Published online Jul 16, 2024. doi: 10.12998/wjcc.v12.i20.4397
Revised: May 13, 2024
Accepted: May 24, 2024
Published online: July 16, 2024
Processing time: 94 Days and 23.6 Hours
Ischemic stroke is a rare event associated with an elevated risk of blood clot formation owing to an underlying malignancy. Herein, we present a case of ovarian carcinoma that led to cerebral infarction.
A 43-year-old woman experienced sudden onset right-sided paralysis and difficulty speaking two days after discovery of a large ovarian tumor measuring approximately 14 cm, which was suspected to be malignant. Further examination revealed left middle cerebral artery infarction. The patient had a history of hypertension and adenomyosis. Following stabilization with heparin treatment and vital signs management, the patient underwent debulking surgery, including total hysterectomy, bilateral salpingo-oophorectomy, omentectomy, and bilateral pelvic and para-aortic lymph node dissection. The final diagnosis was clear cell carcinoma of the right ovary (stage IA). Subsequently, the patient completed six rounds of adjuvant chemotherapy while simultaneously undergoing rehabilitation. Presently, the patient is able to walk independently, although she still experiences aphasia.
Prompt medical intervention and interdisciplinary care are crucial in the setting of incidental findings such as a large ovarian tumor.
Core Tip: We report a case of ischemic stroke associated with ovarian cancer. We have updated the information on ovarian cancer with concurrent ischemic stroke regarding its symptoms, signs, diagnosis, and treatment. Because of the rarity of combined ischemic stroke and ovarian cancer, we provide a strategy for diagnosing and treating this condition.
- Citation: Siu WYS, Ding DC. Ischemic stroke with concomitant clear cell carcinoma of the ovary: A case report and review of literature. World J Clin Cases 2024; 12(20): 4397-4404
- URL: https://www.wjgnet.com/2307-8960/full/v12/i20/4397.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i20.4397
Ovarian cancer is a relatively rare but severe malignancy that develops in the ovaries and female reproductive organs[1]. It ranks fifth in cancer-related deaths among women, with approximately 1000 new cases diagnosed annually in Taiwan[2]. The symptoms of ovarian cancer are often vague and nonspecific, including abdominal bloating, pelvic pain, urinary urgency, and changes in bowel habits[3]. Owing to the lack of specific symptoms, ovarian cancer is frequently diagnosed at an advanced stage, emphasizing the importance of awareness and early detection[4].
Diagnosis typically involves a combination of imaging tests, such as ultrasound and computed tomography (CT), alongside blood tests to measure tumor markers such as CA-125 levels[5]. A definitive diagnosis is made through surgical biopsy and histological examination of the ovarian tissue. Treatment strategies vary based on the disease stage, patient age, and overall health. The primary treatment typically involves surgery for tumor resection, followed by chemotherapy to target any remaining cancer cells[6].
Ischemic stroke is a leading cause of disability and mortality worldwide and occurs when a blood vessel in the brain is blocked by a clot or narrowed due to atherosclerosis[7]. Ischemic strokes account for approximately 87% of all stroke cases[7]. The symptoms of ischemic stroke typically manifest suddenly and include weakness or paralysis on one side of the body, difficulty speaking or understanding speech, sudden confusion, vision problems, and severe headache. Prompt recognition of these symptoms is critical, as early intervention can minimize brain damage and improve outcomes[7].
The diagnosis of ischemic stroke involves a thorough neurological examination, imaging studies such as CT or magnetic resonance imaging to confirm the presence of a clot and determine the extent of brain damage, and additional tests such as Doppler ultrasound or angiography to identify the underlying cause[8].
Treatment aims to restore blood flow to the affected brain areas and prevent further damage. This may involve administering clot-dissolving medications (thrombolytics) such as tissue plasminogen activator or performing mechanical thrombectomy to remove clots directly[9,10]. Supportive care, rehabilitation, and lifestyle modification to reduce stroke risk factors are crucial components of stroke management. Early recognition, rapid intervention, and comprehensive care are essential for optimizing outcomes in individuals with ischemic stroke.
Ischemic stroke is an uncommon occurrence resulting from an increased tendency for blood clot formation induced by an underlying malignancy[11]. Venous thromboembolism (VTE) is the leading secondary cause of death in patients with ovarian cancer, especially those with clear cell histology[12]. However, the incidence of arterial thrombosis in patients with ovarian carcinoma is only 2.4%, and cerebral infarction accounts for only 2.2%[12].
Herein, we describe a case of ovarian clear cell carcinoma with concurrent cerebral infarction.
Sudden onset of right hemiplegia and aphasia for 2 days.
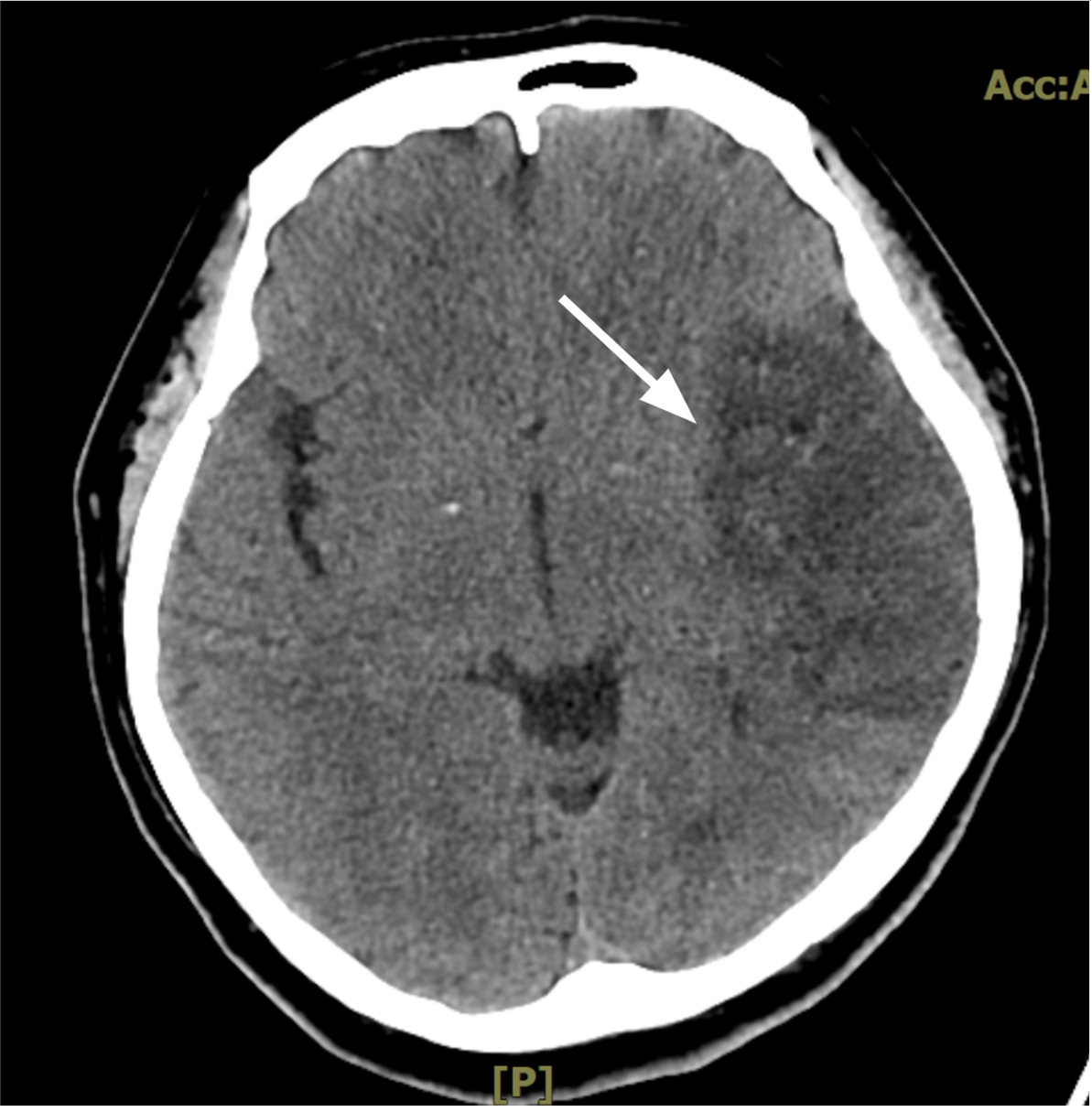
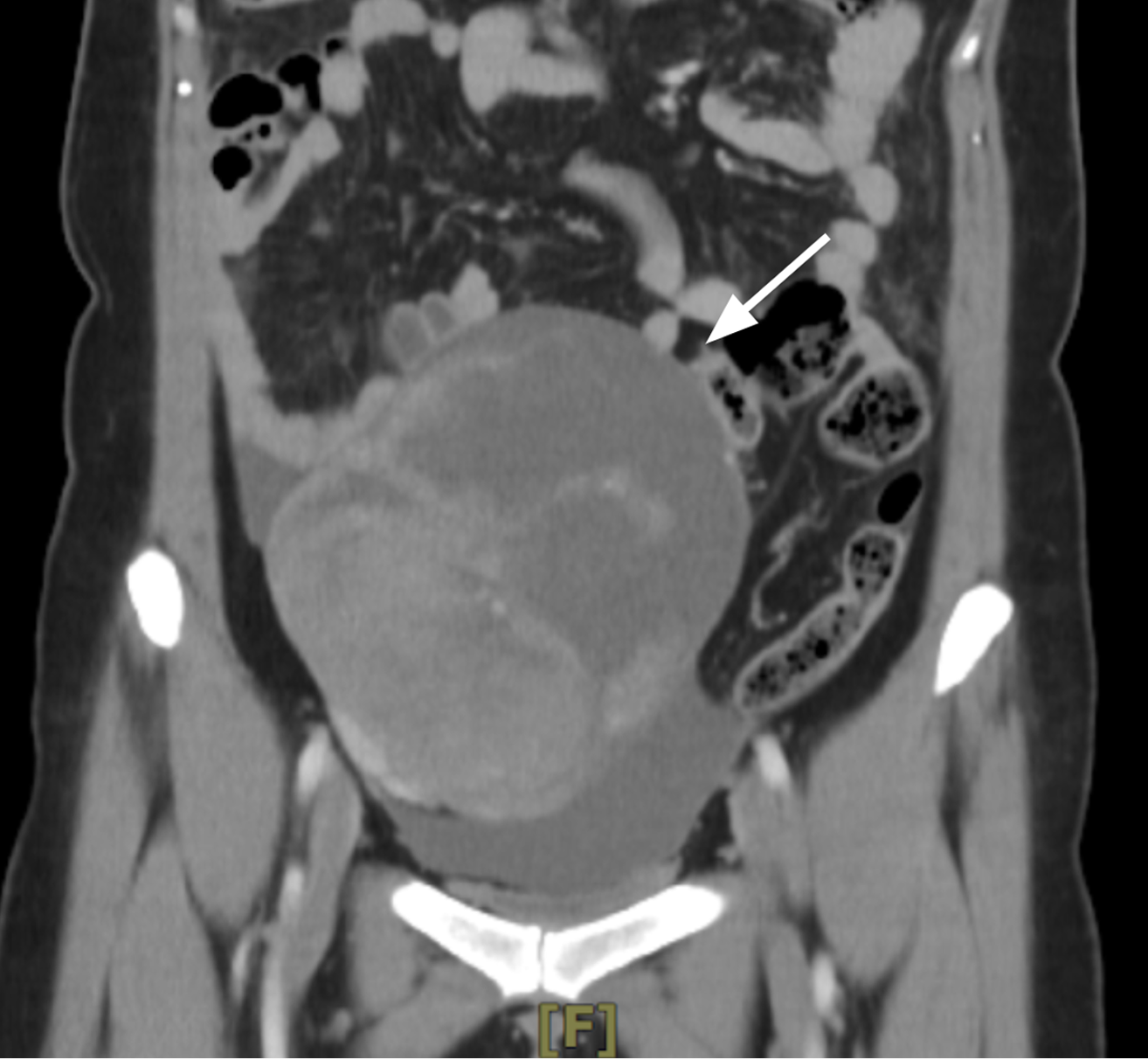
A 43-year-old female (G0P0) experienced a sudden onset of right hemiplegia and aphasia. Two days prior, a large ovarian tumor measuring approximately 14 cm and suspected to be malignant was found incidentally. She visited our emergency room, where a brain CT scan showed a left parietal hypodensity without intracranial hemorrhage and was diagnosed with a left middle cerebral artery infarction. Abdominal CT revealed a 14 cm ovarian tumor in the right pelvis. She was admitted to the surgical intensive care unit, where heparin therapy was initiated. After one week of therapy, her vital signs were stable, heparin therapy was discontinued, and she was transferred to the gynecologic service.
The patient’s medical history was significant for hypertension controlled on antihypertensive medications. She had adenomyosis. The patient was nulliparous.
The patient’s father had a history of colon cancer, but no other family history of cancer was recorded.
The patient was 160 cm tall and weighed 65.4 kg. Her body mass index was 25.5, and her blood pressure upon admission was 182/97 mmHg. One week after admission, a blood pressure of 142/83 mmHg was noted on the day of surgery. On postoperative day 9 (day of discharge), the patient’s blood pressure was 132/85 mmHg. She presented with right hemiparesis, aphasia, and an ill-looking appearance. The patient’s motor power was 0 in the right upper and lower extremities and 4 in the left upper and lower extremities. The pupils were located at the midline. Babinski’s sign was positive. Clear breath sounds and regular heartbeats were also observed. Vaginal examination revealed a pinpoint cervical opening and an enlarged pelvic tumor.
All tumor markers were elevated including carcinoembryonic antigen (18.4 ng/mL; normal limit: 3.0 ng/mL), CA125 (676.5 U/mL; normal limit: 35.0 U/mL), and CA19-9 (52.9 U/mL; normal limit: 35.0 UmL). Electrocardiogram findings were normal. Before the operation, D-Dimer was 7361 ng/mL. The D-dimer value was returned to normal (325.99 ng/mL) 2 months postoperatively.
CT revealed a left parietal hypodensity without intracranial hemorrhage (Figure 1). Transabdominal ultrasonography revealed a large pelvic tumor measuring 14 cm × 9 cm. CT revealed a 14.2 cm mixed cystic and solid component tumor in the pelvic cavity (Figure 2). We did not find thrombus in other body parts.
The final diagnosis was clear cell carcinoma of the right ovary, stage IA. An ischemic stroke was noted at the left middle cerebral artery.
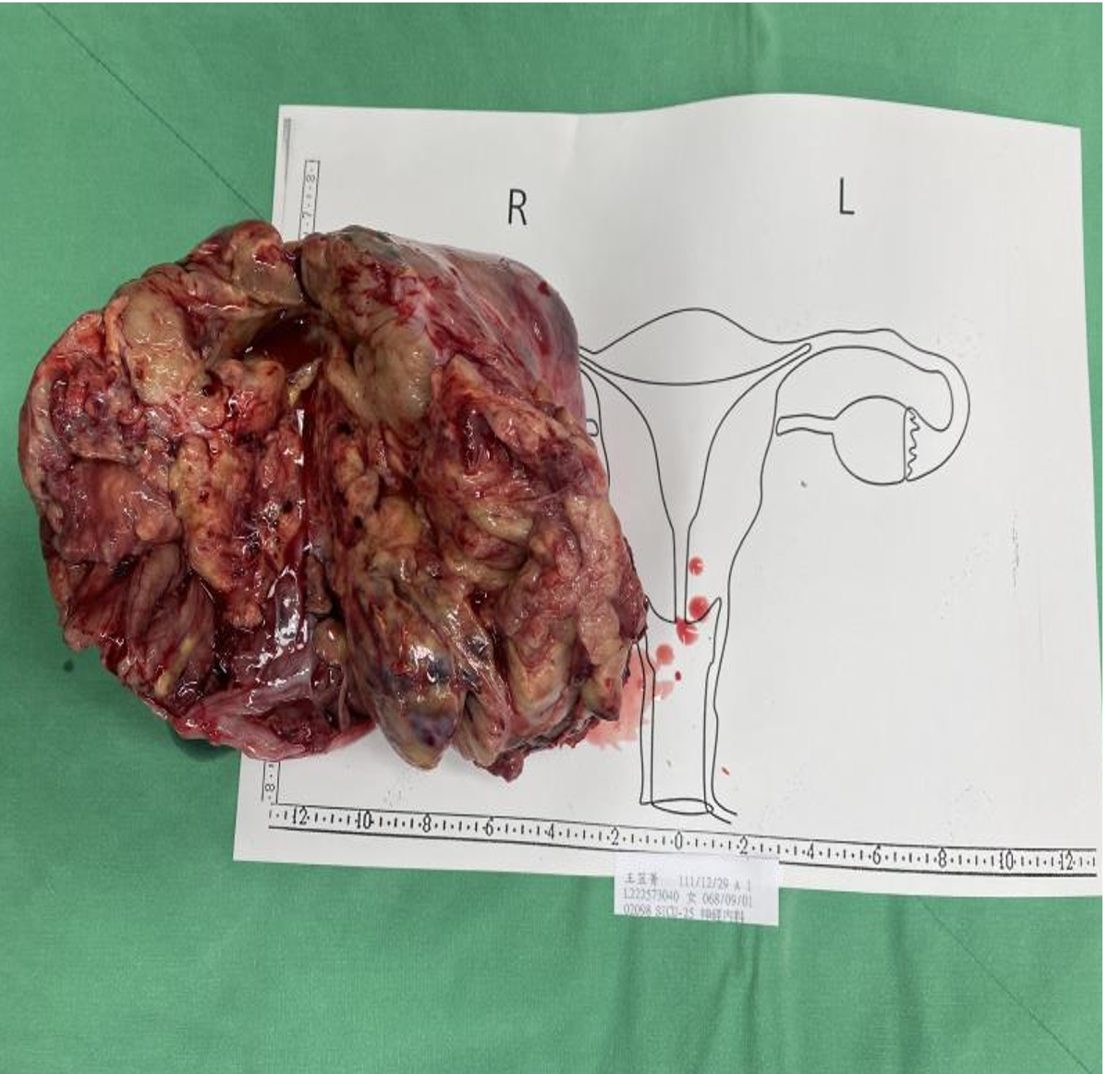
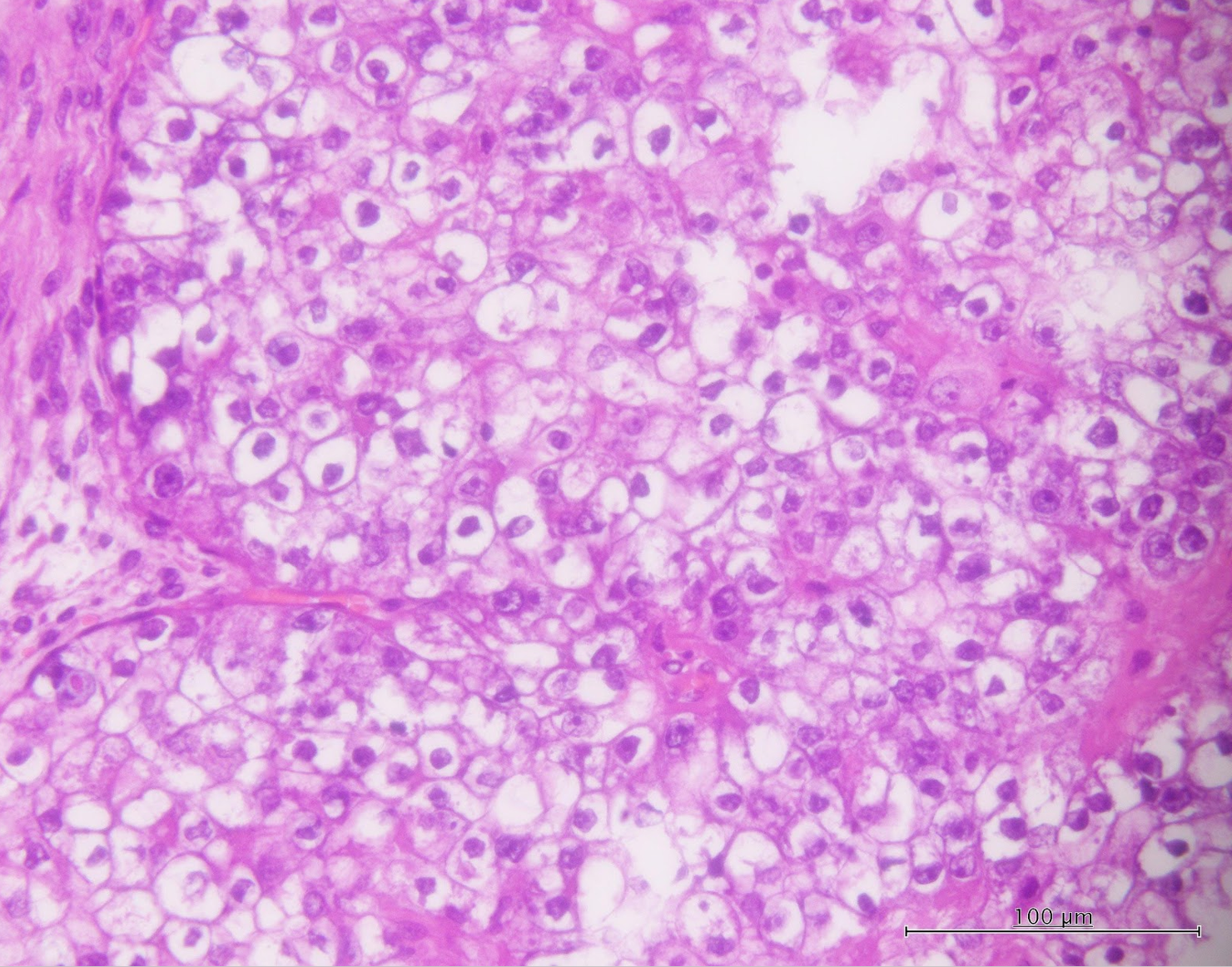
After one week of heparin therapy, her stroke status was stable. The patient underwent debulking surgery with total hysterectomy, bilateral salpingo-oophorectomy, pelvic and para-aortic lymphadenectomy, and omentectomy (Figure 3). Histopathological examination revealed stage IC clear cell carcinoma of the ovary (Figure 4). After surgery, adjuvant chemotherapy with paclitaxel (175 mg/m2) and carboplatin (dose-area under the curve = 5) was administered.
The patient received six courses of adjuvant chemotherapy. The tumor markers returned to normal levels after treatment. During treatment with chemotherapy, the patient underwent simultaneous rehabilitation. Regarding subsequent therapy for stroke, she received a subcutaneous injection of 60 mg clexane for two months. The novel anticoagulation agent, dabigatran (150 mg twice daily), was given for three months. Thereafter, 100 mg of aspirin was administered daily. Antihypertensive medications were administered. After follow-up for one year and four months, she was able to walk independently, but aphasia persisted.
Ovarian clear cell carcinoma is a subtype of epithelial ovarian cancer comprising approximately 5%–10% of all ovarian malignancies[13]. While it is less common than histological subtypes such as serous carcinoma, its prevalence varies depending on geographic and ethnic factors. Clear cell carcinoma of the ovary is characterized by distinct histological features[13]. Under a microscope, the tumor cells have a clear cytoplasm owing to the accumulation of glycogen and lipids[14]. Additionally, clear cell carcinomas often present with hobnail cells and papillary structures. Dysregulation of the PI3K/AKT/mTOR pathway has also been implicated in the pathogenesis of this cancer subtype[15]. Clinically, ovarian clear-cell carcinoma tends to present at an advanced stage, and is often associated with resistance to conventional platinum-based chemotherapy[16]. Patients with clear cell carcinoma may have a poorer prognosis than those with other histological subtypes of ovarian cancer[17].
Trousseau syndrome, first described in 1865 by Armand Trousseau, describes the hypercoagulability associated with malignant diseases[18]. Although ovarian cancer has a high incidence of VTE, cerebral infarction or arterial embolism rarely occur in ovarian cancer[19]. In a study that included 13031 patients with ovarian cancer, 5.2% had VTE events within 24 months[20]. Compared to patients with VTE or pulmonary embolism, patients with ovarian cancer rarely develop cerebral infarction[21]. In a retrospective study consisting of 827 patients with primary epithelial ovarian cancer, 3.2% presented with cerebral infarction within one year before the commencement of treatment for malignant disease or during initial clinical treatment[18]. This study also demonstrated a statistically significant association between cerebral infarction occurrence and the histological subtype of clear cell carcinoma. Tissue factors, cancer procoagulants, and inflammatory cytokines such as interleukin (IL)-6 all play essential roles in promoting hypercoagulable states in ovarian cancer. Clear cell carcinoma is associated with excess levels of tissue factor and IL-6 and is thus more likely to lead to the development of VTE[22].
Generally, risk factors for arterial thromboembolic events in other parts of the body, including the heart and brain, are hypertension, hyperlipidemia, obesity, diabetes, and smoking[23]. In gynecology, taking combined oral contraceptive pills or hormone replacement therapy increases the arterial thromboembolic risk[24]. In a prospective cohort study documenting 893 incident stroke cases, women with endometriosis had a 34% greater risk of stroke than those without endometriosis[25]. Also, in another study of 521612 participants, endometriosis was significantly associated with increased risks of ischemic stroke[26]. Endometriosis can increase arterial stiffness; thus, patients may be at an increased cardiovascular risk[27].
We searched the literature and found one populational study and 15 case reports related to this topic (Table 1)[19,21,28-40]. The patients’ ages ranged from 35 to 76 years, and most patients had a history of hypertension. The tumor stages ranged from I to IV. The most commonly used chemotherapeutic regimens in these reports were carboplatin and paclitaxel, and five of the 13 patients died. The populational study revealed ovarian cancer patients faced a heightened likelihood of experiencing ischemic stroke, with age, hypertension, diabetes, and chemotherapy treatment emerging as distinct risk factors[39].
| Ref. | Year | Age | BMI (kg/m2) | Parity | History of hypertension | Stage | Thrombosis site | Adjuvant therapy | Status |
| Blustein et al[19] | 2023 | 35 | No record | 1 | Yes | IIB | Right MCA | Carboplatin, dose-dense paclitaxel for 6 courses | Survive |
| You et al[30] | 2022 | 41 | No record | No record | No record | No record | Left parietal, temporal lob | Neoadjuvant therapy × 3 | Died |
| Tandi et al[33] | 2022 | 76 | No record | No record | No | IIA | posterior cortical artery | No record | No record |
| Farooqui et al[34] | 2021 | 52 | No record | No record | No | IV | Right MCA and ACA | No record | No record |
| Chen et al[21] | 2020 | 46 | 21.8 | No record | Yes | IIIC | Deep vein thrombosis and pulmonary embolism | Carboplatin, paclitaxel for 3 courses | Survive |
| Sakuta et al[35] | 2019 | 55 | No record | No record | No | IV | Left MCA | Not yet started | Survive |
| Potugari et al[36] | 2019 | 52 | No record | No record | Yes | IIIB | Multiple acute and subacute infarcts in the brain | Neoadjuvant therapy × 6, post-op chemotherapy × 3 | Survive |
| Ricci et al[37] | 2018 | 57 | No record | No record | No | No record | Left mesial-occipital lobe | Yes | Survive |
| Lin et al[31] | 2015 | 60 | Not record | Not record | Yes | IIIC, recurrent | Bilateral cerebra and cerebella | No | Died |
| Yagi et al[38] | 2014 | 54 | No record | No record | No | No record | Right MCA | No | Died 3 weeks after the onset of stroke |
| Kuan et al[39] | 2014 | 49 (median of 8810 patients) | No record | No record | Yes (risk factor) | No record | Ischemic stroke risk: 1.38-fold | No record | No record |
| Tadokoro et al[40] | 2013 | 55, 56 | No record | No record | No | No record | Left MCA | No record | No record |
| Naoi et al[28] | 2013 | 55, 62 | No record | No record | No record, Yes | IIIC, IC | Bilateral thalamus, right frontal lobe, and left cerebellum | Carboplatin, paclitaxel for 6 courses, recurrence | Died, survive |
| Devulapalli et al[29] | 2012 | 62 | No record | No record | Yes | I | Occipital | Carboplatin, paclitaxel for 6 courses | Survive |
| Oueida et al[32] | 2011 | 56 | Not record | Not record | No | IC | Endocarditis with multi-organ embolic infarction | 5 courses of adjuvant chemotherapy | Died |
| Current case | 2024 | 43 | 25.5 | 0 | Yes | IA | Left MCA | Carboplatin, paclitaxel for 6 courses | Survive |
Given the known association between ovarian malignancy and thromboembolic states, it is reasonable to relate the hypercoagulable state of ovarian cancer to the cerebral infarction event in this case.
Clear ovarian cell carcinomas may be associated with thromboembolic events. Therefore, malignancy should be considered a risk factor for cerebral infarction development, particularly in patients diagnosed with ovarian cancer.
| 1. | Rizzuto I, Behrens RF, Smith LA. Risk of ovarian cancer in women treated with ovarian stimulating drugs for infertility. Cochrane Database Syst Rev. 2019;6:CD008215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Teng YH, Liu FC, Huang SY, Kuo CF, Yu HP. Epidemiology and Mortality of Ovarian Cancer in Taiwan: A Population-Based Study. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 3. | Brain KE, Smits S, Simon AE, Forbes LJ, Roberts C, Robbé IJ, Steward J, White C, Neal RD, Hanson J; ICBP Module 2 Working Group. Ovarian cancer symptom awareness and anticipated delayed presentation in a population sample. BMC Cancer. 2014;14:171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Radu CA, Matos de Melo Fernandes N, Khalfe S, Stordal B. Awareness of ovarian cancer symptoms and risk factors in a young ethnically diverse British population. Cancer Med. 2023;12:9879-9892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 5. | Guo B, Lian W, Liu S, Cao Y, Liu J. Comparison of diagnostic values between CA125 combined with CA199 and ultrasound combined with CT in ovarian cancer. Oncol Lett. 2019;17:5523-5528. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Matulonis UA, Sood AK, Fallowfield L, Howitt BE, Sehouli J, Karlan BY. Ovarian cancer. Nat Rev Dis Primers. 2016;2:16061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 541] [Cited by in RCA: 905] [Article Influence: 90.5] [Reference Citation Analysis (0)] |
| 7. | Kuriakose D, Xiao Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 445] [Cited by in RCA: 718] [Article Influence: 119.7] [Reference Citation Analysis (0)] |
| 8. | H Buck B, Akhtar N, Alrohimi A, Khan K, Shuaib A. Stroke mimics: incidence, aetiology, clinical features and treatment. Ann Med. 2021;53:420-436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 9. | Wardlaw JM, Murray V, Berge E, del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. 2014;2014:CD000213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 287] [Cited by in RCA: 343] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 10. | Castaño C, Remollo S, García MR, Hidalgo C, Hernández-Perez M, Ciorba M. Mechanical thrombectomy with 'ADAPT' technique by transcervical access in acute ischemic stroke. Neuroradiol J. 2015;28:617-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Bang OY, Chung JW, Lee MJ, Seo WK, Kim GM, Ahn MJ; OASIS-Cancer Study Investigators. Cancer-Related Stroke: An Emerging Subtype of Ischemic Stroke with Unique Pathomechanisms. J Stroke. 2020;22:1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 109] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 12. | Weeks KS, Herbach E, McDonald M, Charlton M, Schweizer ML. Meta-Analysis of VTE Risk: Ovarian Cancer Patients by Stage, Histology, Cytoreduction, and Ascites at Diagnosis. Obstet Gynecol Int. 2020;2020:2374716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Tang H, Liu Y, Wang X, Guan L, Chen W, Jiang H, Lu Y. Clear cell carcinoma of the ovary: Clinicopathologic features and outcomes in a Chinese cohort. Medicine (Baltimore). 2018;97:e10881. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (11)] |
| 14. | Khan T, He Y, Kryza T, Harrington BS, Gunter JH, Sullivan MA, Cuda T, Rogers R, Davies CM, Broomfield A, Gough M, Wu AC, McGann T, Weroha SJ, Haluska P, Forbes JM, Armes JE, Barry SC, Coward JI, Jagasia N, Chetty N, Snell CE, Lourie R, Perrin LC, Hooper JD. Disruption of Glycogen Utilization Markedly Improves the Efficacy of Carboplatin against Preclinical Models of Clear Cell Ovarian Carcinoma. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Driva TS, Schatz C, Haybaeck J. Endometriosis-Associated Ovarian Carcinomas: How PI3K/AKT/mTOR Pathway Affects Their Pathogenesis. Biomolecules. 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 29] [Reference Citation Analysis (0)] |
| 16. | Matsuzaki S, Yoshino K, Ueda Y, Matsuzaki S, Kakuda M, Okazawa A, Egawa-Takata T, Kobayashi E, Kimura T. Potential targets for ovarian clear cell carcinoma: a review of updates and future perspectives. Cancer Cell Int. 2015;15:117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Lee YY, Kim TJ, Kim MJ, Kim HJ, Song T, Kim MK, Choi CH, Lee JW, Bae DS, Kim BG. Prognosis of ovarian clear cell carcinoma compared to other histological subtypes: a meta-analysis. Gynecol Oncol. 2011;122:541-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 84] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Takano H, Nakajima K, Nagayoshi Y, Komazaki H, Suzuki J, Tanabe H, Niimi S, Isonishi S, Okamoto A. Clinical associations of Trousseau's syndrome associated with cerebral infarction and ovarian cancer. J Gynecol Oncol. 2018;29:e67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Blustein P, Werner S, Sham S, Febles A, Katz H, Villella J. Right middle cerebral artery stroke secondary to ovarian clear cell carcinoma in a 35-year-old: A case report. Case Rep Womens Health. 2023;37:e00485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 20. | Rodriguez AO, Wun T, Chew H, Zhou H, Harvey D, White RH. Venous thromboembolism in ovarian cancer. Gynecol Oncol. 2007;105:784-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 130] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 21. | Chen J, Sun H, Wu M, Zhong X, Zhang Y. Spontaneous arterial thrombosis in a patient with advanced ovarian clear cell cancer: a case report and literature review. J Int Med Res. 2020;48:300060520926742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 22. | Uno K, Homma S, Satoh T, Nakanishi K, Abe D, Matsumoto K, Oki A, Tsunoda H, Yamaguchi I, Nagasawa T, Yoshikawa H, Aonuma K. Tissue factor expression as a possible determinant of thromboembolism in ovarian cancer. Br J Cancer. 2007;96:290-295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 131] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 23. | Sharifi-Rad J, Rodrigues CF, Sharopov F, Docea AO, Can Karaca A, Sharifi-Rad M, Kahveci Karıncaoglu D, Gülseren G, Şenol E, Demircan E, Taheri Y, Suleria HAR, Özçelik B, Nur Kasapoğlu K, Gültekin-Özgüven M, Daşkaya-Dikmen C, Cho WC, Martins N, Calina D. Diet, Lifestyle and Cardiovascular Diseases: Linking Pathophysiology to Cardioprotective Effects of Natural Bioactive Compounds. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 192] [Cited by in RCA: 166] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 24. | Gialeraki A, Valsami S, Pittaras T, Panayiotakopoulos G, Politou M. Oral Contraceptives and HRT Risk of Thrombosis. Clin Appl Thromb Hemost. 2018;24:217-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 25. | Farland LV, Degnan WJ 3rd, Bell ML, Kasner SE, Liberman AL, Shah DK, Rexrode KM, Missmer SA. Laparoscopically Confirmed Endometriosis and Risk of Incident Stroke: A Prospective Cohort Study. Stroke. 2022;53:3116-3122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 26. | Zheng M, Zheng S. Endometriosis Increases the Risk of Stroke: A Mendelian Randomization Study. Stroke. 2023;54:e30-e33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 27. | Li PC, Yang YC, Wang JH, Lin SZ, Ding DC. Endometriosis Is Associated with an Increased Risk of Coronary Artery Disease in Asian Women. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Naoi H, Hashimoto H, Kajimoto E, Takeda M, Yoshida S, Miyatake T, Yokoi T, Isaka S, Nagamatsu M. Cerebral infarctions as manifestation of ovarian clear cell carcinoma: report of two cases and review of the literature. Int Cancer Conf J 2013; 2: 206–10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Devulapalli S, Pinto N, Gandothra C, Jayam-Trouth A, Kurukumbi M. A rare case of occipital stroke as a consequence of nonbacterial thrombotic endocarditis in ovarian clear cell carcinoma: a case report. Case Rep Neurol. 2012;4:84-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | You Y, Chen X, Jiang Y, Cheng W. Ovarian clear cell cancer associated with Trousseau syndrome: A case report and literature review. Medicine (Baltimore). 2022;101:e32106. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 31. | Lin YK, Lee JT, Yang FC, Sung YF, Kao HW, Lin CC, Hsu CH. Systemic embolic events with nonbacterial thrombotic endocarditis as manifestations of recurrent ovarian clear cell carcinoma. Taiwan J Obstet Gynecol. 2015;54:625-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Oueida Z, Scola M. Ovarian Clear Cell Carcinoma Presenting as Non-bacterial Thrombotic Endocarditis and Systemic Embolization. World J Oncol. 2011;2:270-274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 33. | Tandi R, Bansal S, Sahu S, Dinesh Eshwar M, Raghavan P, Kulkarni OV, Natarajan B, Dodda S, Banur A. Stroke as a Paraneoplastic Manifestation of Ovarian Cancer: A Case Report. Cureus. 2022;14:e29835. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 34. | Farooqui AA, Ashraf R, D'Ornellas R, Aslam A, Marcelin M, Shetty V. Tricuspid Valve Vegetation Secondary to Ovarian Cancer Leading to Acute Stroke via Pulmonary Arteriovenous Malformation. Cureus. 2021;13:e17136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 35. | Sakuta K, Mukai T, Fujii A, Makita K, Yaguchi H. Endovascular Therapy for Concurrent Cardio-Cerebral Infarction in a Patient With Trousseau Syndrome. Front Neurol. 2019;10:965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 36. | Potugari BR, Priyanka P, Komanapalli SD, Mercier RJ. Ovarian Cancer Presenting as Cryptogenic Stroke from Patent Foramen Ovale. Clin Med Res. 2019;17:97-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 37. | Ricci S, Lupato A, Polo A, Sacco S. Recurrent ischemic stroke of undetermined cause revealed an occult malignancy. Neurol Sci. 2018;39:383-384. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 38. | Yagi T, Takahashi K, Tanikawa M, Seki M, Abe T, Suzuki N. Fatal intracranial hemorrhage after intravenous thrombolytic therapy for acute ischemic stroke associated with cancer-related nonbacterial thrombotic endocarditis. J Stroke Cerebrovasc Dis. 2014;23:e413-e416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 39. | Kuan AS, Teng CJ, Wu HH, Su VY, Chen YT, Chien SH, Yeh CM, Hu LY, Chen TJ, Tzeng CH, Liu CJ. Risk of ischemic stroke in patients with ovarian cancer: a nationwide population-based study. BMC Med. 2014;12:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 40. | Tadokoro Y, Sakaguchi M, Yagita Y, Furukado S, Okazaki S, Fujinaka T, Kimura T, Yoshimine T, Mochizuki H, Kitagawa K. Ischemic stroke in patients with solid gynecologic tract tumors and coagulopathy. Eur Neurol. 2013;70:304-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/