Published online Nov 26, 2025. doi: 10.12998/wjcc.v13.i33.113560
Revised: September 25, 2025
Accepted: November 5, 2025
Published online: November 26, 2025
Processing time: 84 Days and 23.5 Hours
Venlafaxine, a serotonin-norepinephrine reuptake inhibitor, is widely prescribed for the treatment of major depressive disorder. At therapeutic dose, it is generally safe, with a low incidence of adverse effects. However, massive venlafaxine inge
A 31-year-old woman with a history of depression ingested 14.8 g of venlafaxine along with 6 mg of estazolam and 6 mg of flunitrazepam. On admission, 2 hours post-ingestion, she presented only with mild QTc prolongation. At 4 hours post-ingestion, she developed a generalized tonic-clonic seizure. Following endo
In cases of massive venlafaxine ingestion, continuous intensive monitoring, particularly of QTc, is essential for at least 24 hours, even when initial clinical signs are mild. If refractory ventricular arrhythmias occur, prompt ini
Core Tip: A 31-year-old woman ingested a massive dose of venlafaxine (14.8 g) and initially showed only mild QTc pro
- Citation: Mori K, Kamijo Y, Doi T, Abe H, Takeuchi I. Severe venlafaxine poisoning successfully rescued with veno-arterial extracorporeal membrane oxygenation: A case report. World J Clin Cases 2025; 13(33): 113560
- URL: https://www.wjgnet.com/2307-8960/full/v13/i33/113560.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i33.113560
Venlafaxine (VEN) is a serotonin-norepinephrine reuptake inhibitor (SNRI) widely prescribed for the treatment of major depressive disorder. The typical therapeutic dose ranges from 75 mg to 225 mg daily, and at this dose VEN is generally safe, with a low incidence of adverse effects. However, massive ingestion can cause severe cardiotoxicity, leading to life-threating arrhythmias[1-4].
Veno-arterial extracorporeal membrane oxygenation (VA-ECMO) is often employed to manage refractory cardiogenic shock or fatal arrhythmias.
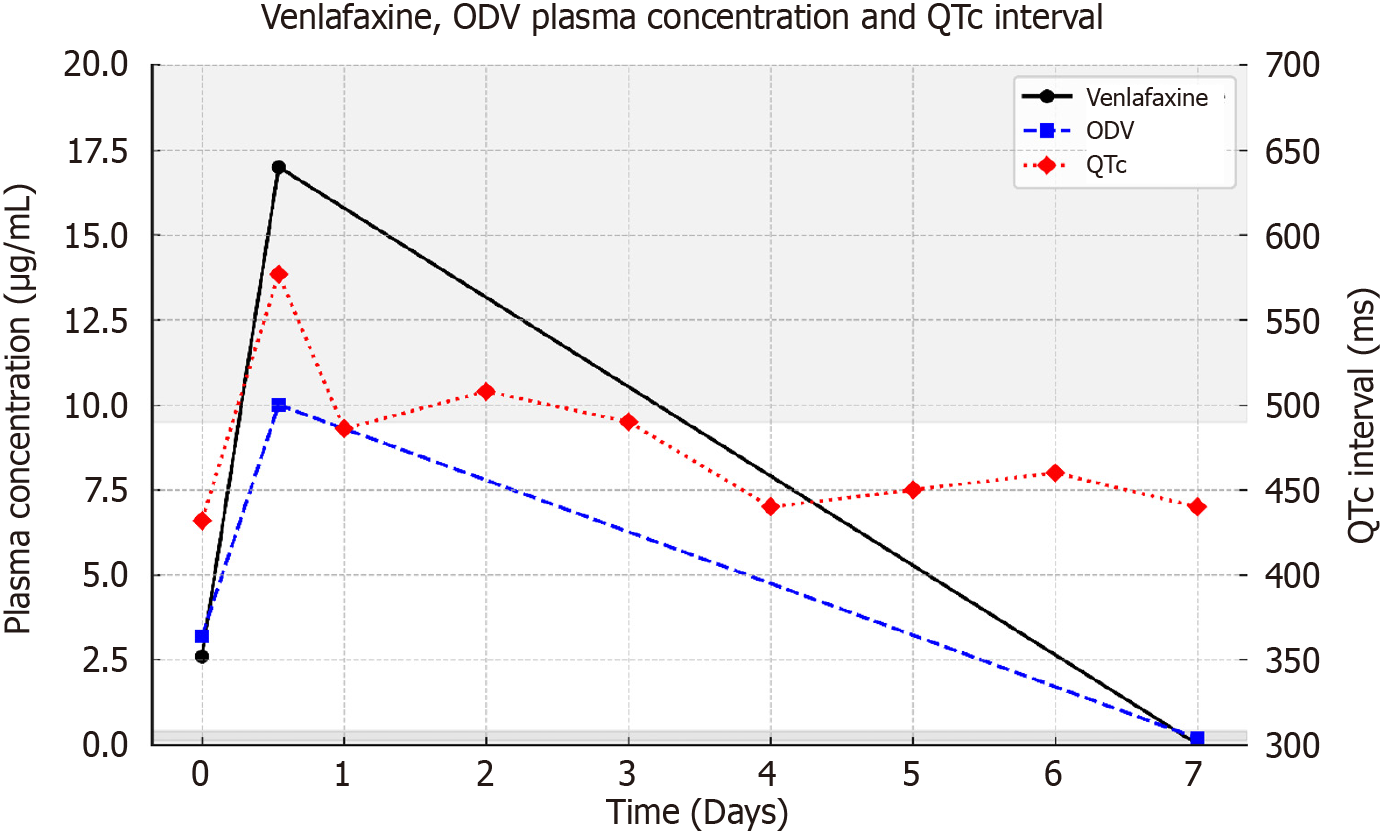
We report a case of massive VEN ingestion in which the patient developed refractory ventricular fibrillation (VF) and was successfully treated with VA-ECMO. In the present case, the patient initially presented with only mild QTc prolongation at 2 hours post-ingestion but developed refractory VF at 15 hours, with QTc prolongation persisting for several days. Serial serum concentrations of VEN and its active metabolite, O-desmethylvenlafaxine (ODV), were determined.
A 31-year-old woman presented to the emergency department following intentional ingestion of a large amount of medication in a suicide attempt.
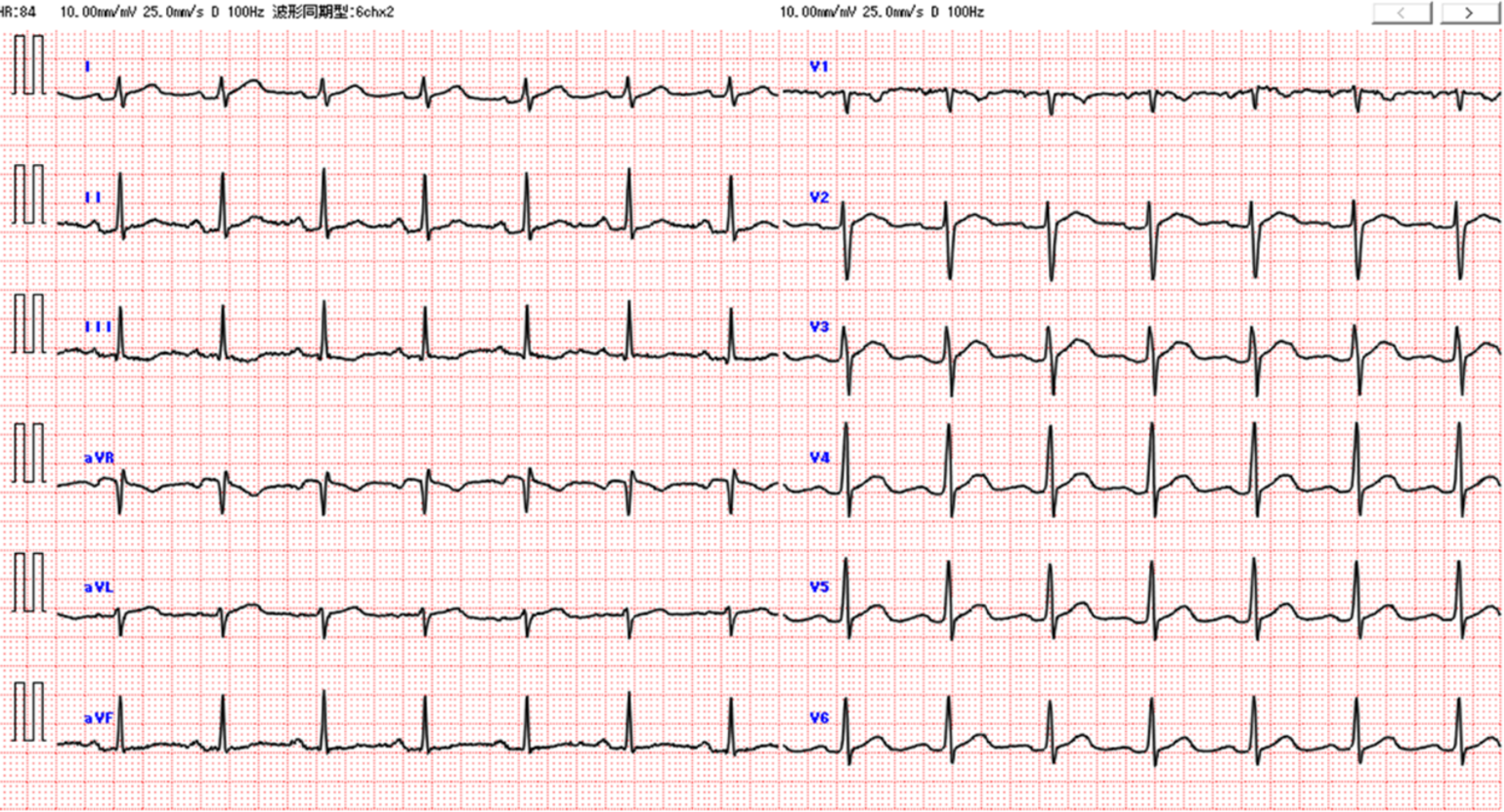
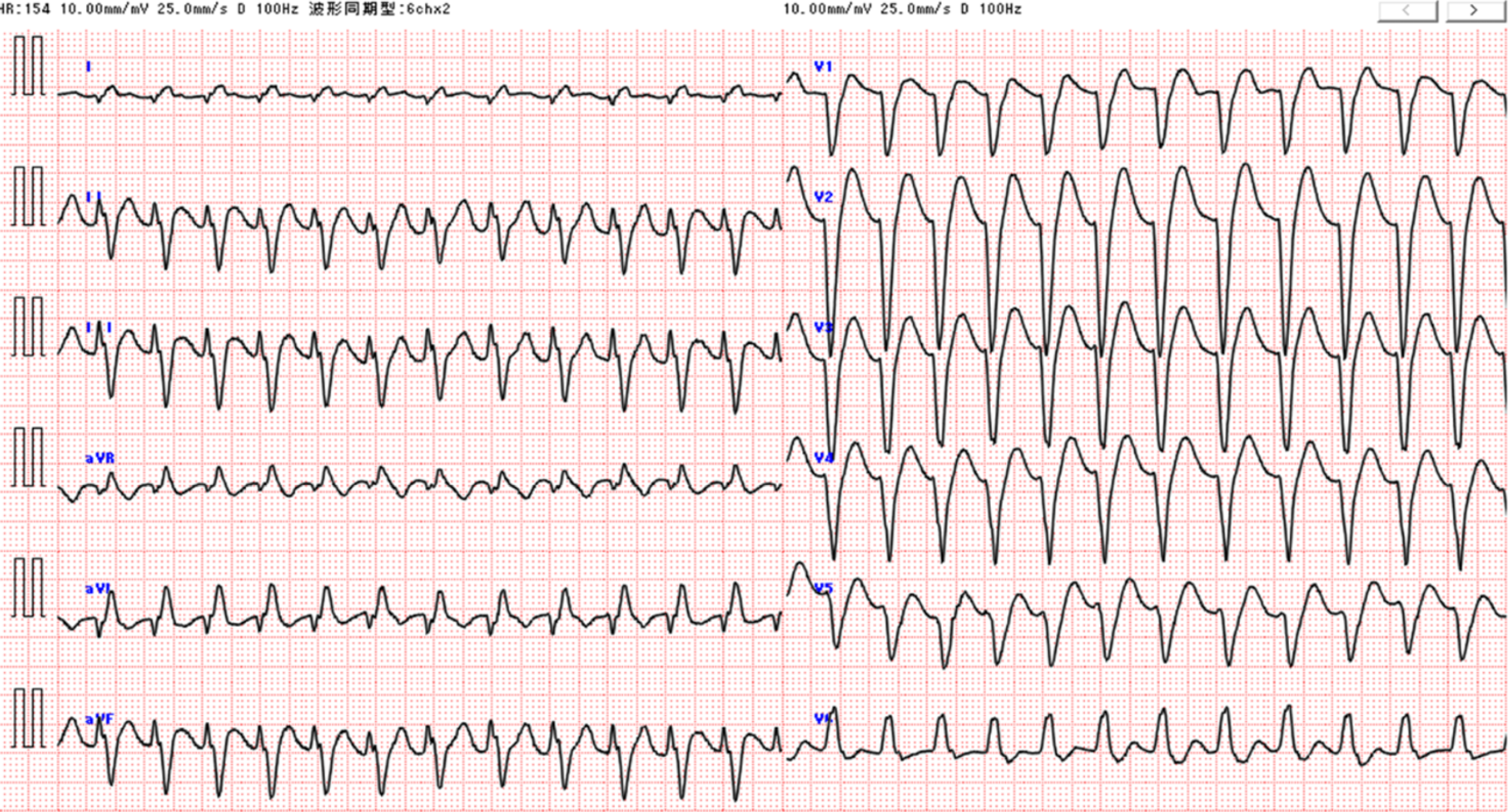
A 31-year-old woman with a history of depression ingested 197 tablets of Effexor XR® 75 mg (total 14.8 g of venlafaxine), three 2 mg tablets of estazolam, and three 2 mg tablets of flunitrazepam in a suicide attempt. She was transported to the emergency department approximately 2 hours after ingestion. On arrival, her vital signs were stable and electrocardiogram (ECG) revealed mild QTc prolongation (432 ms) (Figure 1). Two hours after admission (4 hours post-ingestion), she developed a generalized tonic-clonic seizure, requiring endotracheal intubation and intravenous midazolam. A nasogastric tube was placed, and 50 g of activated charcoal was administered. At 15 hours post-ingestion, she developed ventricular tachycardia progressing to refractory ventricular fibrillation, unresponsive to defibrillation and antiarrhythmic drugs (Figure 2). VA-ECMO was initiated, and sinus rhythm was restored 15 minutes later. QTc remained prolonged over the following 2 days and normalized by hospital day 4. The patient was extubated on day 5 and dis
The patient had a history of depression and was not known to have any other comorbidities.
The patient had a personal history of depression. There was no known family history of psychiatric disorders, car
On arrival at the emergency department, the patient was conscious and alert. Her vital signs were as follows: Blood pressure 138/96 mmHg, heart rate 93 beats per minute, respiratory rate 16 breaths per minute, temperature 36.0 °C, and oxygen saturation 100% on room air. Glasgow Coma Scale score was E4V5M6. No abnormalities were observed on physical examination, and there were no signs of trauma or intoxication.
Initial laboratory tests, including complete blood count, electrolytes, liver and renal function, and arterial blood gas analysis, were within normal limits. Toxicological screening was not immediately available. Subsequent toxicological analysis using LC-MS/MS revealed elevated serum venlafaxine and ODV concentrations: 2.6 µg/mL and 3.2 µg/mL, respectively, at 2 hours post-ingestion, and 17 µg/mL and 10 µg/mL, respectively, at 15 hours post-ingestion.
Chest X-ray and head CT performed on admission revealed no abnormalities.
Consultation with the clinical toxicology department was conducted to evaluate the toxicokinetics and serum concentration profile of venlafaxine and ODV.
Refractory ventricular fibrillation induced by massive venlafaxine overdose, successfully treated with VA-ECMO.
The patient was admitted to the intensive care unit for close observation. Two hours after admission, she developed a generalized tonic-clonic seizure. Endotracheal intubation was performed, and continuous intravenous infusion of midazolam was initiated. A nasogastric tube was inserted, and 50 g of activated charcoal was administered. At 15 hours post-ingestion, the patient developed ventricular tachycardia that rapidly progressed to refractory ventricular fibrillation. Electrical defibrillation and administration of amiodarone and lidocaine were ineffective. VA-ECMO was promptly initiated. Sinus rhythm was restored 15 minutes after extracorporeal membrane oxygenation (ECMO) initiation, and circulatory status stabilized. VA-ECMO was maintained until QTc normalized.
After initiation of VA-ECMO, no further arrhythmias occurred. QTc remained prolonged for 2 days (486 ms on day 2, 508 ms on day 3) and normalized to 433 ms on hospital day 4, at which time ECMO was discontinued. The patient was extubated on day 5, transferred out of the intensive care unit on day 6, and discharged on day 8 without any neurological or cardiac sequelae.
Venlafaxine is primarily metabolized in the liver via cytochrome P450 2D6 (CYP2D6) to ODV. Although venlafaxine is generally considered safe, massive ingestion can cause fatal arrhythmias[1-4]. The QT prolongation seen in this case may be explained by venlafaxine’s inhibition of the hERG potassium channel, which reduces repolarization reserve.
The delayed time to peak plasma concentration (Tmax) and persistently high serum levels in this case suggest delayed gastrointestinal absorption and enzyme saturation, likely due to the massive dose and delayed charcoal administration. Hemodialysis is generally ineffective due to the drug’s large volume of distribution. In contrast, VA-ECMO provides essential circulatory support until venlafaxine is sufficiently metabolized and cardiac function recovers.
Forsberg et al[5] reported a case of a 48-year-old man who ingested 20 g of venlafaxine, developed seizures, Takotsubo cardiomyopathy, and cardiac arrest. The patient was successfully rescued with 36 hours of VA-ECMO. At 24 hours post-ingestion, his serum venlafaxine concentration was 12.6 µg/mL; ODV levels were not reported.
Compared with previous fatal cases[1-4], both the ingested dose and the serum concentrations in this case were within the lethal range. The delayed onset of refractory arrhythmia at 15 hours post-ingestion, despite only mild QTc pro
This case underscores the importance of early consideration of VA-ECMO in patients with SNRI overdose who develop refractory arrhythmias. Continuous ECG monitoring for at least 24 hours is essential, even when initial findings are mild.
Massive venlafaxine overdose can lead to delayed onset of life-threatening arrhythmias despite initially mild symptoms. Continuous ECG monitoring for at least 24 hours is essential. In cases of refractory ventricular arrhythmia, early initiation of VA-ECMO should be considered to improve survival.
We thank the Japanese Society for Clinical Analytical Toxicology (J's-CAT) for their support in the toxicological analysis of this case.
| 1. | Bosse GM, Spiller HA, Collins AM. A fatal case of venlafaxine overdose. J Med Toxicol. 2008;4:18-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Höjer J, Hulting J, Salmonson H. Fatal cardiotoxicity induced by venlafaxine overdosage. Clin Toxicol (Phila). 2008;46:336-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Mazur JE, Doty JD, Krygiel AS. Fatality related to a 30-g venlafaxine overdose. Pharmacotherapy. 2003;23:1668-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Alibegović A, Kariž S, Volavšek M. Fatal overdose with a combination of SNRIs venlafaxine and duloxetine. Forensic Sci Med Pathol. 2019;15:258-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Forsberg S, Abazi L, Forsman P. Successful use of extended cardiopulmonary resuscitation followed by extracorporeal oxygenation after venlafaxine-induced takotsubo cardiomyopathy and cardiac arrest: a case report. J Med Case Rep. 2021;15:485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/