.
Mucinous neoplasia of the appendix is a rare condition that occurs in approximately 1% of the patients undergoing appendectomy[2], or even lower[3]. LAMNs are three times more likely to affect females than males and are typically found in patients between the ages of 50-60 years. Ultrasound examinations and computed tomography scans are very useful diagnostic methods. However, the diagnostic results are often discovered during surgeries for appendicitis and other abdominal organ diseases. Appendiceal mucinous neoplasm is commonly misdiagnosed as acute appendicitis, adnexal mass and retroperitoneal tumors. While this case is in disguise of ovarian cystadenoma. And confirmed dia
Low-grade appendiceal mucinous adenomas are rare tumors that are easily misdiagnosed, and a more thorough clinical workup is required to make a definitive diagnosis.
We sincerely thank all the authors for their valuable contributions to this research.
| 1. | Tarabishi J, Douedari A, Almasalmeh T, Tarzi M. LAMN as a differential diagnosis for abdominal pain: a case report from Syria. J Surg Case Rep. 2022;2022:rjab585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Sueda T, Murata K, Takeda T, Kagawa Y, Hasegawa J, Komori T, Noura S, Ikeda K, Tsujie M, Ohue M, Ota H, Ikenaga M, Hata T, Matsuda C, Mizushima T, Yamamoto H, Sekimoto M, Nezu R, Mori M, Doki Y. Survival outcomes of appendiceal mucinous neoplasms by histological type and stage: Analysis of 266 cases in a multicenter collaborative retrospective clinical study. Ann Gastroenterol Surg. 2019;3:291-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Köhler F, Reese L, Hendricks A, Kastner C, Müller S, Lock JF, Germer CT, Wiegering A. Low-grade mucinous neoplasms (LAMN) of the appendix in Germany between 2011 and 2018: a nationwide analysis based on data provided by the German Center for Cancer Registry Data (ZfKD) at the Robert Koch Institute (RKI). Langenbecks Arch Surg. 2022;407:3615-3622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 4. | Pai RK, Beck AH, Norton JA, Longacre TA. Appendiceal mucinous neoplasms: clinicopathologic study of 116 cases with analysis of factors predicting recurrence. Am J Surg Pathol. 2009;33:1425-1439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 170] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 5. | Han Z, Liu X, Tian Y, Shen S, Wang H, Hu S, Wu X, Yan Z, Lu C, Wang P, Bai Y, Kong Y, Wang L, Cao S, Li Z, Zhong H, Meng C, Zhou Y. Long term survival outcomes of surgery combined with hyperthermic intraperitoneal chemotherapy for perforated low-grade appendiceal mucinous neoplasms: A multicenter retrospective study. World J Surg. 2024;48:86-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | González-Moreno S, Brun E, Sugarbaker PH. Lymph node metastasis in epithelial malignancies of the appendix with peritoneal dissemination does not reduce survival in patients treated by cytoreductive surgery and perioperative intraperitoneal chemotherapy. Ann Surg Oncol. 2005;12:72-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Baratti D, Kusamura S, Nonaka D, Cabras AD, Laterza B, Deraco M. Pseudomyxoma peritonei: biological features are the dominant prognostic determinants after complete cytoreduction and hyperthermic intraperitoneal chemotherapy. Ann Surg. 2009;249:243-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Chua TC, Moran BJ, Sugarbaker PH, Levine EA, Glehen O, Gilly FN, Baratti D, Deraco M, Elias D, Sardi A, Liauw W, Yan TD, Barrios P, Gómez Portilla A, de Hingh IH, Ceelen WP, Pelz JO, Piso P, González-Moreno S, Van Der Speeten K, Morris DL. Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Clin Oncol. 2012;30:2449-2456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 658] [Cited by in RCA: 812] [Article Influence: 58.0] [Reference Citation Analysis (0)] |
| 9. | Elias D, Gilly F, Quenet F, Bereder JM, Sidéris L, Mansvelt B, Lorimier G, Glehen O; Association Française de Chirurgie. Pseudomyxoma peritonei: a French multicentric study of 301 patients treated with cytoreductive surgery and intraperitoneal chemotherapy. Eur J Surg Oncol. 2010;36:456-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 191] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 10. | Enblad M, Birgisson H, Wanders A, Sköldberg F, Ghanipour L, Graf W. Importance of Absent Neoplastic Epithelium in Patients Treated With Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy. Ann Surg Oncol. 2016;23:1149-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/