Published online Sep 26, 2025. doi: 10.12998/wjcc.v13.i27.107158
Revised: May 21, 2025
Accepted: June 20, 2025
Published online: September 26, 2025
Processing time: 137 Days and 5 Hours
Primary signet ring cell carcinoma of the urethra in women is an exceedingly rare malignancy. It was first reported in postmenopausal women in 1987, and only five patients have been reported to date.
A 61-year-old woman presented with irregular vaginal bleeding, and subsequent evaluation identified a tumor located in the distal urethra. Upon diagnosis of primary urethral carcinoma, she underwent a distal urethrectomy. Histopathological analysis demonstrated that the tumor consisted of a combination of intestinal adenocarcinoma and signet ring cell carcinoma. At the 12-month postoperative follow-up, there was no evidence of disease recurrence.
This case report highlights the exceptional rarity of female urethral signet ring cell carcinoma, emphasizing the importance of early clinical detection and the necessity for precise and conservative surgical intervention.
Core Tip: Primary signet ring cell carcinoma of the urethra in women is an exceedingly rare malignancy. A 61-year-old woman presented with irregular vaginal bleeding. She was found to have a tumor located in the distal urethra. Based upon a diagnosis of primary urethral carcinoma, she underwent distal urethrectomy. Microscopically, the tumor was composed of intestinal adenocarcinoma and signet ring cell carcinoma. No recurrence was observed 12 months after surgery.
- Citation: Xu P, Ling SS, Hu E, Yi BX. Primary signet ring cell carcinoma of the female urethra: A case report. World J Clin Cases 2025; 13(27): 107158
- URL: https://www.wjgnet.com/2307-8960/full/v13/i27/107158.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i27.107158
Urothelial carcinoma represents the predominant form of urethral cancer, with squamous cell carcinoma being the second most frequent form. Of all urethral cancer cases, 16.4% are classified as adenocarcinoma[1]. The primary urethral cancer exhibits an incidence rate of 4.3 per million among men, in contrast to 1.5 per million among women in the United States, highlighting a pronounced predilection for older males[2,3]. Primary signet ring cell carcinoma of the urethra in women is an exceedingly rare malignancy[4]. It was first reported in postmenopausal women in 1987, and only five patients have been reported to date[5,6]. Signet ring cell carcinoma was named due to its signet ring-like appearance.
A 61-year-old multiparous female had a vaginal mass detected 2 years previously, and had recently developed irregular vaginal bleeding for 2 months.
The patient was admitted to the hospital on January 31, 2024, and reported no associated symptoms of urinary frequency, urgency, or stranguria.
Ten years ago, the patient underwent a Manchester operation (including partial cervical resection, anterior and posterior vaginal wall repair, and cardinal ligament shortening) at a local hospital due to pelvic organ prolapse. The patient had no prior history of malignancies, hypertension, or diabetes.
The patient was a multiparous woman with a history of two full-term deliveries and one abortion. She experienced menopause at the age of 55 years. Her father had a history of hypertension, while her two sisters and one brother were in good health.
Gynecological examination identified a 2 cm mass situated at the urethral orifice, exhibiting a medium texture and the absence of surface bleeding (Figure 1). No masses or abnormal bleeding were detected in the cervix or vagina. No enlarged lymph nodes were palpable in the inguinal region.
Tumor marker levels were within the normal range, including carbohydrate antigen 125, carbohydrate antigen 153, carbohydrate antigen 19-9, α-fetoprotein, and carcinoembryonic antigen.
Pelvic enhanced computed tomography (CT) was conducted to assess the pelvic and abdominal cavities, and showed no evidence of lymph node metastasis. In addition, cystoscopy findings were unremarkable. There were no abnormalities on gastrointestinal endoscopy, breast color Doppler ultrasound and lung CT examination.
The patient underwent a distal urethral resection after multidisciplinary diagnosis and treatment planning. The patient did not receiveundergo adjuvant radiotherapy or chemotherapy according to the European Association of Urology Guidelines on Primary Urethral Carcinoma-2020 Update.
The patient declined genetic testing due to financial constraints.
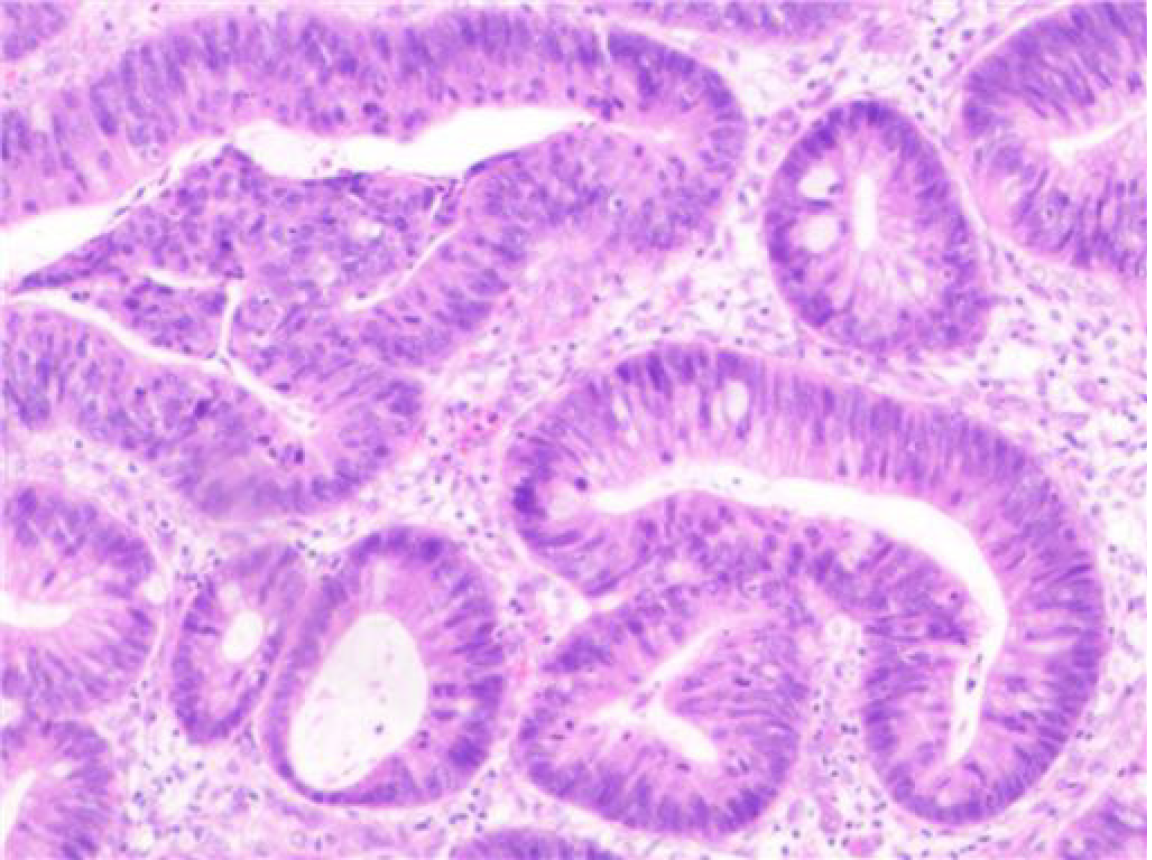
Final pathological examination confirmed the presence of intestinal adenocarcinoma and signet ring cell carcinoma, measuring 2.0 cm in size, located in the urethra, with negative surgical margins. No cancer accumulation was found in the external urethral tissue (Figure 2).
Primary signet ring cell carcinoma of the female urethra T1N0M0.
The patient underwent a distal urethral resection after multidisciplinary diagnosis and treatment planning. The patient did not receive adjuvant radiotherapy or chemotherapy.
At the 12-month follow-up, no evidence of recurrence was observed, and lifelong follow-up is recommended for potential disease progression.
Primary urethral malignant tumors are rare, with a higher incidence in males compared to females. Risk factors include long-term urethral catheterization, chronic urinary tract infections, urethral strictures, sexually transmitted diseases, and a history of radiotherapy. In women, it may be associated with recurrent lower urinary tract infections or urethral diverticulum[7]. In female patients, tumors were located in the proximal urethra in 28.9% of cases, the distal urethra in 68.9%, and both proximal and distal urethra in 2.2%[2]. The 5-year overall survival rate for primary urethral malignant tumors is 61%. Among the histological subtypes, squamous cell carcinoma has a relatively better prognosis, with a 5-year overall survival rate of 64%, while adenocarcinoma has the poorest prognosis, with a 5-year overall survival rate of only 31%[8]. Studies suggest that female patients often have a worse prognosis compared to male patients at the time of diagnosis[3].
The most common histological types are squamous cell carcinoma and transitional cell carcinoma, while adenocarcinoma represents 16.4% of cases[1]. Histologically, adenocarcinoma is subdivided into intestinal, mucinous, clear cell, and signet ring cell types. Consequently, primary signet ring cell carcinoma of the female urethra is exceedingly rare[9]. Our case represents the sixth reported instance of female urethral signet ring cell adenocarcinoma in the English literature. As previously mentioned, the patient had no urinary system-related risk factors but had a history of pelvic organ prolapse and underwent surgical treatment for the condition.
The common symptoms of urethral malignant tumors include dysuria (48%), hematuria (62%), perineal mass (52%), urinary urgency (20%), pelvic pain (33%), and fistula (10%) among others[7]. The patient initially presented with no obvious urinary symptoms but was treated for irregular vaginal bleeding, which was likely related to the tumor's location. This incidental finding allowed for early detection and prompt treatment of the condition[8]. The patient could have received earlier treatment, as she had noticed the mass two years previously but only sought medical attention after developing symptoms of vaginal bleeding.
Signet ring cell carcinoma was named due to its signet ring-like appearance. This unique adenocarcinoma variant is defined by cells with abundant cytoplasmic mucin, which pushes the nucleus to the cell periphery. According to the 2010 World Health Organization classification, signet ring cell carcinoma is not classified as an independent histological subtype but is included within the poorly cohesive carcinoma category[10]. Signet ring cell adenocarcinoma is most frequently found in the gastrointestinal tract, followed by the breast and lung. Its occurrence in the urethra is exceedingly rare. Therefore, when diagnosing primary signet ring cell adenocarcinoma of the urethra, it is essential to perform upper and lower gastrointestinal endoscopy, breast examination, and lung CT imaging to rule out primary tumors in these organs. The diagnosis of primary urethral malignancy typically requires endoscopic evaluation and biopsy for definitive confirmation[7]. Magnetic resonance imaging is the preferred imaging modality for local and locoregional evaluation of confirmed or suspected tumors[7].
Endoscopic transurethral resection is not recommended for distal tumors due to its low local control rate, with recurrence rates as high as 50% within 17 months[7,11]. For stage T2 tumors of the distal urethra, distal urethral resection can be considered as a conservative treatment option if surgical margins are negative[12]. Studies report a 5-year recurrence-free survival rate of 65% and a 5-year disease-specific survival rate of 82% for this approach[7,13]. For malignant tumors of the posterior urethra in women, conservative surgery is not recommended, and radical cystectomy should be the preferred approach[7,12].
Cisplatin-based neoadjuvant chemotherapy is recommended prior to radical surgery for the management of proximal T2N0 urethral cancer. Multidisciplinary diagnosis and treatment are essential for all patients presenting with locally advanced disease (T3N0-2M0). In male patients with locally advanced squamous cell carcinoma, a regimen of radical radiotherapy augmented with radiosensitizing chemotherapy is advocated to achieve curative intent while preserving genital integrity. For patients experiencing local urethral recurrence, options such as salvage surgery or radiotherapy may be considered. In cases of distant metastatic disease, systemic therapy tailored to the specific characteristics of the tumor should be assessed and implemented as appropriate[12].
Compared with other reports, this case is the youngest and has the earliest stage. We expect her to have a better prognosis (Table 1).
| No. | Age (years) | Symptoms | Symptom duration | Location and extent of tumors at presentation | Stage (TNM) | Treatment | Follow up | Status |
| Suzuki et al[6] | 70 | Frequency, difficulty in urination, nocturia and acute retention | 6 weeks | Urethral mass fixed to the symphysis pubis, vagina and bladder neck with left inguinal lymph node metastasis | T4N1 or 2 M0 | Radiotherapy. Anterior exenteration and left inguinal lymph node dissection. Palliative chemotherapy | 18 months | DOD |
| Suzuki et al[6] | 66 | Frequency and bloody vaginal discharge | 9 months | Entire urethra, anterior vaginal wall, pelvic side walls and bladder neck with right inguinal lymph node metastasis | T3N1 or 2 M0 | No treatment | 6 months | Presumably DOD |
| Suzuki et al[6] | 72 | Enlarging mass at the external urethral meatus and yellowish discharge | 4-6 months | Polypoid tumor at the external urethral meatus | TaN0M0 | Wide local excision (2 cm of distal urethra, urethral meatus and anterior vulva) and bilateral inguinal lymph node dissection | 7 months | NED |
| Suzuki et al[6] | 69 | Difficulty in urination and bloody fluid from urethra | 24 months | Anterior vaginal wall and bladder neck | T3N0M0 | Total cysto-urethrectomy and hysterectomy with bloody fluid pelvic lymph node dissection | 17 months | NED |
| Grimsby et al[5] | 81 | Suprapubic pain, urethral discharge, urinary frequency, urgency, and stranguria | No report | A firm tender mass at 7 o’clock in the urethra | T4N0M0 | Robotic assisted radical cystectomy, bilateral pelvic lymph node dissection | 1 month | DOD |
| 6 (present case) | 61 | Irregular vaginal bleeding | 2 months | 2 cm mass situated at the urethral orifice | T1N0M0 | Distal urethral resection | 12 months | NED |
This case highlights the exceptional rarity of female urethral signet ring cell carcinoma, emphasizing the importance of early clinical detection and the necessity for precise, conservative surgical intervention. Irregular vaginal bleeding in females should not be exclusively attributed to gynecological conditions, as it may also signal the presence of a urinary tract neoplasm, necessitating a comprehensive multidisciplinary assessment for accurate diagnosis. Given the exceedingly low incidence of female urethral signet ring cell carcinoma, it is imperative to amass and analyze data from multiple centers to advance our understanding and management of this condition.
The authors are grateful to the staff of the Pathology Department of Jinhua People’s Hospital, Zhejiang Province, China.
| 1. | Swartz MA, Porter MP, Lin DW, Weiss NS. Incidence of primary urethral carcinoma in the United States. Urology. 2006;68:1164-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 164] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 2. | Gakis G, Morgan TM, Efstathiou JA, Keegan KA, Mischinger J, Todenhoefer T, Schubert T, Zaid HB, Hrbacek J, Ali-El-Dein B, Clayman RH, Galland S, Olugbade K Jr, Rink M, Fritsche HM, Burger M, Chang SS, Babjuk M, Thalmann GN, Stenzl A, Daneshmand S. Prognostic factors and outcomes in primary urethral cancer: results from the international collaboration on primary urethral carcinoma. World J Urol. 2016;34:97-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Sui W, RoyChoudhury A, Wenske S, Decastro GJ, McKiernan JM, Anderson CB. Outcomes and Prognostic Factors of Primary Urethral Cancer. Urology. 2017;100:180-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 4. | Aron M, Park S, Lowenthal BM, Gupta S, Sahoo D, Cheville JC, Hansel DE. Primary Female Urethral Carcinoma: Proposed Staging Modifications Based on Assessment of Female Urethral Histology and Analysis of a Large Series of Female Urethral Carcinomas. Am J Surg Pathol. 2020;44:1591-1601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Grimsby G, Wolter C. Signet ring adenocarcinoma of a urethral diverticulum. J Surg Case Rep. 2011;2011:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Suzuki K, Morita T, Tokue A. Primary signet ring cell carcinoma of female urethra. Int J Urol. 2001;8:509-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Neuville P, Murez T, Savoie PH, Rocher L, Fléchon A, Ferretti L, Van Hove A, Branger N, Camparo P, Rouprêt M. Primary urethral carcinoma: Recommendations of the oncology committee of the French Urology Association. Fr J Urol. 2024;34:102606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Derksen JW, Visser O, de la Rivière GB, Meuleman EJ, Heldeweg EA, Lagerveld BW. Primary urethral carcinoma in females: an epidemiologic study on demographical factors, histological types, tumour stage and survival. World J Urol. 2013;31:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Joseph DDC, Chinnathambi J, Jamburaj A. Primary signet ring cell carcinoma of the male urethra. Ecancermedicalscience. 2022;16:1426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Arai T. Where does signet-ring cell carcinoma come from and where does it go? Gastric Cancer. 2019;22:651-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Dalbagni G, Zhang ZF, Lacombe L, Herr HW. Female urethral carcinoma: an analysis of treatment outcome and a plea for a standardized management strategy. Br J Urol. 1998;82:835-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 61] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Gakis G, Bruins HM, Cathomas R, Compérat EM, Cowan NC, van der Heijden AG, Hernández V, Linares Espinós EE, Lorch A, Neuzillet Y, Ribal MJ, Rouanne M, Thalmann GN, Veskimäe E, Witjes AJ. European Association of Urology Guidelines on Primary Urethral Carcinoma-2020 Update. Eur Urol Oncol. 2020;3:424-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Dimarco DS, Dimarco CS, Zincke H, Webb MJ, Bass SE, Slezak JM, Lightner DJ. Surgical treatment for local control of female urethral carcinoma. Urol Oncol. 2004;22:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/