Published online Nov 26, 2025. doi: 10.12998/wjcc.v13.i33.113751
Revised: September 24, 2025
Accepted: October 28, 2025
Published online: November 26, 2025
Processing time: 80 Days and 8.1 Hours
Erythrodermic psoriasis (EP) is a rare and life-threatening form of psoriasis associated with significant morbidity and mortality. Systemic immunosuppre
We describe a 49-year-old man with longstanding severe plaque psoriasis, liver cirrhosis, and bipolar disorder who developed EP involving > 90% of body surface area [Psoriasis Area and Severity Index (PASI) 45]. Following initial stabilization, he was admitted to the intensive care unit (ICU) with hemodynamic instability, leukocytosis with eosinophilia, and diffuse desquamation. Ixekizumab was initiated with high-dose topical clobetasol. During his ICU stay, he developed recurrent bacteremias and neurologic decline (Glasgow Coma Scale 7/15), fo
This case highlights the diagnostic and therapeutic challenges of managing EP in the setting of biologic therapy. Disseminated cutaneous HSV-1 should be considered in immunosuppressed patients presenting with new vesicular eruptions, and prompt PCR testing with early antiviral therapy is essential. A multidisciplinary approach is critical to balance immunosuppression for disease control with infection risk.
Core Tip: Erythrodermic psoriasis (EP) is a rare, severe form of psoriasis associated with high morbidity and mortality. Management frequently requires systemic immunosuppression, which increases susceptibility to opportunistic infections. We describe a patient with EP who developed disseminated herpes simplex virus type 1 while receiving biologic and corticosteroid therapy. This case emphasizes the importance of early recognition of vesicular eruptions, timely diagnostic testing, and prompt antiviral therapy. Clinicians must balance disease control with infection risk, highlighting the need for vigilant monitoring and multidisciplinary management in EP.
- Citation: Berjawi A, Attieh R, Younes M, Beydoun K, Fassih I, Tannous Z. Disseminated herpes simplex virus type 1 treated with ixekizumab in a patient with erythrodermic psoriasis: A case report. World J Clin Cases 2025; 13(33): 113751
- URL: https://www.wjgnet.com/2307-8960/full/v13/i33/113751.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i33.113751
Erythrodermic psoriasis (EP) is an uncommon and severe manifestation of psoriasis vulgaris, with an estimated prevalence of 1%-2.25% among patients with psoriasis[1]. It is the leading cause of erythroderma, accounting for approximately one-quarter of cases, and carries high morbidity and mortality due to complications such as fluid loss, electrolyte imbalance, infection, and cardiovascular instability[1].
Management of EP is complex and often requires systemic immunosuppressive agents, including cyclosporine, methotrexate, and biologics such as infliximab and ixekizumab[2]. While these therapies can achieve disease control, they may increase susceptibility to opportunistic or disseminated infections. Disseminated herpes simplex virus type-1 (HSV-1) infection is rarely reported in otherwise immunocompetent individuals, and its occurrence during treatment of EP has not been described previously.
In the present case, HSV-1 involvement was confined to the skin without evidence of visceral disease. Such a pre
This case report was prepared in accordance with the CARE (CAse REport) guidelines, which provide a structured framework for transparent and comprehensive case reporting[5]. We present the case of a 49-year-old man with EP complicated by cutaneous disseminated HSV-1 infection following biologic and corticosteroid therapy, highlighting the diagnostic and therapeutic challenges encountered in balancing immunosuppression with infection control.
A 49-year-old man presented with rapidly progressive generalized erythema, scaling, and edema involving more than 90% of his body surface area (BSA), accompanied by fever, chills, and altered consciousness.
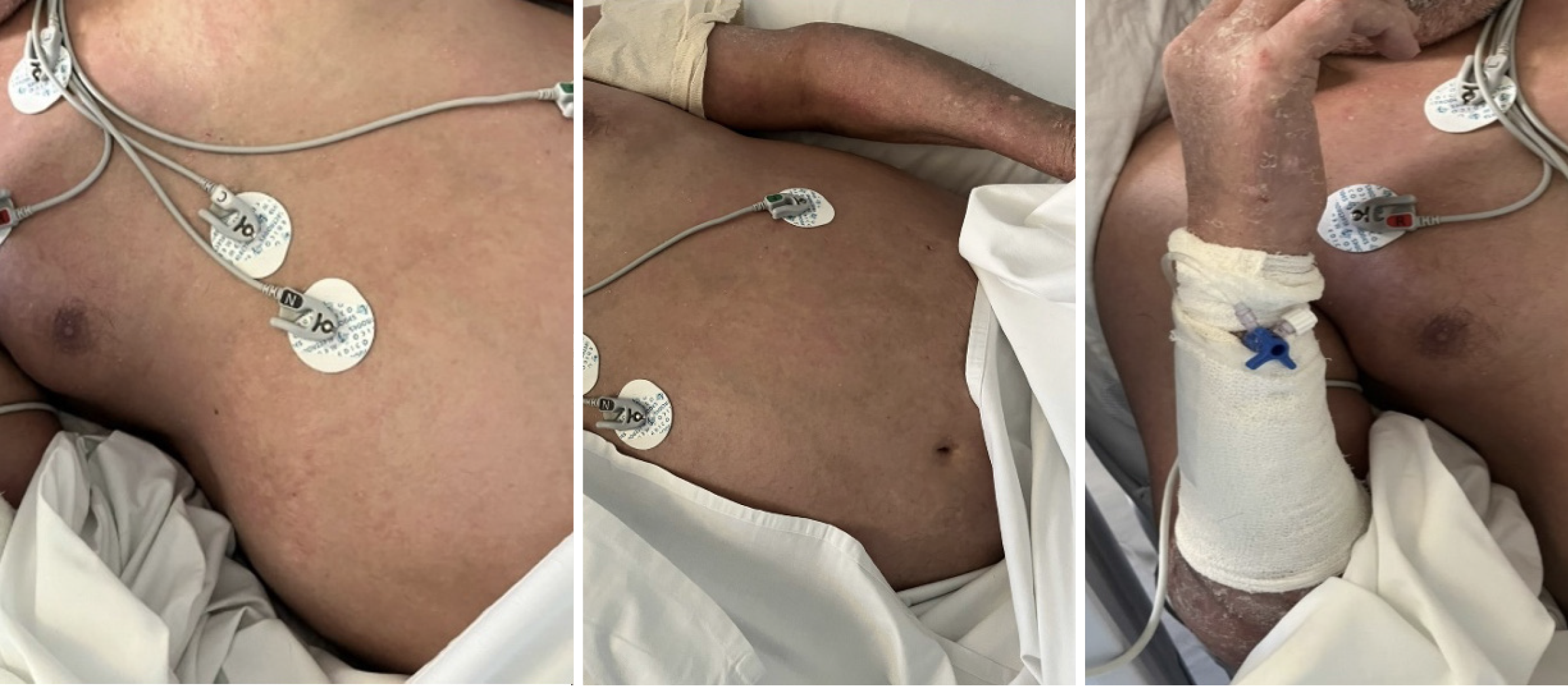
Two weeks before admission, the patient developed worsening erythema and scaling that began on the upper extremities and rapidly progressed to involve over 75% of his BSA (Figure 1). He self-initiated oral prednisone, which was sub
The patient had a 10-year history of severe plaque psoriasis refractory to multiple systemic agents, including meth
The patient was married and lived with his family. He reported no history of alcohol use, smoking, or illicit drug use. There was no family history of psoriasis, autoimmune disease, or dermatologic disorders.
At ICU admission, vital signs were blood pressure 85/55 mmHg, heart rate 125 beats/minutes, temperature 39.0 °C, respiratory rate 28/minutes, and oxygen saturation 91% on 2 L/minutes oxygen. Examination revealed diffuse confluent erythema with scaling involving > 90% of BSA, generalized edema, and desquamation. No ulcerations were noted initially. During his ICU stay, the patient developed widespread vesicles, erosions, and hemorrhagic crusts. Neurologic assessment showed a Glasgow Coma Scale score of 7/15, necessitating intubation.
Initial laboratory studies demonstrated leukocytosis (17.2 × 109/L), eosinophilia (1.2 × 109/L), elevated C-reactive protein (120 mg/L), hypoalbuminemia (2.6 g/dL), and mild hyponatremia (Na 131 mmol/L). Renal function was preserved (creatinine 0.9 mg/dL). HSV-1 polymerase chain reaction (PCR) from vesicular swabs was positive.
No radiologic imaging was required for diagnosis.
Given the patient’s critical condition and overlapping dermatologic and infectious complications, a multidisciplinary team was assembled. The consultation included dermatology, infectious diseases, critical care, and gastroenterology specialists.
The dermatology team guided the diagnosis of erythrodermic psoriasis and recommended initiation of biologic therapy with ixekizumab after failure of infliximab. The infectious diseases team managed recurrent bacteremias and directed antiviral therapy once disseminated HSV-1 was confirmed. The critical care team stabilized the patient’s hemodynamic status, managed airway protection during neurologic decline, and coordinated supportive care. The gastroenterology team provided input on the management of underlying liver cirrhosis, portal hypertension, and medication safety in the context of hepatic dysfunction.
Consensus was reached to temporarily withhold immunosuppressive therapy during active HSV-1 infection, initiate intravenous acyclovir, and later reintroduce ixekizumab cautiously once the viral lesions had resolved.
Erythrodermic psoriasis complicated by disseminated cutaneous herpes simplex virus type-1 infection in the context of biologic (ixekizumab) and corticosteroid therapy.
Upon ICU admission, the patient was stabilized with intravenous fluids and empiric broad-spectrum antibiotics, later de-escalated based on culture results. Ixekizumab was initiated along with high-potency topical corticosteroids (clobetasol propionate 0.05%, approximately 30 g/day). During the ICU course, the patient developed recurrent bacteremias and a widespread vesicular eruption. HSV-1 PCR confirmed disseminated infection. Ixekizumab and corticosteroids were withheld, and intravenous acyclovir (5 mg/kg every 8 hours) was started with renal function monitoring. Following ten days of antiviral therapy and resolution of cutaneous lesions, ixekizumab was reintroduced with cautious tapering of topical corticosteroids (Table 1, Figures 2 and 3).
| Date/interval | Clinical events | Investigations/labs/vitals | Interventions | Outcomes |
| 2 weeks before first hospital admission | Severe itching and erythema of upper extremities progressing rapidly | - | Self-initiated oral prednisone (unprescribed) → discontinued at dermatology visit; switched to topical corticosteroids and moisturizers | Erythema progressed to > 75% BSA |
| 3 days later | Worsening erythema with fever | Vitals: BP 115/70 mmHg, HR 110 bpm, Temp | Infliximab infusion (5 mg/kg) | No improvement; admitted for first hospitalization |
| First hospital admission | Diffuse erythema (> 75% BSA) with fever | As above | Broad-spectrum antibiotics → de-escalated to MSSA coverage; discharged on oral Augmentin | Temporary stabilization |
| 10 days later (second admission, ICU) | Increasing chills, diffuse edema, worsening erythema (> 90% BSA). PASI 45 calculated | Vitals: BP 85/55 mmHg, HR 125 bpm, Temp | ICU admission; fluid resuscitation | Hemodynamically unstable |
| Early ICU course (second admission) | Confluent erythroderma and desquamation | Punch biopsy performed: Hypogranulosis, ectatic dermal vessels, neutrophils in stratum corneum, scattered dermal eosinophils | Ixekizumab initiated; topical clobetasol approximately 30 g/day | Recurrent bacteremias; progressive decline in consciousness (GCS 7/15); intubated |
| 1 week after ixekizumab | Disseminated vesicles, erosions, hemorrhagic crusts (Figure 2) | HSV-1 PCR positive | IV acyclovir 5 mg/kg q8h; clobetasol stopped; ixekizumab withheld | Gradual clinical improvement |
| 10 days later | Improvement in HSV lesions | - | Topical corticosteroids reintroduced; ixekizumab restarted | Steady recovery (Figure 3) |
| 6-week follow-up | Resolution of widespread erythema and palmoplantar scaling (PASI 9.7) | - | Continued ixekizumab; oral acyclovir prophylaxis | Stable improvement; no relapses (Figure 3) |
The patient demonstrated steady improvement after antiviral therapy and reinitiation of ixekizumab. By six weeks, his Psoriasis Area and Severity Index (PASI) had improved from 45 to 9.7, with resolution of widespread erythema and palmoplantar scaling. He was discharged on oral acyclovir prophylaxis, which was continued for six months. At follow-up visits, the patient remained clinically stable with no relapses or new adverse events.
To our knowledge, no published articles have reported disseminated HSV-1 infection in the setting of erythrodermic psoriasis treated with ixekizumab in combination with topical corticosteroids. This case underscores the complexity of managing severe psoriasis while balancing the risks of immunosuppression and opportunistic infection.
EP is frequently precipitated by abrupt withdrawal of systemic therapy, including corticosteroids, cyclosporine, or methotrexate. Its pathogenesis is not fully understood, although an increased T helper 2 immune response has been proposed as a mechanism that may predispose to disseminated viral infections such as eczema herpeticum or Kaposi varicelliform eruption[3]. In line with recommendations from the National Psoriasis Foundation, first-line therapy for severe EP includes infliximab or cyclosporine[2]. In our case, infliximab was attempted after prior cyclosporine failure. Despite this, the patient deteriorated, and the presence of eosinophils on skin biopsy suggested a possible paradoxical drug reaction. Given the patient’s history of partial response to ixekizumab, this biologic was reintroduced with topical clobetasol as primary therapy. The subsequent emergence of disseminated HSV-1 infection highlights a rare but im
Disseminated HSV-1 infection is exceptionally rare in immunocompetent individuals and has been described only in isolated case reports[6-9]. In our patient, multiple factors likely contributed to susceptibility, including recent infliximab exposure, initiation of ixekizumab, and concurrent use of high-dose topical corticosteroids. Disseminated herpes zoster is more frequently reported than disseminated HSV-1, particularly in immunosuppressed populations such as patients with AIDS or those receiving mycophenolate and tacrolimus[7]. It has also been observed during the coronavirus disease 2019 pandemic in patients receiving immunomodulatory therapy, including high-dose corticosteroids[8]. Isolated reports document systemic HSV-1 infection following oral corticosteroid therapy alone[9], or in the context of infliximab therapy for rheumatoid arthritis[10]. These observations support the conclusion that both biologics and corticosteroids may serve as predisposing factors for disseminated herpes infections.
Our patient’s diagnosis was established by PCR confirmation of HSV-1, emphasizing the importance of maintaining a high index of suspicion in immunosuppressed patients presenting with new vesicular or erosive lesions. The differential diagnosis is broad and includes Stevens-Johnson syndrome, drug reaction with eosinophilia and systemic symptoms, bullous pemphigoid, and vasculitic eruptions. Early virologic testing is therefore critical to distinguish disseminated HSV-1 from these mimics, as timely antiviral therapy can be lifesaving.
Ixekizumab is a monoclonal antibody targeting interleukin-17A, with demonstrated efficacy and an acceptable safety profile in psoriasis, psoriatic arthritis, and ankylosing spondylitis[11-15]. However, infections remain a theoretical and increasingly recognized risk. A 2020 case report documented herpes zoster following ixekizumab in a patient with erythrodermic psoriasis[16], and our case extends these observations by describing disseminated HSV-1 under similar conditions. This raises the possibility that patients with severe EP and extensive skin barrier compromise may be particularly vulnerable to viral reactivation or dissemination when treated with biologics.
In summary, this case illustrates the therapeutic challenges of managing erythrodermic psoriasis in the presence of multiple comorbidities. Disseminated HSV-1 should be considered in the differential diagnosis of new vesicular eruptions in immunosuppressed patients with EP. Prompt recognition, PCR confirmation, and initiation of antiviral therapy were essential for the favorable outcome observed. A multidisciplinary approach remains indispensable in balancing disease control with infection risk in this fragile patient population.
This case illustrates the therapeutic challenges of managing erythrodermic psoriasis in a patient with multiple comorbidities. Disseminated HSV-1 should be considered in the differential diagnosis of new vesicular eruptions in immunosuppressed patients with psoriasis. Timely PCR confirmation, prompt antiviral therapy, and cautious reintroduction of biologics were critical to achieving a favorable outcome. Clinicians should remain vigilant for severe opportunistic infections when treating erythrodermic psoriasis with ixekizumab or other biologics.
The authors thank the intensive care, dermatology, infectious diseases, and gastroenterology teams involved in the management of this patient.
| 1. | Singh RK, Lee KM, Ucmak D, Brodsky M, Atanelov Z, Farahnik B, Abrouk M, Nakamura M, Zhu TH, Liao W. Erythrodermic psoriasis: pathophysiology and current treatment perspectives. Psoriasis (Auckl). 2016;6:93-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Rosenbach M, Hsu S, Korman NJ, Lebwohl MG, Young M, Bebo BF Jr, Van Voorhees AS; National Psoriasis Foundation Medical Board. Treatment of erythrodermic psoriasis: from the medical board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:655-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 102] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Leung DY, Bieber T. Atopic dermatitis. Lancet. 2003;361:151-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1017] [Cited by in RCA: 967] [Article Influence: 42.0] [Reference Citation Analysis (0)] |
| 4. | Wollenberg A, Zoch C, Wetzel S, Plewig G, Przybilla B. Predisposing factors and clinical features of eczema herpeticum: a retrospective analysis of 100 cases. J Am Acad Dermatol. 2003;49:198-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 190] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 5. | Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. 2014;67:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 446] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 6. | Boivin G, Malette B, Goyette N. Disseminated herpes simplex virus type 1 primary infection in a healthy individual. Can J Infect Dis Med Microbiol. 2009;20:122-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Petrun B, Williams V, Brice S. Disseminated varicella-zoster virus in an immunocompetent adult. Dermatol Online J. 2015;21:13030/qt3cz2x99b. [PubMed] |
| 8. | Voisin O, Deluca N, Mahé A, Lelorc'h E, Hubert S, Ménage E, Borie MF, Azria P, Fite C, Pilmis B, Mourad JJ. Disseminated Herpes Zoster During COVID-19. Infect Dis Clin Pract (Baltim Md). 2021;29:e109-e110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Kim M, Jalal A, Rubio-Gomez H, Bromberg R. A case report of severe systemic herpes simplex virus-1 (HSV-1) infection with multi-organ involvement after a course of oral corticosteroid treatment. BMC Infect Dis. 2022;22:817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 10. | Justice EA, Khan SY, Logan S, Jobanputra P. Disseminated cutaneous Herpes Simplex Virus-1 in a woman with rheumatoid arthritis receiving infliximab: a case report. J Med Case Rep. 2008;2:282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Markham A. Ixekizumab: First Global Approval. Drugs. 2016;76:901-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Lespessailles E, Toumi H. Ixekizumab in the treatment of psoriatic arthritis. Immunotherapy. 2021;13:19-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Blauvelt A, Lebwohl MG, Mabuchi T, Leung A, Garrelts A, Crane H, ElMaraghy H, Patel H, Ridenour T, See K, Gallo G, Paul C. Long-term efficacy and safety of ixekizumab: A 5-year analysis of the UNCOVER-3 randomized controlled trial. J Am Acad Dermatol. 2021;85:360-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 14. | Leonardi C, Reich K, Foley P, Torii H, Gerdes S, Guenther L, Gooderham M, Ferris LK, Griffiths CEM, ElMaraghy H, Crane H, Patel H, Burge R, Gallo G, Shrom D, Leung A, Lin CY, Papp K. Efficacy and Safety of Ixekizumab Through 5 Years in Moderate-to-Severe Psoriasis: Long-Term Results from the UNCOVER-1 and UNCOVER-2 Phase-3 Randomized Controlled Trials. Dermatol Ther (Heidelb). 2020;10:431-447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 15. | Genovese MC, Mysler E, Tomita T, Papp KA, Salvarani C, Schwartzman S, Gallo G, Patel H, Lisse JR, Kronbergs A, Leage SL, Adams DH, Xu W, Marzo-Ortega H, Lebwohl MG. Safety of ixekizumab in adult patients with plaque psoriasis, psoriatic arthritis and axial spondyloarthritis: data from 21 clinical trials. Rheumatology (Oxford). 2020;59:3834-3844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 16. | Pruneda CC, Austin BA, Wallis DT, Paulger BR, Tarbox MB. Ixekizumab and herpes zoster in an erythrodermic patient. Proc (Bayl Univ Med Cent). 2020;33:417-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/