Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4391
Revised: May 10, 2024
Accepted: May 23, 2024
Published online: July 16, 2024
Processing time: 95 Days and 21 Hours
Meckel's diverticulum is a common congenital anomaly of the gastrointestinal tract, with a higher incidence rate in children under 7 years old. The condition is characteristically asymptomatic but may become a clinical concern when complications such as intestinal obstruction, bleeding, perforation, or diverticulitis precipitate acute abdominal presentations.
This report describes the case of a middle-aged man initially suspected of having acute appendicitis, which rapidly progressed to acute peritonitis with concomi
Meckel's diverticulum is a rare cause of small bowel obstruction in adults, and it should be considered in a differential diagnosis.
Core Tip: Meckel's diverticulum is occasionally encountered in clinical practice, but the formation of internal hernias in Meckel's diverticulum is extremely rare, requiring clinical doctors to be good at differential diagnosis and adopt correct treatment strategies.
- Citation: Zhang Q, Xu XJ, Ma J, Zhang YM. Misdiagnosed Meckel's diverticulum with internal hernia mimicking appendicitis: A case report. World J Clin Cases 2024; 12(20): 4391-4396
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4391.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4391
Meckel's diverticulum is a frequent congenital anomaly of the gastrointestinal tract. Owing to the absence of distinct clinical manifestations, preoperative diagnosis is difficult. Terminal ileal Meckel's diverticulum is particularly chal
The patient, a 37-year-old man, was admitted to the hospital with an abrupt onset of lower right abdominal pain that persisted for 2 h.
The medical history included sudden, continuous distension pain in the right lower abdomen after dinner, accompanied by nausea and cessation of gas passage through the anus, without vomiting or fever.
The patient had no history of hypertension, diabetes, inflammatory bowel disease, or abdominal surgeries.
The patient’s family history did not indicate any genetic or hereditary predispositions.
Physical examination revealed that the patient was in distress, with a flat abdomen and localized tenderness in the right lower quadrant. No rebound tenderness or peritoneal irritation signs were observed, with bowel sounds occurring at a frequency of five times per minute.
Laboratory findings revealed a white blood cell count of 11.39 × 109/L, with 82.4% neutrophils. Liver and kidney function tests and C-reactive protein levels fell within normal ranges.
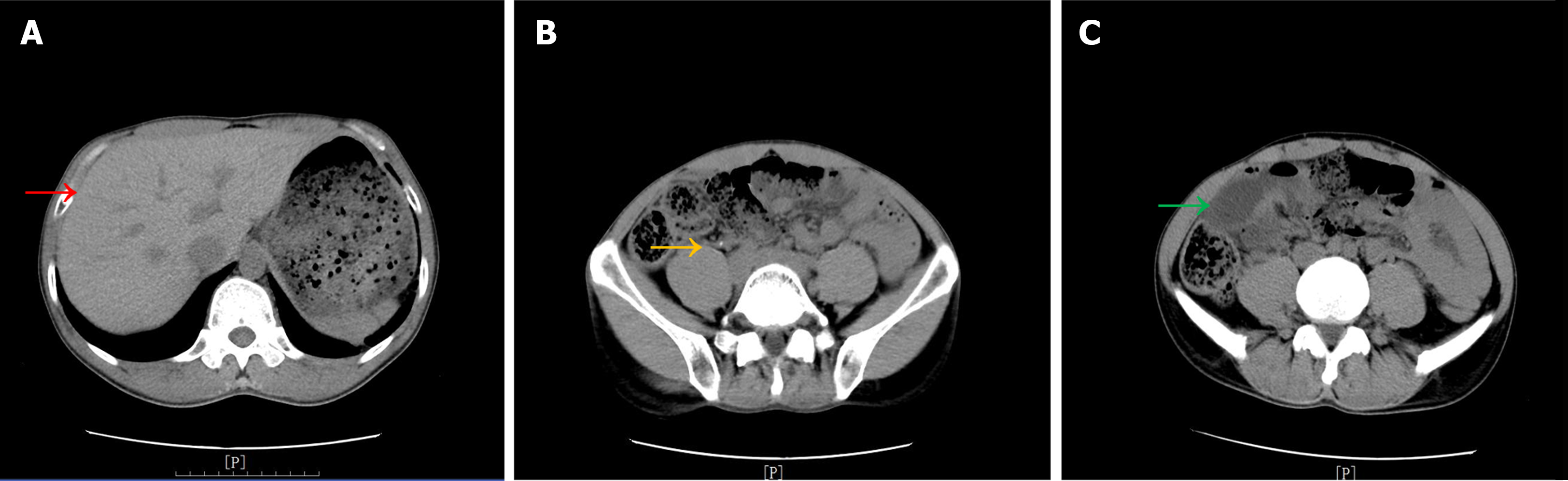
Abdominal computed tomography (CT) scans indicated the presence of an appendiceal fecalith with mild surrounding effusion, dilation of specific small intestine segments in the lower right abdomen with fluid accumulation, and effusion in the mesenteric area without fluid accumulation in the abdominal or pelvic cavity (Figure 1).
Initial evaluation, based on the patient's persistent right lower quadrant pain, elevated leukocyte and neutrophil counts, and radiologic evidence of an appendiceal fecalith and surrounding effusion, led to a provisional diagnosis of acute appendicitis. Due to inadequate fasting time, the patient received ceftriaxone (1.0 g) for infection and pain management, with continuous monitoring of abdominal signs.
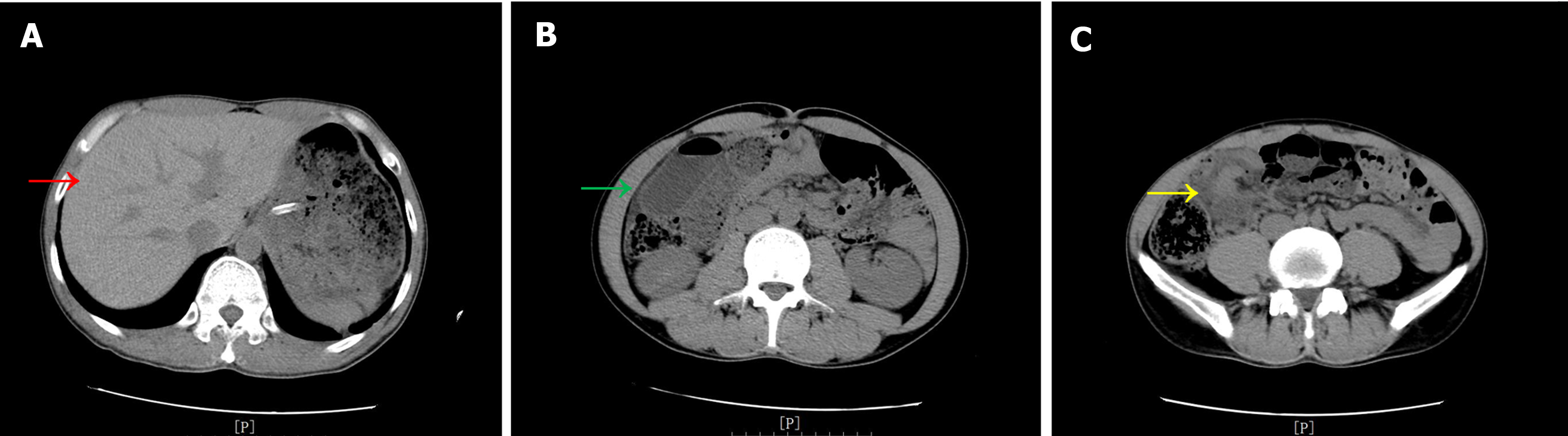
However, the patient's condition deteriorated approximately 2 h after admission, with intensified abdominal pain observed. Subsequent physical examination revealed palpable distension in the lower right quadrant, increased abdominal rigidity, and rebound tenderness. An urgent second abdominal CT scan revealed persistence of the appendiceal fecalith without a significant increase in surrounding effusion, absence of fluid in the abdominopelvic cavity, and worsening dilation of the small intestine in the right lower quadrant and high-density shadows in areas of the intestinal lumen, suggesting potential hemorrhagic intestinal lesions (Figure 2).
The final diagnosis was Meckel's diverticulum with internal hernia and intestinal necrosis.
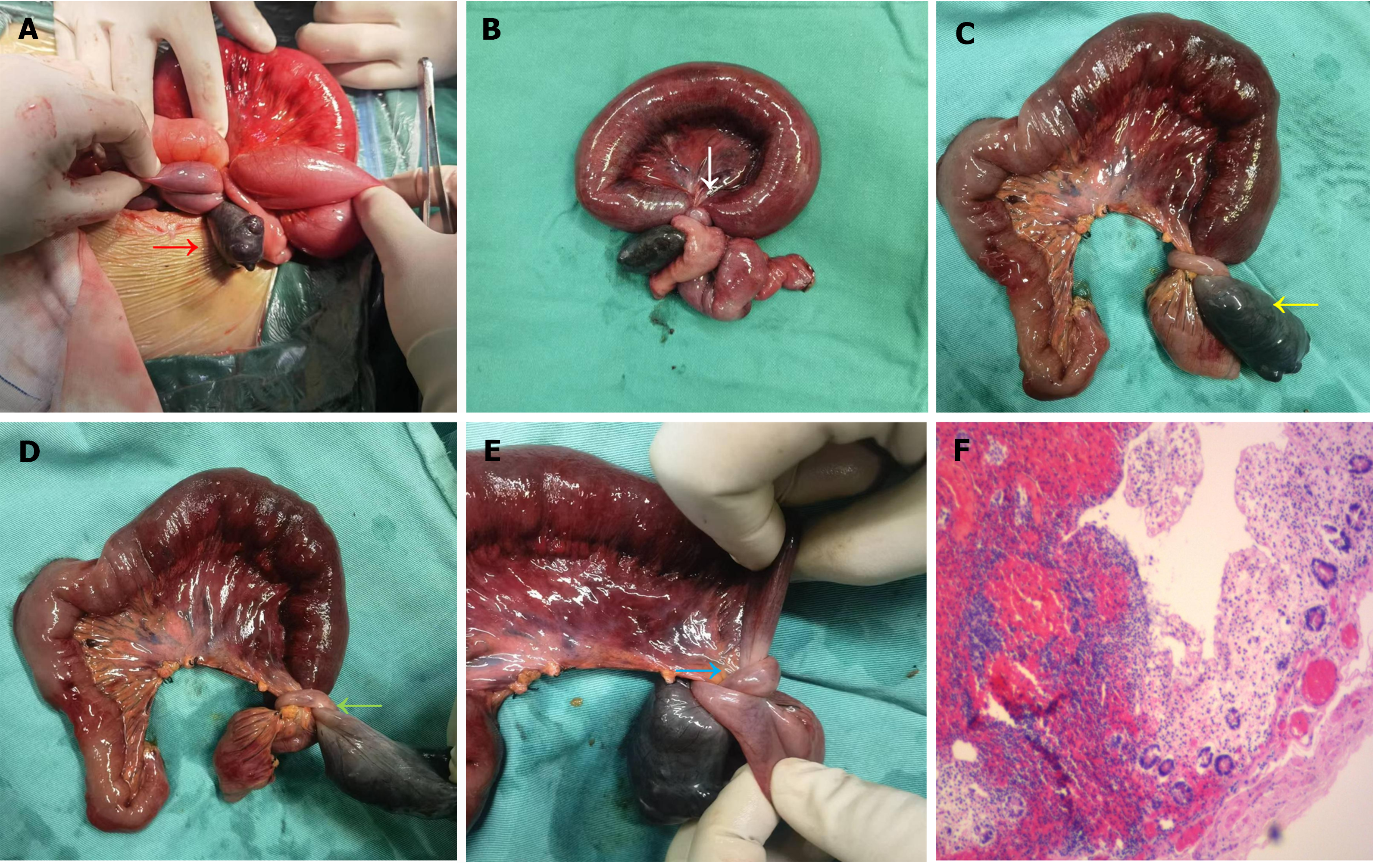
Further assessment revealed progressive worsening of abdominal pain, rapidly progressing to acute peritonitis. CT findings indicated increased small intestinal dilation and fluid accumulation, with high-density shadows in the intestinal lumen, suggesting the possibility of intestinal necrosis with hemorrhage. Emergency surgery was promptly performed after rapid preoperative preparation. Surgical exploration revealed an internal hernia in the small intestine located 50 cm from the ileocecal junction, accompanied by proximal bowel obstruction. The hernial content was identified as a Meckel's diverticulum, measuring approximately 6 cm × 4 cm × 4 cm, that exhibited necrosis, and its base was entrapped in a configuration reminiscent of a surgical knot. Examination of the remaining small intestine and other abdominal organs revealed no abnormalities. Consequently, partial resection of the small intestine followed by intestinal anastomosis was performed (Figure 3A-E).
Pathological examination confirmed the presence of a small intestine diverticulum with necrosis (Figure 3F). The patient recovered well and was discharged one week after surgery. He was advised to undergo regular follow-up visits in the outpatient department.
Meckel's diverticulum, resulting from incomplete involution of the yolk sac during embryonic development, is a frequent congenital anomaly of the gastrointestinal tract. Characterized by a saccular malformation of the ileal wall within 100 cm of the ileocecal valve, its prevalence is relatively low at 2%, predominantly occurring in children younger than 7 years of age[1,2]. Despite its intrinsic asymptomatic nature, complications such as intestinal obstruction, bleeding, perforation, and diverticulitis are major causes for seeking clinical intervention. Owing to the absence of distinct clinical manifestations, preoperative diagnosis is challenging, particularly for terminal ileal Meckel's diverticulum, which may overlap with the location of the appendix and mimic the symptoms, signs, and ultrasound findings of acute appendicitis, fre
In this case, a middle-aged male patient presented at the Emergency Department with a 2-hour history of abdominal pain without previous episodes of recurrent abdominal pain. Upon admission, the chief complaint was right lower quadrant pain, with tenderness noted around McBurney's point upon examination. Routine blood tests indicated an elevated white blood cell count, and abdominal CT suggested the presence of an appendiceal fecalith with slight surrounding effusion, leading to an initial diagnosis of acute appendicitis. Considering recent food intake, the decision was made to defer immediate surgery and instead initiate anti-infective therapy. Notably, the first abdominal CT revealed localized small intestinal dilation in the right lower quadrant, which was initially considered a secondary appendicitis symptom due to the absence of previous abdominal surgeries[4]. The progressive worsening of the patient's pain and abrupt onset of signs of peritonitis necessitated a reevaluation. A subsequent CT scan, conducted 2 h later, revealed exacerbated dilation of the terminal ileum and high-density shadows in the intestinal lumen indicative of intestinal necrosis[5], without significant alterations in the peri-appendiceal effusion. These findings prompted a decisive reversal of the initial diagnosis and urgent surgical exploration.
During the surgical procedure, a midline incision was made in the lower abdomen, revealing a segment of necrotic intestine immediately identified as a Meckel's diverticulum accompanied by internal hernia formation. Palpation of the appendiceal lumen revealed small fecaliths; however, no signs of thickening or inflammatory changes were observed. While infections, perforations, and obstructions associated with small intestinal diverticula are relatively common clinically, spontaneous internal hernia formation secondary to a diverticulum is rare. Involvement of the small intestine in the hernial ring is rarer, and entrapment resembling a surgical knot is even more uncommon. These entrapments pose challenges in release, even after specimen removal. Although the mechanism behind their formation remains unclear, it is speculated to be related to the imbalance of intestinal motility induced by the diverticulum, with heavy dinner consumption possibly acting as a trigger.
For the patient described herein, the duration from admission to definitive diagnosis via surgical exploration was approximately 4 h, and diverticular necrosis and obstruction were rapidly identified. The rapid onset of intestinal necrosis was attributed to delayed surgical exploration and the formation of an internal hernia associated with Meckel's diverticulum. Patients with internal hernias typically manifest severe abdominal pain and display classic signs of intestinal obstruction. CT scans may reveal mesenteric whirlpool changes and abnormal clustering of intestines, which is crucial for early diagnosis[6]. However, imaging diagnosis in this patient was challenging due to the presence of entrapped Meckel's diverticulum, minimal intestinal necrosis, and normal mesenteric morphology. Following the formation of an internal hernia, blood circulation within the diverticulum becomes compromised, exacerbating intestinal necrosis due to entrapment at the diverticulum base. We believe that the main reasons for the patient's misdiagnosis throughout the treatment course were related to the following factors: (1) The patient's abdominal pain was located in the lower right abdomen, and the exudation of fecal stones and their surroundings in the appendix misled the diagnosis; and (2) the patient's Meckel diverticulum was located in the distal ileum, overlapping with the position of the appendix, and the trapped diverticulum was difficult to distinguish on CT. Therefore, this case emphasizes that recognizing atypical abdominal pain is paramount. Vigilant monitoring of abdominal signs, dynamic reassessment of imaging studies, and prompt surgical exploration when warranted, are imperative throughout treatment. Laparoscopic examination is increasingly recommended as a diagnostic and therapeutic modality.
Meckel's diverticulum, a prevalent gastrointestinal condition, typically manifests with clinical manifestations such as diverticulitis. The occurrence of a diverticulum coupled with an internal hernia is clinically rare, making early diagnosis and treatment crucial. This case report highlights the potential for misdiagnosis of Meckel's diverticulum and underscores the significance of differential diagnosis, thus providing valuable diagnostic and therapeutic insights for clinicians.
| 1. | Singh DR, Pulickal GG, Lo ZJ, Peh WC. Clinics in diagnostic imaging (162). Meckel's diverticulum. Singapore Med J. 2015;56:523-6; quiz 527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Park IK, Cho MJ. Clinical characteristics and treatment outcomes of symptomatic Meckel diverticulum: a comparative study among children, adolescent, and adult patients. Ann Surg Treat Res. 2023;105:107-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Yan L, Zhou B, Wu P, Tian Y, Lou Y. Meckel's diverticulum mimicking acute appendicitis in children: a retrospective cohort study. BMC Surg. 2024;24:40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Musa A, Alelyani M, Hadadi I, Ahmed AM, Shubayr N, Alamri S, Osman H, Khandaker MU, Mahmoud MZ. Comparison between computed tomography and ultrasonography to diagnose acute appendicitis in a Saudi population. J Radiati Res Appl Sci. 2024;17:100827. [DOI] [Full Text] |
| 5. | Li BQ, Qi WJ, Yuan M, Wang HY, Chen M, Song ZX, Li Q, Li L, Jiang B, Ma ZL, Xiu DR, Yuan CH. Increased Attenuation of Intestinal Contents at CT Indicates Bowel Necrosis in Closed-Loop Small Bowel Obstruction. Radiology. 2024;310:e231710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 6. | Dilauro M, McInnes MD, Schieda N, Kielar AZ, Verma R, Walsh C, Vizhul A, Petrcich W, Mamazza J. Internal Hernia after Laparoscopic Roux-en-Y Gastric Bypass: Optimal CT Signs for Diagnosis and Clinical Decision Making. Radiology. 2017;282:752-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/