Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4434
Revised: May 5, 2024
Accepted: June 3, 2024
Published online: July 16, 2024
Processing time: 85 Days and 16.4 Hours
This case report highlights a rare instance of concurrent keloid and epidermal cyst development at an ear cartilage harvest site following rhinoplasty in a 25-year-old woman. Both conditions, which typically stem from skin trauma, seldom occur together, demonstrating the exceptional characteristics of this case.
The patient underwent successful surgical removal of both the keloid and the epidermal cyst. Postoperative treatment included the use of silicone sheets, gel, and oral tranilast to reduce scarring. No recurrence was observed over a 6-mo follow-up period, indicating effective management of the condition.
The effective management of complex skin trauma cases underscores the need for individualized treatment strategies in plastic surgery.
Core Tip: This case report documents a rare co-occurrence of a keloid and an epidermal cyst at the site of auricular cartilage harvest used in rhinoplasty, emphasizing the complex interplay of surgical trauma and genetic predisposition in scar formation. It highlights the challenges in managing such dual complications, illustrating the necessity for meticulous surgical removal and postoperative care strategies to minimize recurrence and optimize cosmetic outcomes. The case underscores the importance of considering potential adverse sequelae in surgical planning and patient counseling.
- Citation: Kim JM, Cheon JS, Choi WY. Ear keloid and epidermal cyst following auricular cartilage harvest for rhinoplasty: A case report. World J Clin Cases 2024; 12(20): 4434-4439
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4434.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4434
Keloids, which arise from surgical interventions or other trauma, are benign but persistent fibroproliferative scar lesions that seldom resolve without medical or surgical treatment. They extend beyond the boundaries of the original wound and tend to recur even after surgical removal[1,2]. Keloids often manifest as irregular, dark red lesions accompanied by itching or pain, causing significant cosmetic concerns when occurring on the face. Pierced ears are particularly considered a common precursor to keloid formation[3]. By contrast, epidermal cysts are intradermal or subcutaneous cystic lesions characterized by the presence of keratin and stratified epithelium[4,5]. These cysts frequently occur in individuals aged 20-29 years and vary in distribution based on body location, with the face being the most common site[6]. They often occur spontaneously but are especially common in the ear area after piercing or surgical intervention[3]. Although both keloids and epidermal cysts may develop after trauma, their coexistence is rarely reported[7]. This report presents a case of an ear keloid co-occurring with an epidermal cyst.
A 25-year-old woman presented with a chief complaint of significant alteration in the appearance of her left ear, characterized by keloid tissue formation at the site of a previous cartilage harvest for rhinoplasty. The patient reported considerable cosmetic concern and psychological distress due to the presence of the large keloid tissue.
Approximately 9 mo after undergoing rhinoplasty using ear cartilage, the patient noticed the development of a firm, palpable keloid tissue, which progressively worsened, prompting her to seek medical advice 1 year after surgery.
The patient denied having any relevant past illnesses that could directly contribute to the current condition; however, the surgical history of cartilage harvesting was noted.
The patient did not report any family history of keloids or other related dermatological conditions, suggesting that this occurrence might have been sporadic or primarily trauma-induced.
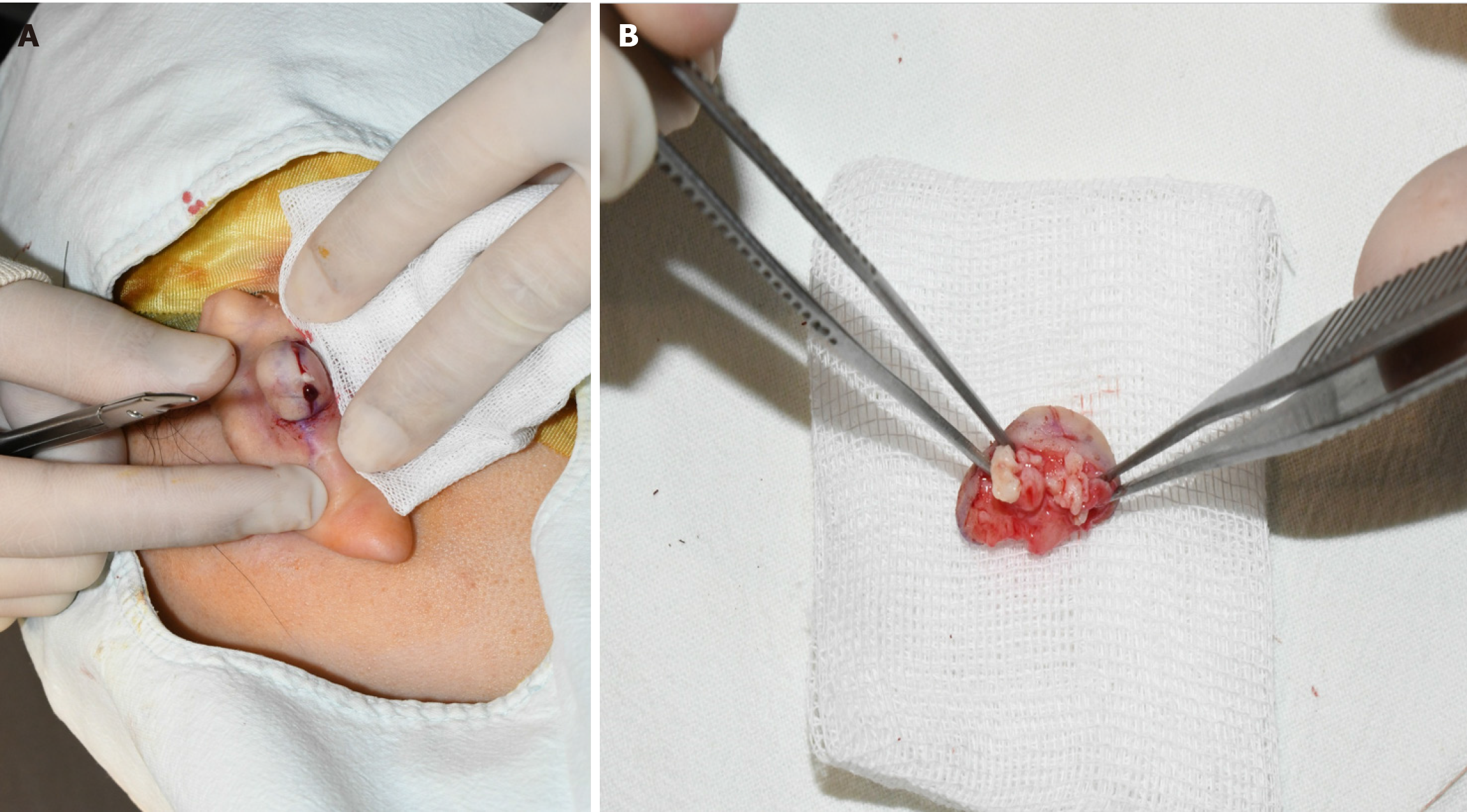
Physical examination revealed a firm, palpable scar tissue measuring 2 cm × 2 cm × 1.5 cm located posterior to the patient’s left ear, with no tenderness or paresthesia (Figure 1).
Keloid co-existing with an epidermal cyst.
Initially, the lesion was diagnosed as a typical keloid based on the clinical evaluation. However, during this process, we observed an epidermal cyst encapsulated within the keloid tissue, characterized by a dirty white, cheese-like substance (Figure 2). This finding led to a revised final diagnosis of a keloid coexisting with an epidermal cyst at the ear cartilage harvest site after rhinoplasty. Both the keloid and the cyst were carefully excised, and the area was covered using a fillet flap.
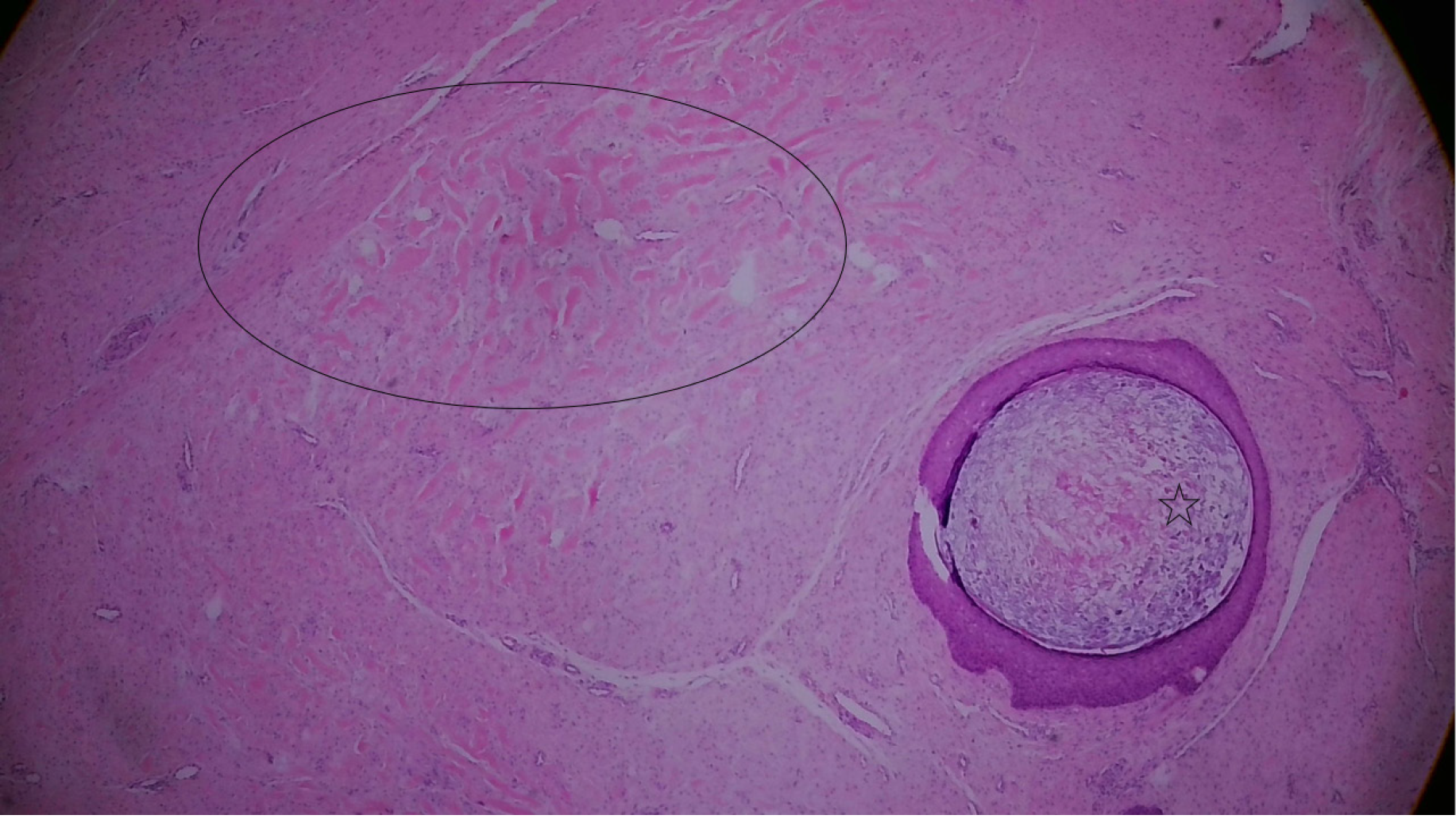
Histologic analysis of the excised tissue via hematoxylin and eosin staining revealed the presence of a cyst surrounded by stratified squamous epithelium containing thick collagen bundles and keratin, characteristic of the keloid tissue (Figure 3). These histologic findings confirmed the diagnosis of an epidermal cyst coexisting within the ear keloid. Postoperatively, a silicone sheet and gel were applied to the scar area, and the patient was prescribed oral tranilast 300 mg/d for 3 mo, to mitigate scar formation (Figure 4). During subsequent regular outpatient follow-ups, the patient reported no ear discomfort, and no recurrence was observed at the 6-mo follow-up.
Keloids and epidermal cysts are distinct pathological entities that may arise from skin trauma, with their coexistence within the same lesion being an exceptionally rare occurrence. This case illustrates the unique challenge presented by the simultaneous development of a keloid and an epidermal cyst, a phenomenon that, while uncommon, underscores the complexity of skin responses to injury. Epidermal cysts can originate either congenitally or as acquired lesions, often attributed to the implantation of epithelium following surgical procedures or other forms of skin trauma[4,5]. This implantation process is a significant etiological factor in cyst formation, highlighting the role of injury in triggering aberrant epithelial growth within the dermis[8]. Keloids, on the other hand, represent an overgrowth of scar tissue that extends beyond the boundaries of the original wound, with their formation influenced by genetic predisposition, the anatomical location of the wound, and the nature of the skin injury[2]. The pathophysiological mechanisms driving keloid formation are complex and not fully understood, although they are known to involve a dysregulated healing response characterized by excessive collagen deposition[1]. The simultaneous occurrence of keloids and epidermal cysts within scar tissue is rare, with both conditions potentially resulting from the grafting effects of traumatic injuries[1,2,5]. Park et al[9] highlighted the risk of keloid formation following auricular cartilage harvesting for rhinoplasty, suggesting that such surgical interventions can predispose individuals to both keloids and epidermal cysts. In the presented case, the chronological sequence of the keloid and epidermal cyst development was unclear, and the patient did not exhibit any specific symptoms apart from the presence of these conditions[7]. The role of ear cartilage grafting in rhinoplasty as a causative factor for their concurrent development is noteworthy, presenting a complex challenge for effective mana
In conclusion, the coexistence of epidermal cysts and keloids necessitates a treatment paradigm that prioritizes the thorough removal of the epidermal cyst to avert its recurrence. This targeted surgical strategy accentuates the primacy of cyst excision in addressing the complexities of such conditions, ensuring that the initial surgical endeavors are concentrated on reducing the recurrence risk and fostering optimal healing. This paradigm highlights the significance of bespoke, patient-centric treatment plans in plastic surgery, where the concurrent management of multiple conditions demands meticulous and strategic planning.
We extend our sincere gratitude to all individuals who contributed to the completion of this manuscript. We especially thank the patient who dedicated her time and effort to this research. We also express our gratitude to all healthcare professionals and researchers involved in the study. Additionally, we would like to thank everyone who assisted in the presentation and publication of this paper.
| 1. | Limandjaja GC, Niessen FB, Scheper RJ, Gibbs S. The Keloid Disorder: Heterogeneity, Histopathology, Mechanisms and Models. Front Cell Dev Biol. 2020;8:360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 169] [Cited by in RCA: 224] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 2. | Shaheen A. Comprehensive Review of Keloid Formation. CRDOA. 2017;4:1-18. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Hendricks WM. Complications of ear piercing: treatment and prevention. Cutis. 1991;48:386-394. [PubMed] |
| 4. | Nigam JS, Bharti JN, Nair V, Gargade CB, Deshpande AH, Dey B, Singh A. Epidermal Cysts: A Clinicopathological Analysis with Emphasis on Unusual Findings. Int J Trichology. 2017;9:108-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Handa U, Chhabra S, Mohan H. Epidermal inclusion cyst: cytomorphological features and differential diagnosis. Diagn Cytopathol. 2008;36:861-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Liu M, Liu X, Wang Y, Wang Z, Tuo H, Feng Y, Zheng Y. Epidermal Cyst on the Scalp Induced by Forceps Injury During Delivery: A Case Report and Epidemiological Analysis of 3949 Patients. Clin Cosmet Investig Dermatol. 2023;16:593-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 7. | Lee HW, Kim CG, Song JS, Koh IC, Kim H, Kim KN. Management of epidermal cysts arising from scar tissues: A retrospective clinical study. Medicine (Baltimore). 2018;97:e12188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Hoang VT, Trinh CT, Nguyen CH, Chansomphou V, Chansomphou V, Tran TTT. Overview of epidermoid cyst. Eur J Radiol Open. 2019;6:291-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 115] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 9. | Park TH, Park JH, Kim JK, Seo SW, Rah DK, Chang CH. Analysis of 15 cases of auricular keloids following conchal cartilage grafts in an asian population. Aesthetic Plast Surg. 2013;37:102-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Ekstein SF, Wyles SP, Moran SL, Meves A. Keloids: a review of therapeutic management. Int J Dermatol. 2021;60:661-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 157] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/