Published online Mar 6, 2024. doi: 10.12998/wjcc.v12.i7.1333
Peer-review started: November 12, 2023
First decision: January 9, 2024
Revised: January 17, 2024
Accepted: February 6, 2024
Article in press: February 6, 2024
Published online: March 6, 2024
Processing time: 109 Days and 23.7 Hours
Multiple primary malignant tumors (MPMTs) are rare type of cancer, especially when solid tumors are the first and lymphoma is the second primary malignancy. We report a patient with heterochronous MPMTs consisting of prostate cancer and rectal diffuse large B-cell lymphoma (DLBCL).
We report a 77-year-old male patient diagnosed with prostate cancer who was treated with radiation therapy and one year of endocrine therapy with bicaluta
Although rare, the possibility of prostate cancer combined with a double primary cancer of DLBCL can provide a deeper understanding.
Core Tip: We report the case of a 77-year-old male patient diagnosed with prostate cancer presenting with dysuria with hematuria. He received radiation therapy and 1 year of endocrine therapy with an efficacy evaluation of partial response. 7 years later, he was diagnosed with diffuse large B-cell lymphoma of the rectum with lung metastases presenting with lower abdominal pain and constipation, and was treated with 2 cycles of chemotherapy on the CHOP regimen with an efficacy evaluation of remission. He was not treated again for personal reasons and unfortunately, the patient died 1 year later.
- Citation: Liang JL, Bu YQ, Peng LL, Zhang HZ. Heterochronous multiple primary prostate cancer and lymphoma: A case report. World J Clin Cases 2024; 12(7): 1333-1338
- URL: https://www.wjgnet.com/2307-8960/full/v12/i7/1333.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i7.1333
Multiple primary malignant tumors (MPMTs) are defined as two or more histologically distinct malignancies in one individual[1]. According to the time interval of diagnosis, it is divided into simultaneous and heterochronic MPMTs. Simultaneous MPMTs are diagnosed within 6 months of the primary cancer, and heterochronous MPMTs are defined as the detection of another malignancy more than 6 months after the diagnosis of the first one[2].
Symptoms of heterochronic MPMTs are similar to those of a single malignant tumor, but the prognosis is worse. MPMTs are diagnosed based on pathological, histological, and immunohistochemical examinations, and there are no standardized treatment guidelines. Treatment plan is mainly based on the patient's pathological staging, clinical staging, and tolerance. Finally, a radical or palliative treatment plan will be chosen. Treatment methods include surgery and systemic therapy, including chemotherapy, endocrine therapy, immunotherapy, targeted therapy, and so on. Adverse drug reactions, overlap between the effects of drugs, and the accumulation of drug toxicity should be considered.
Here, we report a 77-year-old male patient diagnosed with prostate cancer who was treated with radiation therapy and one year of endocrine therapy. Seven years later, rectal diffuse large B-cell lymphoma (DLBCL) with lung metastases was detected.
A 77-year-old man who was treated in another hospital due to dysuria, hematuria, and bloating was transferred to Hebei General Hospital as his symptoms did not improve despite treatment.
Two weeks before admission, the patient developed intermittent dysuria and hematuria. For six months, he had abdominal distension and constipation without significant weight loss, fever, and night sweats. Due to persistent symptoms, the patient was referred to our hospital for further treatment.
He had a history of prostate cancer diagnosed 7 years before his visit. Pathology of puncture biopsy confirmed vesicular adenocarcinoma with a Gleason score of 8. Immunohistochemical staining showed the following results: Prostate-specific antigen (PSA) (++++), P504s (++), 34βE12 (-), P63 (-), androgen receptor (++++), and Ki-67 positive rate of about 5%. Radiotherapy combined with endocrine therapy was given. Gross tumor volume (GTV): Visible tumor in the prostate, CTV: Pelvic lymphatic drainage area. Prescribed dose: 100 % GTV: 6400 cGy, 98% CTV: 5800 cGy. Endocrine therapy regimen included bicalutamide (50 mg per day) and goserelin extended-release implant (1/28 d). Efficacy was assessed as a partial response at the end of radiotherapy. Endocrine therapy was performed for 1 year. Then, it was discontinued for personal reasons. There was no specific family history.
Physical examination on admission showed coarse breath sounds, rales, scattered dry rales at the base of both lungs and pressure pain in the right epigastric region without rebound and muscle tension. In anal palpation, we also found pressure pain in the front of the anus and irregular swelling with brittle texture. The finger sleeve was stained with blood.
After admission, serum total protein was 66.2 g/L (normal range: 65-85 g/L) and serum albumin was 38.3 g/L (normal range: 40-55 g/L). Total PSA was 0.835 ng/mL (normal range: < 4.4 ng/mL). Lactate dehydrogenase was 426.2 (normal range: 109-245 U/L). Coagulation was normal except for mildly elevated D-dimer level (0.94 mg/L, normal range < 0.55 mg/L). Urine analysis showed 3+ occult blood. Screening for human immunodeficiency virus, syphilis, and hepatitis B were negative.
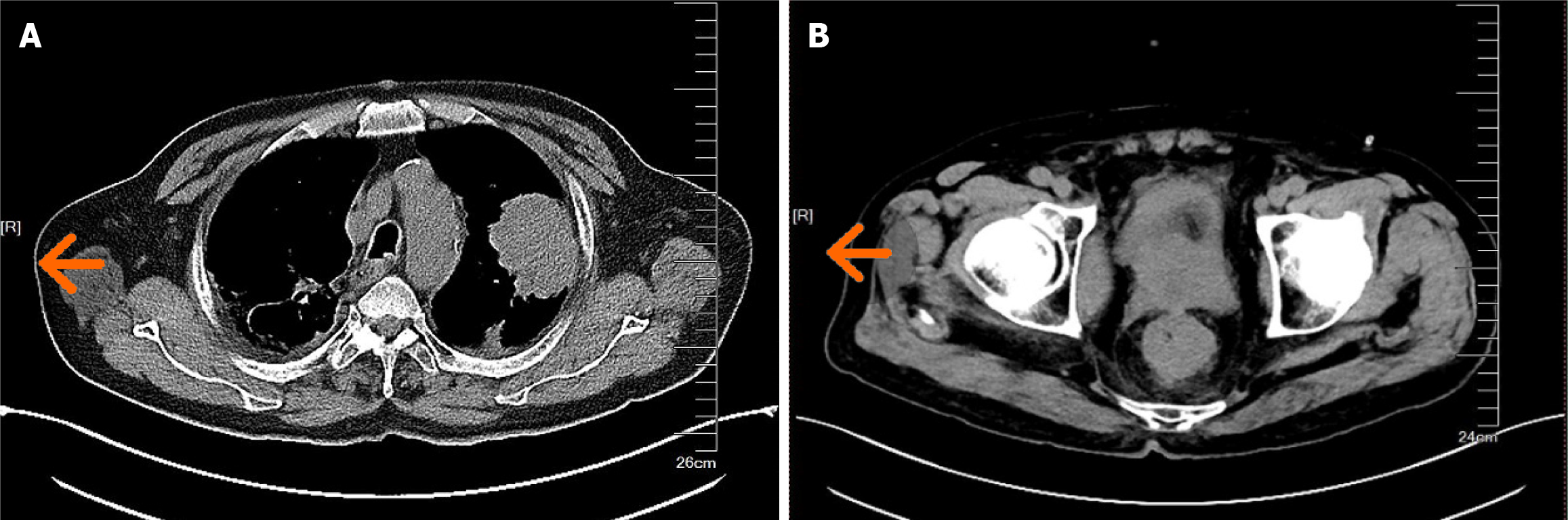
Computed tomography (CT) scan showed marked thickening of the rectal wall and a space-occupying lesion in the apical posterior segment of the upper lobe of the left lung (Figure 1). Colonoscopy showed narrowing of the rectal lumen from the dentate line to 5 cm above the dentate line, with congestive and swollen infiltrative changes in the mucosa, irregular surface structure, and brittle texture.
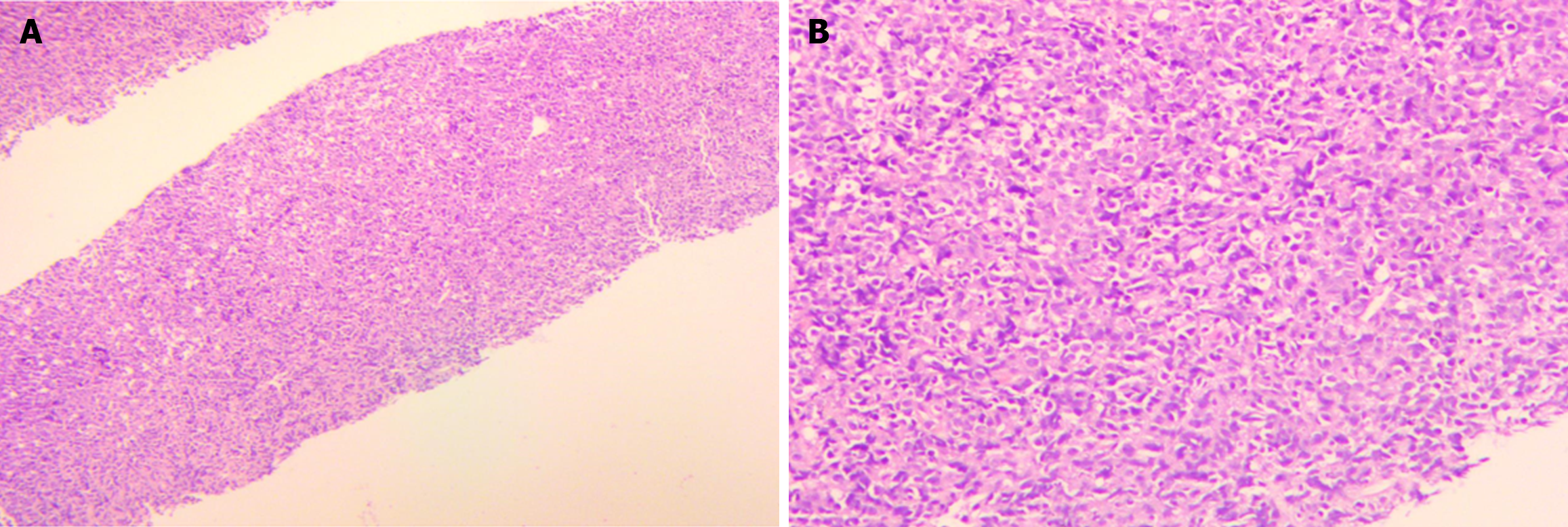
Pathological assessment of rectal biopsy revealed extruded damaged heterogeneous cells in the mucosal mesenchyme. Immunohistochemical staining revealed CD3 (-), CD20 (+), CD21 (-), CD (10-), Bcl-2 (+), Bcl-6 (+), MUM1 (+), c-MYC (20%+), CD5 (-), Cyclin D1 (-), EBNA2 (-), P504s (-), PSA (-), CKpan (-), vimentin (-), CgA (-), CD56 (-), Syn (-), and Ki-67 (90%+) (Figure 2). Miscellaneous in situ component (rectal biopsy) showed EBER (-). Combined with immunohistochemical staining, the diagnosis was confirmed to be diffuse large B-cell lymphoma. CT-guided puncture biopsy of the left lung mass suggested Non-Hodgkin's lymphoma (NHL). Immunohistochemical staining of the lung tissue revealed CD3 (-), CD20 (+), CD21 (-), Bcl-2 (+), Bcl-6 (+), CD10 (-), MUM1 (+), c-MYC (40%+), and Ki-67 (approximately 90%+) (Figure 3). Combined with immunohistochemical staining, the diagnosis was confirmed to be DLBCL.
All three tumors had consistent pathological and immunohistochemical findings. The rectal and pulmonary tumors were not considered to be metastases of prostate cancer. Thus, the diagnosis of MPMTs of prostate cancer and rectal DLBCL with lung metastases was confirmed.
After 2 cycles of chemotherapy with the CHOP regimen, a partial response was obtained (Figure 4).
Subsequently, the patient discontinued treatment due to personal reasons. Unfortunately, the patient died after 1 year.
Prostate cancer is a malignancy of men and significantly increases mortality rates globally. In 2020, GLOBOCAN reported approximately 1.41 million new cases of prostate cancer, resulting in nearly 380000 deaths worldwide, with higher prevalence in developed countries[3]. Late diagnosis of prostate cancer and treatment failure are the main factors leading to the increased mortality rate of prostate cancer[4]. Genetic susceptibility, ethnicity, age, obesity, and other environmental factors are risk factors for prostate cancer. Prostate cancer is diagnosed based on digital rectal examination, prostate-specific antigen analysis, and prostate biopsies.
NHL is a hematologic malignancy originating from lymphoid tissue. The pathogenesis of NHL is unclear and may be related to hepatitis B, human immunodeficiency virus, EBV infection, elevated lactate dehydrogenase, or weak immune response[5]. DLBCL is the most common subtype of NHL, accounting for nearly 30% of cases[6]. Gene expression profiling (GEP) can differentiate between favorable germinal center B-cell (GCB), unfavorable activated B-cell (ABC), and intermediate unclassifiable signatures in DLBCL[7]. Because GEP is not routinely available in clinical practice, immunohistochemical signatures were developed to capture the distinction between the GCB-like DLBCL subgroup and the ABC-like DLBCL subgroup[8]. In 2005, Hans et al[9] applied tissue microarray technology for typing, and established the typing pattern of IHC by detecting CD10, BCL6, and d MUM1. It classified DLBCL into GCB type and non-GCB type. The prognosis of the former was significantly better than that of the latter (P < 0.001). There was 84% consistency between this typing method and the gold standard. This case belonged to the non-GCB type, with a relatively poor prognosis. The international prognostic index of the patient was 5, indicating a high risk and poor prognosis.
MPMTs are rare type of cancer, and despite the increasing incidence, it is rare to have a solid tumor as the first malignancy and lymphoma as the second primary malignancy. In addition to the rarity of prostate cancer combined with DLBCL, it is also rare for a second primary malignancy to develop after radiotherapy for prostate cancer.
In general, cancer survival is increasing by 3%-5% annually. Therefore, MPMTs are becoming increasingly important for cancer diagnosis as survival rates improve[10]. The increase in the incidence of MPMTs can be attributed to the increased number of cancer survivors, the long-term side effects of chemotherapy and radiotherapy, and the role of genetic, environmental, and endocrine factors[11]. The results of a meta-analysis showed that patients with prostate cancer treated with radiotherapy have an increased risk (OR) of developing rectal cancer compared with patients treated with non-radiotherapy measures (OR: 1.45, 95%CI: 1.07-1.97, P = 0.02)[12]. This suggests that radiation therapy may increase the risk of a second primary malignancy. In this case report, a patient with prostate cancer developed rectal DLBCL with lung metastases after radiation therapy and endocrine therapy. The patient had no risk factors, such as genetic and environmental risk factors, and it was hypothesized that radiation therapy and endocrine therapy might have increased the risk of MPMTs.
Although rare, the possibility of prostate cancer combined with a double primary cancer of DLBCL can provide a deeper understanding.
| 1. | Zhai C, Cai Y, Lou F, Liu Z, Xie J, Zhou X, Wang Z, Fang Y, Pan H, Han W. Multiple Primary Malignant Tumors - A Clinical Analysis of 15,321 Patients with Malignancies at a Single Center in China. J Cancer. 2018;9:2795-2801. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 2. | Mukaiyama Y, Suzuki M, Morikawa T, Mori Y, Takeshima Y, Fujimura T, Fukuhara H, Nakagawa T, Nishimatsu H, Kume H, Homma Y. Multiple primary malignant neoplasms of the glottis, renal pelvis, urinary bladder, oral floor, prostate, and esophagus in a Japanese male patient: a case report. World J Surg Oncol. 2014;12:294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 68645] [Article Influence: 13729.0] [Reference Citation Analysis (201)] |
| 4. | Sekhoacha M, Riet K, Motloung P, Gumenku L, Adegoke A, Mashele S. Prostate Cancer Review: Genetics, Diagnosis, Treatment Options, and Alternative Approaches. Molecules. 2022;27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 226] [Cited by in RCA: 534] [Article Influence: 133.5] [Reference Citation Analysis (0)] |
| 5. | Wu J, Zhou Y, Li Q, Zhang J, Mao Y. Primary biliary non-Hodgkin's lymphoma: A case report. Medicine (Baltimore). 2021;100:e26110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Sehn LH, Salles G. Diffuse Large B-Cell Lymphoma. N Engl J Med. 2021;384:842-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 776] [Article Influence: 155.2] [Reference Citation Analysis (0)] |
| 7. | Rosenwald A, Wright G, Chan WC, Connors JM, Campo E, Fisher RI, Gascoyne RD, Muller-Hermelink HK, Smeland EB, Giltnane JM, Hurt EM, Zhao H, Averett L, Yang L, Wilson WH, Jaffe ES, Simon R, Klausner RD, Powell J, Duffey PL, Longo DL, Greiner TC, Weisenburger DD, Sanger WG, Dave BJ, Lynch JC, Vose J, Armitage JO, Montserrat E, López-Guillermo A, Grogan TM, Miller TP, LeBlanc M, Ott G, Kvaloy S, Delabie J, Holte H, Krajci P, Stokke T, Staudt LM; Lymphoma/Leukemia Molecular Profiling Project. The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med. 2002;346:1937-1947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2802] [Cited by in RCA: 2719] [Article Influence: 113.3] [Reference Citation Analysis (0)] |
| 8. | Carbone A, Gloghini A, Kwong YL, Younes A. Diffuse large B cell lymphoma: using pathologic and molecular biomarkers to define subgroups for novel therapy. Ann Hematol. 2014;93:1263-1277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, Müller-Hermelink HK, Campo E, Braziel RM, Jaffe ES, Pan Z, Farinha P, Smith LM, Falini B, Banham AH, Rosenwald A, Staudt LM, Connors JM, Armitage JO, Chan WC. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2826] [Cited by in RCA: 3236] [Article Influence: 140.7] [Reference Citation Analysis (2)] |
| 10. | Chowdhry AK, Fung C, Chowdhry VK, Bergsma D, Dhakal S, Constine LS, Milano MT. A population-based study of prognosis and survival in patients with second primary thyroid cancer after Hodgkin lymphoma. Leuk Lymphoma. 2018;59:1180-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 56678] [Article Influence: 7084.8] [Reference Citation Analysis (135)] |
| 12. | Nugent TS, Low EZ, Fahy MR, Donlon NE, McCormick PH, Mehigan BJ, Cunningham M, Gillham C, Kavanagh DO, Kelly ME, Larkin JO. Prostate radiotherapy and the risk of secondary rectal cancer-a meta-analysis. Int J Colorectal Dis. 2022;37:437-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Udo IA, Nigeria S-Editor: Liu JH L-Editor: A P-Editor: Zhao S