Published online Oct 26, 2025. doi: 10.12998/wjcc.v13.i30.108828
Revised: June 5, 2025
Accepted: August 15, 2025
Published online: October 26, 2025
Processing time: 170 Days and 18.5 Hours
Thyroid cancer is a common malignancy, often found in women. It is the second most common malignant tumor, second only to breast cancer, and it most frequently occurs as papillary thyroid carcinoma (PTC), representing over 90% of cases. PTC frequently presents with lymph node metastases, though in rare cases, patients may experience dysphagia, dyspnea, or hoarseness. In PTC and other differentiated thyroid cancers, direct invasion into major local veins is uncommon, and simultaneous involvement of the vagus nerve is even rarer. Herein, we report a case involving a 50-year-old male patient with a complete invasion of the vagus nerve and the internal jugular vein.
A 50-year-old male discovered a mass on the left side of his neck one year ago. Initially, the mass was approximately 3 cm, but it gradually grew to approximately 6.5 cm in the past month and caused hoarseness. There is no family history of note. On physical examination, a firm, non-tender mass approximately 6.5 cm in diameter was palpated along the lateral border of the left sternocleidomastoid muscle. The mass was irregular in shape, immobile, and did not move with swallowing. The patient has a 5-year history of hypertension with hypokalemia controlled with oral antihypertensive medications (nifedipine and spironolactone). His blood pressure has been maintained between 165-185/112-132 mmHg, and he often reports dizziness. Upon hospitalization, he was dia
The postoperative survival rate for PTC patients is generally good. If clinical signs suggest PTC with recurrent laryngeal nerve involvement, fiberoptic laryngoscopy should be conducted to assess the vocal cords, and intraoperative nerve monitoring is crucial. Preoperative evaluation of the involvement of major neck blood vessels is necessary. Therefore, surgeons should examine signs of large vein damage, as vascular resection and repair or reconstruction are often required. Surgery should be the first choice for differentiated thyroid cancer and radioactive iodine treatment (I-131) should be administered to patients with extrathyroidal invasion or metastasis following total thyroidectomy, followed by TSH suppression therapy.
Core Tip: This study reports a rare case of papillary thyroid carcinoma. The patient underwent two surgeries and recovered well. This unique case provides insights into the treatment guidelines for thyroid cancer. We performed vagus nerve and recurrent laryngeal nerve anastomosis.
- Citation: Li YL, Xia XL, Zhang SY, Tang L, Liu LN, Liu LS. Contralateral metastatic papillary thyroid carcinoma and complicated by primary hyperaldosteronism: A case report. World J Clin Cases 2025; 13(30): 108828
- URL: https://www.wjgnet.com/2307-8960/full/v13/i30/108828.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i30.108828
This study presents a rare case of papillary thyroid carcinoma (PTC) with contralateral neck metastasis involving the internal jugular vein and vagus nerve in a patient with primary hyperaldosteronism.
A 50-year-old male patient observed a lump in his neck for one year, which has progressively enlarged. He experienced hoarseness for one month ago.
A 50-year-old male discovered a mass on the left side of his neck one year ago. Initially, the mass was approximately 3 cm, but it gradually grew to approximately 6.5 cm in the past month and caused hoarseness.
The patient has a 5-year history of hypertension with hypokalemia controlled with oral antihypertensive medications (nifedipine and spironolactone). His blood pressure has been maintained between 165-185/112-132 mmHg, and he often reports dizziness.
There is no family history of note.
On physical examination, a firm, non-tender mass approximately 6.5 cm in diameter was palpated along the lateral border of the left sternocleidomastoid muscle. The mass was irregular in shape, immobile, and did not move with swallowing.
The patient has a history of hypertension and developed severe hypokalemia (2.43 mmol/L) and hypertension upon admission, with blood pressure fluctuating between 174-205/97-135 mmHg. Potassium supplementation was administered, but serum potassium levels remained between 2.43-2.78 mmol/L without any clinical symptoms of hypokalemia. Preoperative multidisciplinary consultation discussed the surgical plan. Due to multiple abnormal hypertension markers, including aldosterone (upright) at 1308.2 pg/mL, aldosterone (supine) at 998.0 pg/mL, angiotensin II (supine) at 127.9 pg/mL, ACTH (8 hours) at 51.9 pg/mL, and adrenal computed tomography (CT) revealing a right adrenal tumor, the patient was diagnosed with primary hyperaldosteronism.
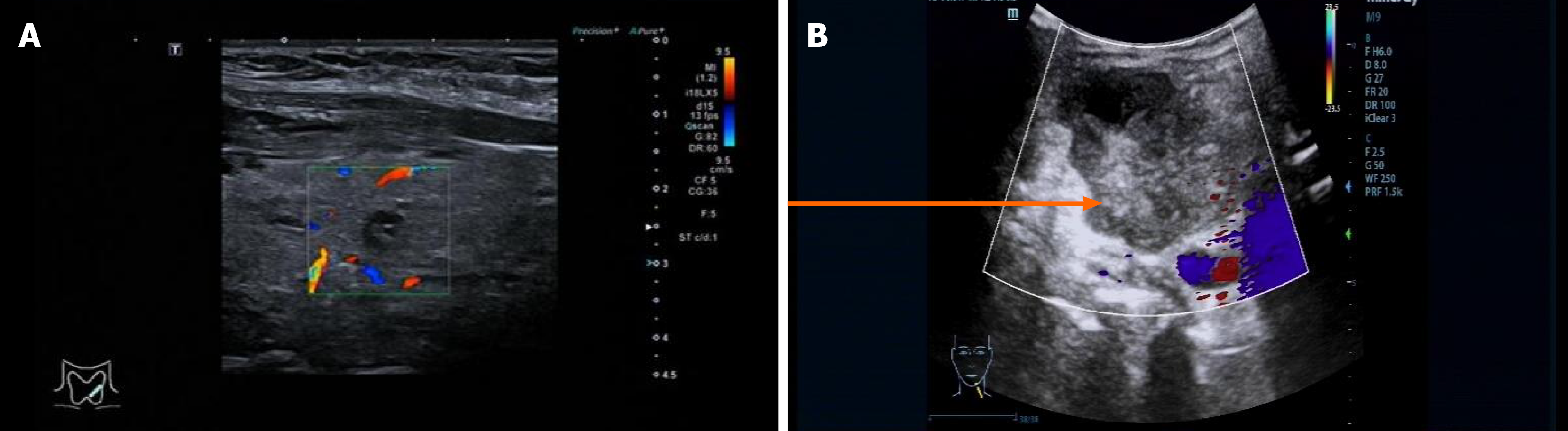
Thyroid ultrasound: A hypoechoic nodule with unclear margins and an irregular shape was observed on the deep surface of the right thyroid lobe. The nodule showed punctate echogenic foci with a longitudinal-to-transverse ratio > 1. Several mixed echogenic nodules were identified in the right lobe, the largest measuring approximately 0.6 cm × 0.4 cm × 0.3 cm, with clear borders and a regular shape. A mixed echogenic nodule was also found in the left lobe, measuring approximately 0.7 cm × 0.6 cm × 0.5 cm, with clear borders and a regular shape. A mixed echogenic mass measuring approximately 6.4 cm × 4.5 cm × 5.3 cm was found in the left neck, with clear borders and regular shape. Color Doppler flow imaging revealed blood flow signals within the mass. The mass was located anterior to the left common carotid artery and posterior to the internal jugular vein, with compression of the jugular vein and almost no visible lumen (Figure 1). There was blood flow stagnation in the upper portion of the mass, with spontaneous imaging visible.
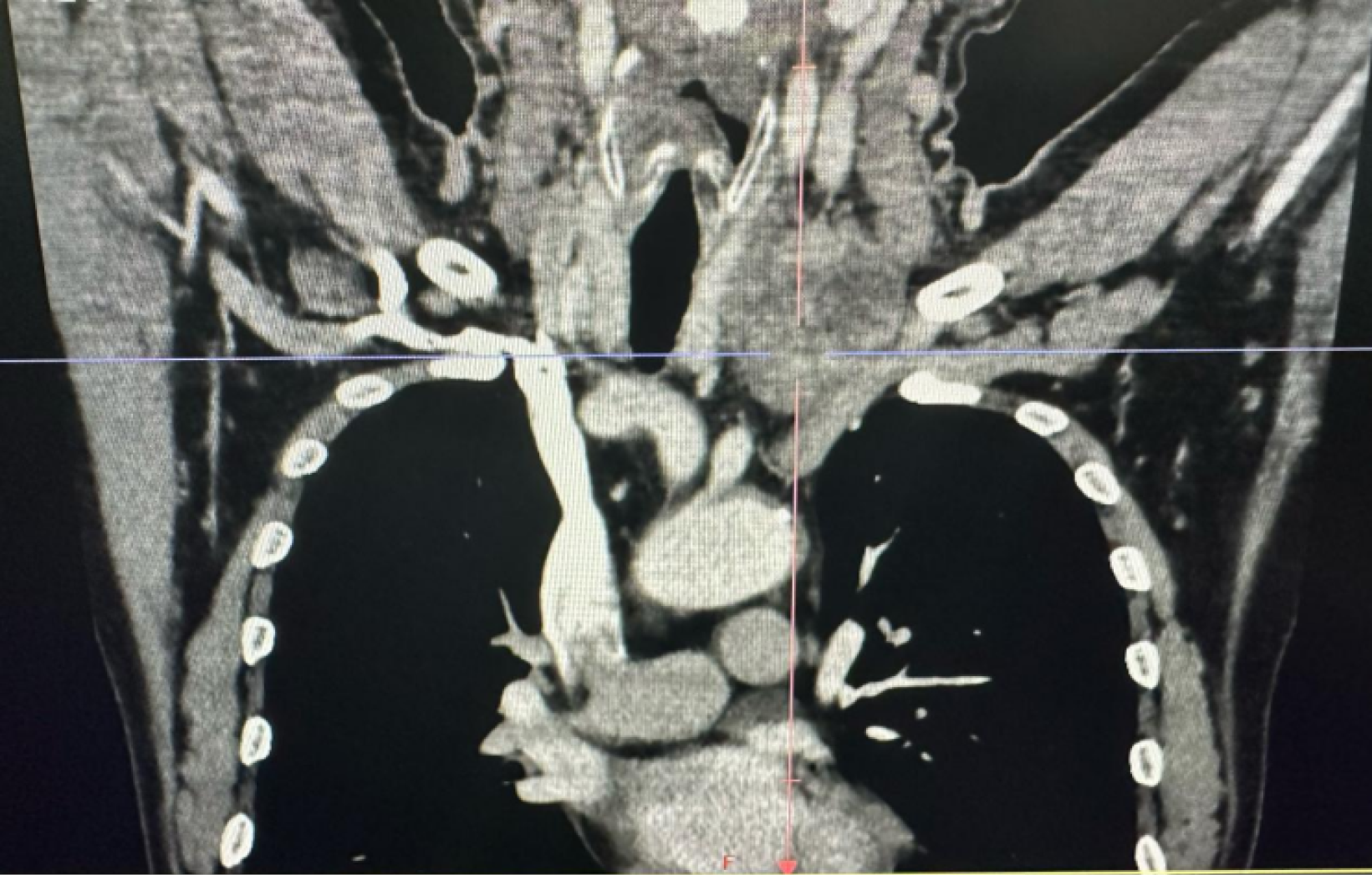
Neck and chest CT scan with contrast: A slightly low-density mass was observed adjacent to the left thyroid lobe, with an unclear boundary between the mass and the upper portion of the thyroid. The largest section measured approximately 4.0 cm × 5.5 cm. On the contrast-enhanced scan, the mass exhibited uneven enhancement (Figure 2).
The lesion extended into the lower chest cavity, with the left common carotid artery lying deep into the mass. The mass was closely adherent to the left common carotid artery, and the boundary between the mass and the left internal jugular vein was unclear. The left internal jugular vein was almost invisible due to compression, and collateral venous circulation was visible around the mass. The neighboring trachea showed slight compression but no significant narrowing.
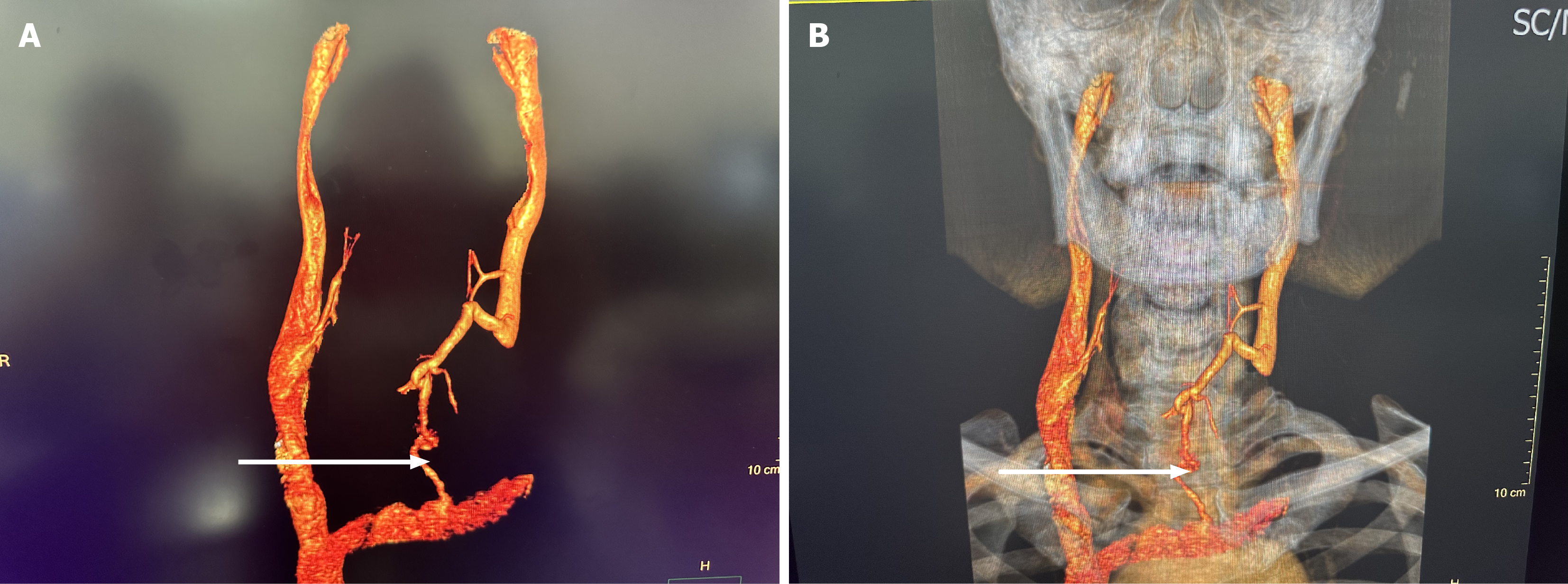
CT angiography/CT venography of head and neck vasculature: The lower portion of the left internal jugular vein was encased by the thyroid mass, with unclear visibility and local truncation. Collateral circulation was observed around the mass. The right internal jugular vein showed no abnormalities (Figure 3). A fiberoptic laryngoscopy revealed left vocal cord immobility, left vocal cord edema, and congestion with poor vocal cord closure.
PTC, primary hyperaldosteronism, hypokalemia, adrenal tumor.
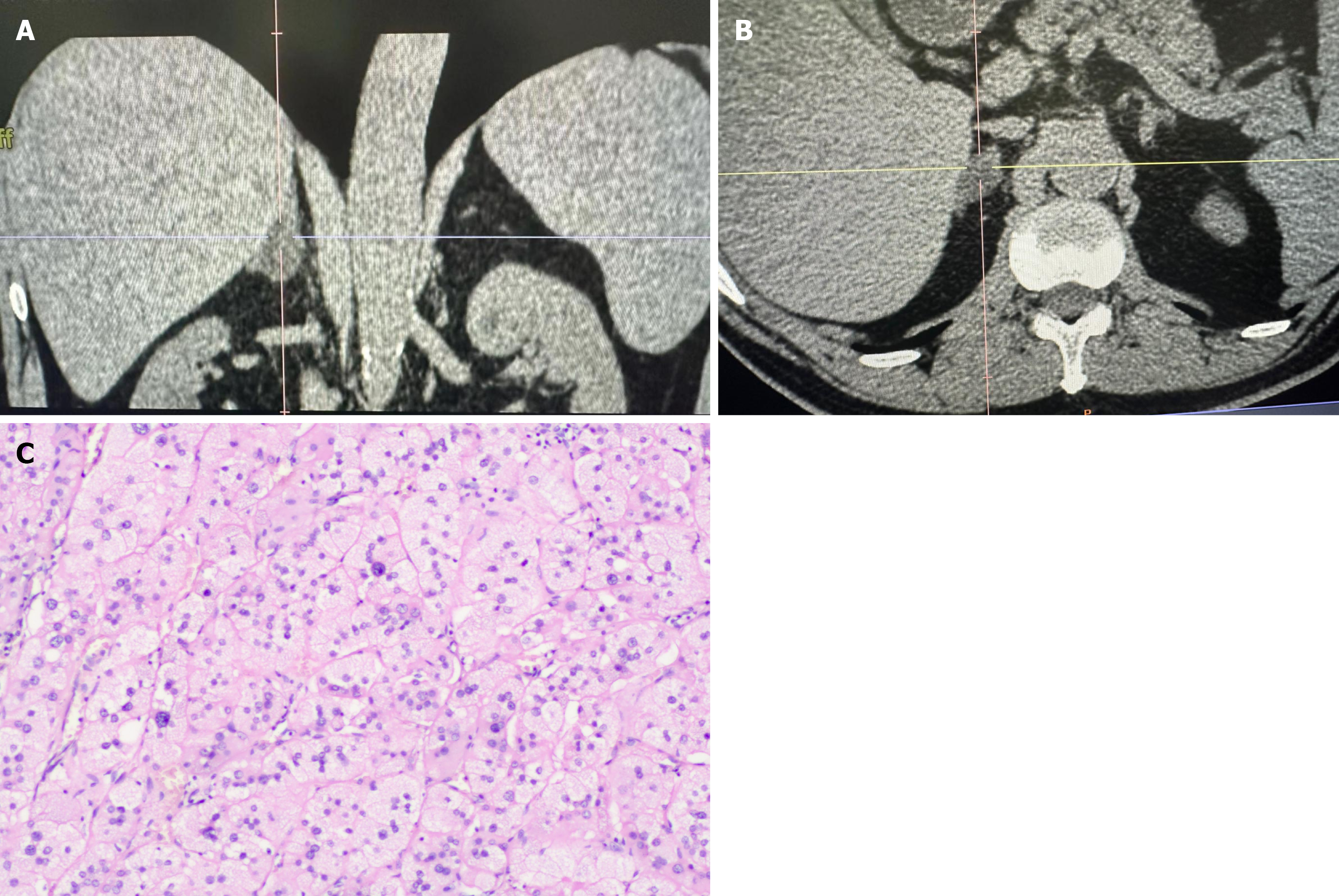
Given the concern for vascular invasion in the patient’s neck, the surgery may require vascular anastomosis or repair. Due to the high risk of malignant hypertension and potential vascular rupture postoperatively, we initially performed a laparoscopic right adrenal tumor resection in collaboration with the urology department. The adrenal pathology report indicated a benign adrenal cortical tumor. The procedure restored the patient’s blood pressure and hypokalemia to normal levels. Two weeks following adrenal surgery, the patient was readmitted for further treatment (Figure 4).
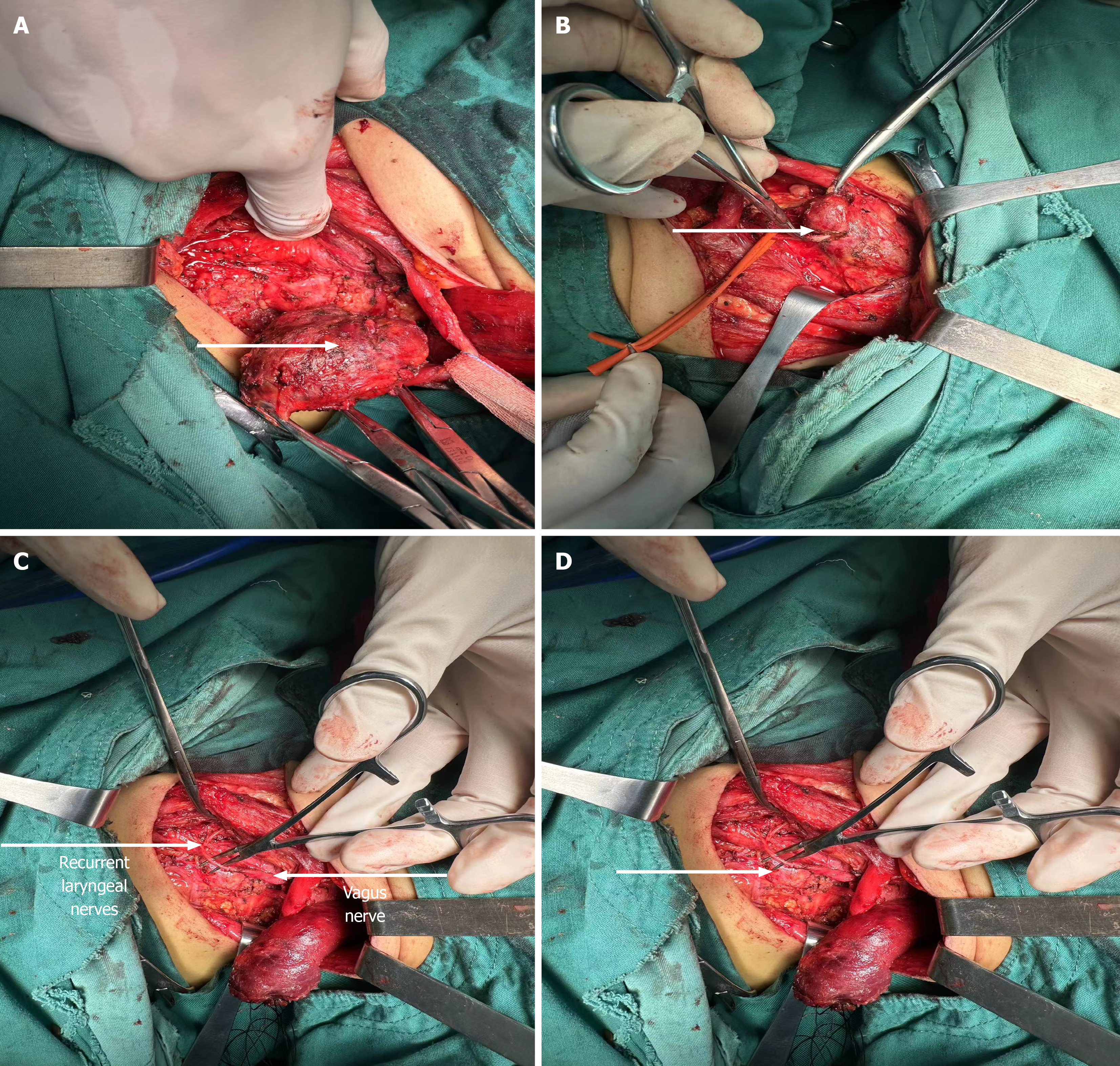
Under general anesthesia with endotracheal intubation, we performed a total thyroidectomy, bilateral central lymph node dissection, left neck tumor resection, left neck lateral lymph node dissection, left recurrent laryngeal nerve (RLN) to vagus nerve end-to-end anastomosis, left internal jugular vein resection and ligation, intraoperative frozen section, and left lower parathyroid auto-transplantation. Intraoperative frozen section results confirmed the diagnosis of right thyroid papillary carcinoma. No tumor was found in the left thyroid, and the left neck tumor was suspected to be PTC (pending immunohistochemical confirmation).
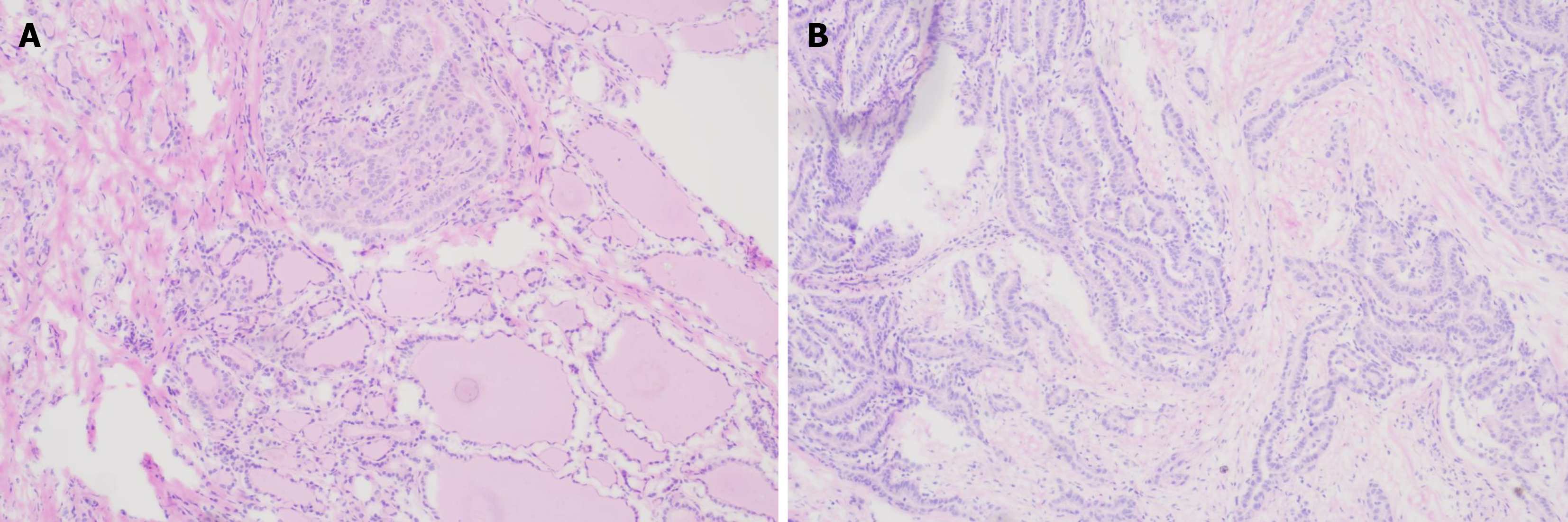
The right thyroid showed a PTC (follicular subtype) with a single focus. The tumor measured 0.8 cm × 0.6 cm × 0.6 cm, with capsule invasion, but no nerve or vascular invasion was observed. The remaining thyroid tissue showed no significant pathological changes. Immunohistochemistry results were CK19 (+), CD56 (-), and TPO (-). In the left thyroid, follicular nodular changes were noted. No cancer metastasis was detected in any of the 26 Lymph nodes examined (Figure 5).
Specifically, the left side lymph nodes in groups II (0/10), III (0/6), IV (0/5), central group (0/4), and group Vb (0/1) showed no signs of malignancy. The right central group lymph nodes contained only minimal fibrofatty tissue. The left neck mass was diagnosed as PTC (classic type), with a single focus and a tumor size of 6 cm × 5 cm × 4 cm. The tumor showed necrosis that invaded the capsule, with evidence of nerve invasion. Immunohistochemistry results were TTF-1 (+), Tg (+), CK19 (+), MC (+), Galectin-3 (+), CyclinD1 (+), Ki67 (+, approximately 8%), CD31 (vascular +), and D2-40 (lymphatic +) (Figure 6).
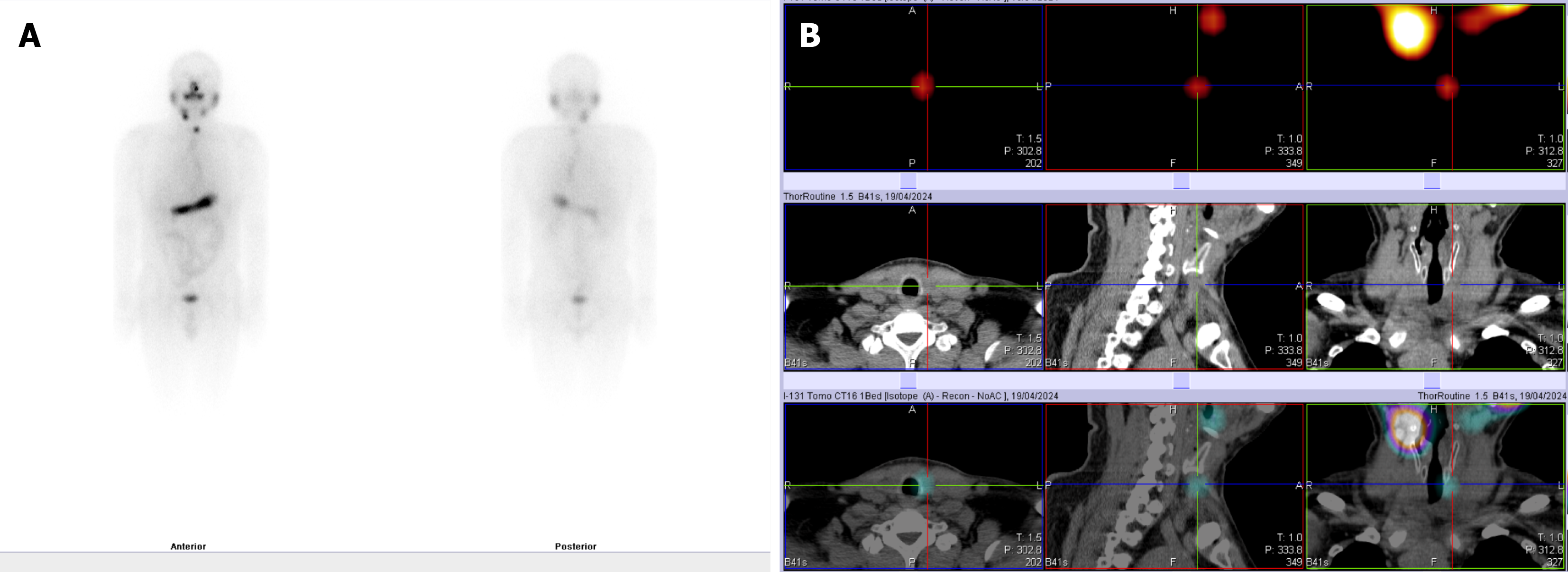
Postoperatively, the patient’s heart rate and blood pressure remained stable, and there were no significant abnormalities in diet or gastrointestinal function. He patient experienced transient hypoparathyroidism, which was treated with calcium supplements for five days. Subsequent parathyroid hormone and serum calcium levels returned to normal. The patient received radioactive iodine (I-131) treatment and TSH suppression therapy postoperatively (Figure 7).
After I-131 therapy, follow-up tests showed thyroid globulin (TG1) at 4.31 ng/mL and TSH at 0.29 mIU/L.Regular outpatient follow-up was conducted at 3 months, 6 months, and 1 year postoperatively. Fiberoptic laryngoscopy indicated persistent left vocal cord paralysis. However, the patient’s voice quality (timbre) and pitch significantly improved compared to their preoperative state.
PTC commonly causes hoarseness when invading the RLN[1]. In this case, preoperative laryngoscopy revealed that the left vocal cord was fixed and paralyzed. During surgery, however, we observed that the left RLN was intact, and the hoarseness was caused by an invasion of the left vagus nerve. Wang and Yang[2] reported a poorly differentiated carcinoma invading the vagus nerve causing hoarseness; however, the authors did not report the treatment process. It is extremely rare for differentiated thyroid carcinoma to invade the vagus nerve and cause hoarseness. Kumar et al[3] reported a case of diffuse large B-cell lymphoma compressing the vagus nerve; the patient did not receive further treatment. An irreparable nerve may lead to lifelong hoarseness and affect other systems. In this case, we considered that the patient had a long-standing unilateral vagus nerve involvement, and other organ functions had adapted, with no obvious symptoms other than hoarseness. During the surgery, we used nerve monitoring equipment to stimulate the left recurrent laryngeal and vagus nerves. Following stimulation, the signals were lost, indicating severe damage to the left vagus-RLN pathway, making it impossible to perform vagus nerve resection and end-to-end anastomosis. Therefore, we performed an end-to-end anastomosis between the left RLN and left vagus nerve. This surgical approach is exploratory, with unconfirmed clinical efficacy. Saxe et al[4] emphasized the importance of intraoperative nerve monitoring (IONM) during thyroid and parathyroid surgery. IONM is indispensable for major thyroid procedures, as routinely employed in our department. During surgery, IONM significantly reduces the risk of injury to the RLN, superior laryngeal nerve, and vagus nerve, thereby minimizing postoperative vocal alterations caused by neural impairment. Furthermore, it substantially lowers the incidence of bilateral RLN injury, a critical complication that may lead to life-threatening respiratory distress. Vagus nerve involvement in PTC impairments (due to direct compression/infiltration) laryngeal dysfunction (most common and significant): Unilateral vocal fold paralysis: Hoarseness, weak phonation, ineffective cough (impaired sputum expulsion), significantly increased aspiration risk (due to laryngeal sensory deficit + glottic insufficiency). Bilateral vocal fold paralysis (rare but critical): Can lead to acute airway obstruction, requiring emergency tracheostomy. Long-term Consequences: Chronic voice impairment, recurrent lower respiratory tract infections (aspiration pneumonia), severe decline in quality of life.
Peng et al[5] investigated 42 patients with RLN infiltration, dividing them into three groups. Group A included six patients with medullary thyroid cancer who underwent RLN resection and cricothyroid cartilage resection. Group B consisted of 29 patients with differentiated thyroid cancer (DTC) who underwent RLN resection and anastomosis with the cervical loop ansa cervicalis nerve (ACN) to the RLN. Group C included seven patients with RLN preservation. In cases of DTC with RLN involvement, R0 resection followed by nerve anastomosis resulted in satisfactory phonation recovery (Table 1)[6]. ACN-RLN anastomosis is one of the most commonly used surgical methods for nerve reinnervation, suggesting that nerve anastomosis plays a role in restoring nerve function. Simó et al[7] think that: Current evidence is low-level; however, it suggests that when the RLN has been severed, avulsed, or sacrificed during thyroid surgery it should be repaired intraoperatively. The immediate repair has on balance more advantages than disadvantages and should be considered whenever possible. This should enable the maintenance of vocal cord tone, better and prompter voice recovery and avoidance of aspiration.
| Group A (medullary thyroid cancer) | Group B (differentiated thyroid cancer) | Group C (differentiated thyroid cancer) | |
| Surgical approach | RLN resection and arytenoidectomy | RLN resection and ansa cervicalis nerve-to-RLN anastomosis | RLN preservation |
| Voice outcome | Poor voice quality | Satisfactory voice function | Good voice quality |
Preoperative imaging modalities, including ultrasound, CT, and CT angiography (CTA)/CT venography (CTV), provided our team with comprehensive vascular invasion assessment, enabling meticulous preoperative planning. This evaluation allowed anticipation of potential vascular reconstruction requirements, even accounting for scenarios where vascular repair might prove technically unachievable. Concurrently, preoperative assessment indicated the common carotid artery was relatively intact, with full preservation anticipated; otherwise, artificial arterial anastomosis would be necessary. Corresponding contingency plans and preoperative consultations were established accordingly. Dikici et al[8] thinks that invasion of IJV (internal jugular vein) with hypervascular tumor thrombosis is an extremely rare condition in PTC. Thrombosis of IJV is probably underdiagnosed. Early-stage diagnosis is important for long-term survival rates.
While our institutional experience includes occasional RLN end-to-end anastomosis during prior procedures, the intraoperative discovery of vagus nerve involvement represented an unprecedented challenge. Leveraging prior neurorrhaphy expertise, we performed an emergency vagal-RLN anastomosis to address this unexpected finding.
Bakkar et al[9] think that immediate reconstruction of an intraoperatively detected RLN injury has been strongly recommended by the 2020 American Association of Endocrine Surgeons guidelines. After neurorrhaphy, RLN regeneration occurs but in a random, misdirected fashion resulting in simultaneous contraction of abductors and adductors. Therefore, normal vocal fold function/mobility is typically not restored. The objective of this technical note is to describe a novel immediate RLN repair technique that has a strong propensity to regenerate and reinnervate laryngeal muscles and potentially restore laryngeal mobility.
In this case, the pathological report of the left thyroid showed no malignant tumor components, while the right thyroid papillary carcinoma had a diameter of < 1 cm. No cancer metastasis was observed in the right central group lymph nodes, and only minimal metastasis was detected in the left cervical lymph nodes.
There was a solitary tumor in the left cervical vascular sheath. We suspect three possibilities: First, an ectopic primary thyroid tumor accompanied by metastasis in the contralateral thyroid gland; second, a "skip" metastasis of the right thyroid malignant tumor to the left cervical vascular sheath. Yuan et al[10] and others reported two rare cases of PTC with lymph node metastasis to the non-ipsilateral sternocleidomastoid muscle and the intercostal muscles. Ding et al[11] reported a case of papillary thyroid microcarcinoma with contralateral lymph node "skip" metastasis, along with breast cancer. Yoon et al[12] reported that “Skip metastasis in patients with PTMC was associated with upper lobe tumor location”. Third, the simultaneous occurrence of two lesions of PTC, where one lesion is not located within the thyroid gland; this simultaneous occurrence is extremely rare.
Attard et al[13] Think that The PTC patients with a tumor size ≤ 1.0 cm, located in the upper pole, without a well-defined margin and extrathyroidal extension should be carefully evaluated for skip metastasis. Ding et al[11] think that a final selection of 13 articles published in English language from 1997 to 2017 was performed. Any research article, review or meta-analysis was taken into consideration. Research was expanded considering the related references of articles. The incidence of skip metastases ranged from 1.6 to 21.8%. Risk factors such as age > 45 years, size < 5 mm and tumor located in the upper pole or isthmus of thyroid gland were found. Due to the frequency of skip metastases in thyroid cancer, a careful preoperative examination of lateral lymph nodes should be necessary. These studies share significant parallels with our current case. In this patient, the thyroid tumor was located at the upper-middle pole of the thyroid gland, measuring less than 1 cm in diameter. Notably, early skip metastasis was observed despite the tumor's small size.
Based on the current situation, we consider "skip" metastasis to be the more likely explanation. During surgery, after performing end-to-end anastomosis of the vagus and RLNs, the patient reported a significant reduction in hoarseness three days postoperatively. We conducted a follow-up fiber-optic laryngoscopy at one and two months postoperatively, and the left vocal cord remained fixed.
This patient also had a primary aldosteronism with a unilateral adrenal tumor. Based on a previous recommendation, we performed a retroperitoneal laparoscopic adrenal tumor resection before thyroid surgery, which promptly normalized various biochemical indicators and controlled blood pressure, thereby reducing the risk of complications following thyroid surgery.
With suspected internal jugular vein involvement, Kobayashi et al[14] have recommended thyroid and vascular ultrasonography as the first choice for assessment, while Dikici et al[9] suggested further examinations with CT, magnetic resonance imaging (MRI), CTA, or CTV for more detailed evaluation. After these tests, Xiong et al[15] stated that the gold standard for tumor characterization remains fine needle aspiration biopsy. If the fine needle aspiration yields unsatisfactory results, immunohistochemistry should be conducted, and if necessary, a second fine needle aspiration or core needle biopsy should be performed[16].
Whether a correlation exists between PTC and primary aldosteronism is a point of concern in this case and there may be relevant correlations with the following aspects: (1) Mutual influence of the endocrine system: The thyroid and adrenal glands are both important components of the endocrine system that exhibit certain interactions in hormone regulation and metabolic processes; (2) Genetic factors: Certain genetic syndromes may simultaneously increase the risk of thyroid and adrenal diseases; (3) Immune system abnormalities: Autoimmune diseases may simultaneously affect the thyroid and adrenal glands; (4) Environmental factors: Environmental factors such as radiation exposure, chemicals, and lifestyle may simultaneously affect the functions of the thyroid and adrenal glands; (5) Metabolic syndrome: Metabolic syndrome describes a group of metabolic disorders including hypertension, hyperglycemia, obesity, and dyslipidemia; and (6) Hormone interactions: Thyroid hormones and aldosterone have different physiological functions in the body, but they may interact in some metabolic processes.
Although these interactions do not directly cause PTC or primary aldosteronism, they may have implications for metabolism and fluid balance. These correlations require further clinical research and case analyses.
The major thyroid surgery was scheduled one month after the initial adrenalectomy, following rigorous assessment of the patient's recovery trajectory. This decision was made after confirming normalization of key physiological and psychological parameters, including: Fluid-electrolyte balance restoration, Hemodynamic stability (blood pressure within reference range), adequate psychological resilience for surgical endurance.
Thorough preoperative preparation is critical for optimizing surgical outcomes. Prior to major thyroid resection, our multidisciplinary team implemented the following standardized protocols: Preoperative optimization; corrected fluid-electrolyte disturbances and identified primary pathological drivers through comprehensive laboratory evaluation.
Conducted meticulous preoperative assessments including: Thyroid function evaluation (TSH, free T4, thyroglobulin levels); cardiopulmonary function testing (echocardiography, pulmonary function tests); Laryngeal examination with preoperative vocal cord mobility assessment via flexible laryngoscopy; Contrast-enhanced CT angiography with 3D vascular reconstruction for anatomical localization; Postoperative Rehabilitation Program.
Initiated early vocal rehabilitation within 24 hours postoperatively under rehabilitation medicine supervision, incorporating: Progressive voice simulation training with biofeedback, structured phonation exercises targeting pitch, loudness, and resonance. Regular stroboscopic laryngeal assessments at 1/3/6-month intervals.
Implemented cervical rehabilitation protocol featuring: Isometric neck exercises (Day 14 post-op); Progressive range-of-motion training (starting Week 2); Scar massage techniques (after suture removal); Maintained ongoing functional assessment throughout the 12-month postoperative period, with dynamic adjustment of rehabilitation intensity based on recovery milestones.
The postoperative survival rate for PTC patients is generally good. If clinical symptoms suggest vascular or nerve involvement, imaging examinations such as ultrasonography, CT, or MRI should be immediately performed. In cases suggesting PTC with RLN involvement, fiberoptic laryngoscopy should be conducted to assess vocal cord status and intraoperative nerve monitoring is strongly recommended. Simultaneous invasion of the blood vessels and vagus nerve in PTC is rare and associated with severe complications. Preoperative evaluation of large cervical vessel involvement is essential. Surgeons should examine signs of large vein damage, as vascular resection and repair or reconstruction are often required. Prior to major thyroid surgery or any other organ surgery, in cases complicated by primary aldos
| 1. | Chen JM, Fang JG, Zhong Q, Hou LZ, Ma HZ, Feng L, He SZ, Shi Q, Lian M, Wang R, Shen XX. [Clinical characteristics and prognosis in papillary thyroid carcinoma patients with recurrent laryngeal nerve invasion]. Zhonghua Yi Xue Za Zhi. 2022;102:3868-3874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Wang YT, Yang YJ. [Multimodal ultrasound diagnosis of thyroid low differentiated squamous cell carcinoma invading the vagus nerve: Case report]. Zhongguo Yixue Yingxiang Jishu. 2022;38:955-956. [DOI] [Full Text] |
| 3. | Kumar K, Ahmed R, Bajantri B, Singh A, Abbas H, Dejesus E, Khan RR, Niazi M, Chilimuri S. Tumors Presenting as Multiple Cranial Nerve Palsies. Case Rep Neurol. 2017;9:54-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Saxe A, Idris M, Gemechu J. Does the Use of Intraoperative Neuromonitoring during Thyroid and Parathyroid Surgery Reduce the Incidence of Recurrent Laryngeal Nerve Injuries? A Systematic Review and Meta-Analysis. Diagnostics (Basel). 2024;14:860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 5. | Peng J, Zhu G, Gao Y, Song X, Yu H, Huang R, Chen M, Jiang Y, Sun G, Li M, Zheng H, Wang W. New strategy for intraoperative phonosurgical management of recurrent laryngeal nerve infiltrated by thyroid carcinoma. Langenbecks Arch Surg. 2024;409:138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Wang W, Chen D, Chen S, Li D, Li M, Xia S, Zheng H. Laryngeal reinnervation using ansa cervicalis for thyroid surgery-related unilateral vocal fold paralysis: a long-term outcome analysis of 237 cases. PLoS One. 2011;6:e19128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 7. | Simó R, Nixon IJ, Rovira A, Vander Poorten V, Sanabria A, Zafereo M, Hartl DM, Kowalski LP, Randolph GW, Kamani D, Shaha AR, Shah J, Marie JP, Rinaldo A, Ferlito A. Immediate Intraoperative Repair of the Recurrent Laryngeal Nerve in Thyroid Surgery. Laryngoscope. 2021;131:1429-1435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Dikici AS, Yıldırım O, Er ME, Kılıç F, Tutar O, Kantarcı F, Mihmanlı I. A Rare Complication of the Thyroid Malignancies: Jugular Vein Invasion. Pol J Radiol. 2015;80:360-363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Bakkar S, Chorti A, Papavramidis T. Immediate repair of the recurrent laryngeal nerve during thyroid surgery via a tension-free end-to-side anastomosis with the Vagus. Updates Surg. 2025;77:363-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Yuan M, Zhao Y, Fu Q, Wang Y, Fu Y. Papillary thyroid carcinoma with rare lymph node metastasis between the non-ipsilateral sternocleidomastoid and striate muscles: two case reports and literature review. Gland Surg. 2022;11:2003-2012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Ding M, Kong YH, Gu JH, Xie RL, Fei J. Papillary thyroid microcarcinoma with contralateral lymphatic skip metastasis and breast cancer: A case report. World J Clin Cases. 2022;10:3609-3614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 12. | Yoon JH, Park JY, Hong AR, Kim HK, Kang HC. Predictors of lateral lymph node metastasis and skip metastasis in patients with papillary thyroid microcarcinoma. Front Endocrinol (Lausanne). 2024;15:1392247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 13. | Attard A, Paladino NC, Lo Monte AI, Falco N, Melfa G, Rotolo G, Rizzuto S, Gulotta E, Salamone G, Bonventre S, Scerrino G, Cocorullo G. Skip metastases to lateral cervical lymph nodes in differentiated thyroid cancer: a systematic review. BMC Surg. 2019;18:112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Kobayashi K, Hirokawa M, Yabuta T, Fukushima M, Kihara M, Higashiyama T, Tomoda C, Takamura Y, Ito Y, Miya A, Amino N, Miyauchi A. Tumor thrombus of thyroid malignancies in veins: importance of detection by ultrasonography. Thyroid. 2011;21:527-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Xiong XJ, Xiao MM, Zhang YX, Liu DG, Jin ML, Wang J, Xu HT, Li QC, Wu GP. The Accurate Interpretation and Clinical Significance of Morphological Features of Fine Needle Aspiration Cells in Papillary Thyroid Carcinoma. Anal Cell Pathol (Amst). 2023;2023:9397755. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 16. | Hahn SY, Shin JH, Han BK, Ko EY, Ko ES. Ultrasonography-guided core needle biopsy for the thyroid nodule: does the procedure hold any benefit for the diagnosis when fine-needle aspiration cytology analysis shows inconclusive results? Br J Radiol. 2013;86:20130007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/