Published online May 6, 2024. doi: 10.12998/wjcc.v12.i13.2269
Peer-review started: December 22, 2023
First decision: January 10, 2024
Revised: January 25, 2024
Accepted: March 20, 2024
Article in press: March 20, 2024
Published online: May 6, 2024
Processing time: 124 Days and 21.7 Hours
Invasive functional evaluation by fractional flow reserve (FFR) is considered as a gold standard for the evaluation of intermediate coronary stenosis. However, in patients with diabetes due to accelerated progression of atherosclerosis the outcome may be worse even in the presence of negative functional testing.
We present a case of 55-year-old male diabetic patient who was admitted for chest pain. Diagnostic coronary angiography disclosed 2 intermediate stenoses of the obtuse marginal branch with no evidence of restenosis on previously implanted stent. Patient undergone invasive functional testing of intermediate lesion with preserved FFR (0.88), low coronary flow reserve (1.2) and very high index of mi
Combined functional and anatomic imaging of intermediate coronary stenosis in diabetic patients represent comprehensive contemporary decision pathway in the management of the patients.
Core Tip: We present a case of the diabetic patient with moderate-to-severe coronary stenosis with preserved fractional flow reserve, low coronary flow reserve, high index of microvascular resistance and intravascular optical coherence tomography image demonstrating fibrotic plaque without signs of thin-cup fibroatheroma. Combined functional and anatomic imaging of intermediate coronary stenosis represent comprehensive contemporary decision pathway in the management of the patients.
- Citation: Al Nooryani A, Aboushokka W, Beleslin B, Nedeljkovic-Beleslin B. Deferred revascularization in diabetic patient according to combined invasive functional and intravascular imaging data: A case report. World J Clin Cases 2024; 12(13): 2269-2274
- URL: https://www.wjgnet.com/2307-8960/full/v12/i13/2269.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i13.2269
Fractional flow reserve (FFR) is considered as a functional gold standard for the evaluation of coronary stenosis, and the decision for management of intermediate coronary stenosis should be based on functional evaluation[1]. Still, there are some clinical conditions, such as patients with diabetes mellitus (DM) where the value of FFR is still not so well validated and defined. In fact, the previous data have shown that the outcome of deferred lesions according to negative FFR is worse in patients with DM in comparison to non-diabetic patients[2]. In addition, COMBINE optical coherence tomo
We present a case of 55-year-old male diabetic patient who was admitted to our clinic for chest pain syndrome. His chest pain appeared occasionally during last 2 wk and had rather atypical presentation both at rest and after exertion. It was not accompanied by any other symptoms like dyspnea, fatigue or nausea. Due to recent appearance of chest pain of uncertain origin as well as previous implanted stent in left main coronary artery, the patient was referred directly to invasive coronary angiography without non/invasive functional testing.
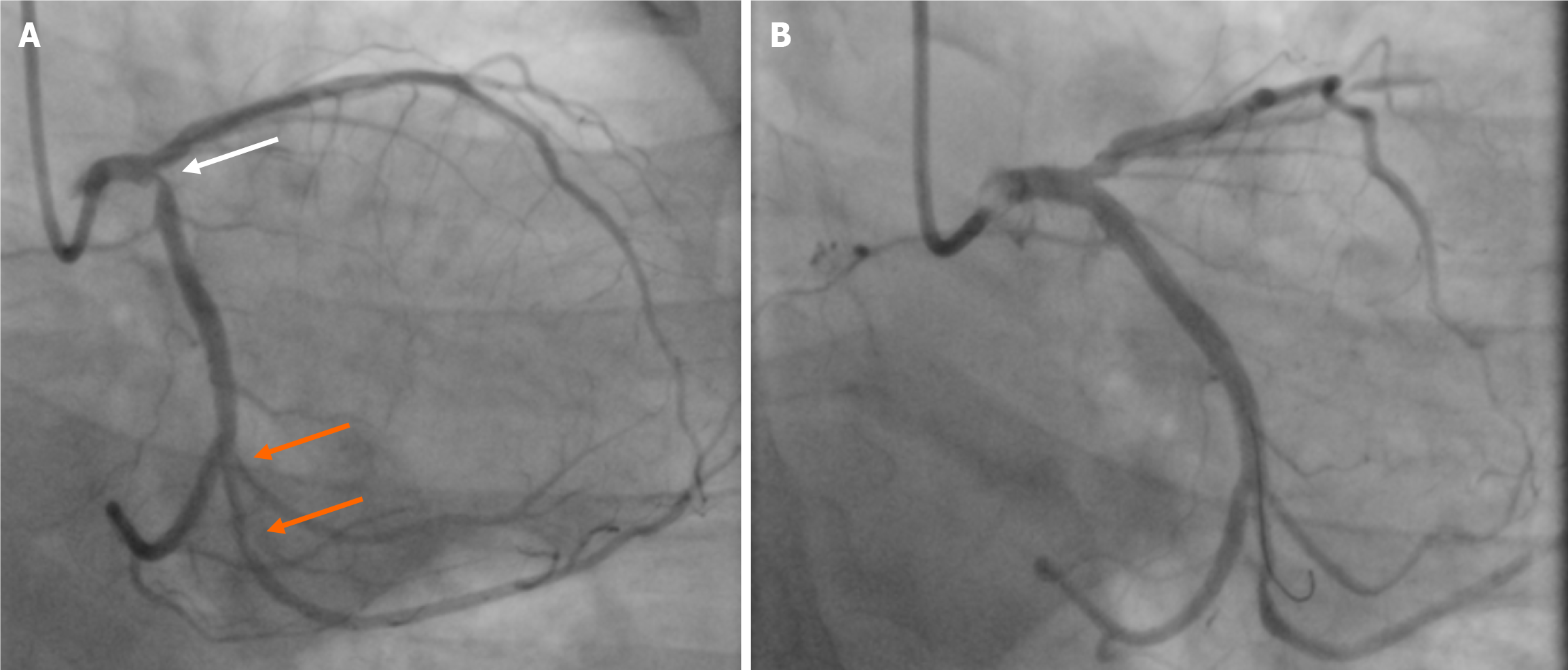
Three years ago, he suffered from non-ST segment elevation myocardial infarction due to critical lesion of the ostial circumflex (Cx) artery which was treated with implantation of one drug-eluting stent (DES) with crossover from left main to Cx coronary artery (Figure 1). Following DES implantation from left main to Cx, 2 intermediate stenoses of the proximal part of the long second obtuse marginal branch (Figure 1A, orange arrows) were observed that were estimated to be not significant without a need for further intervention. Four years ago, he also had percutaneous coronary intervention with one DES implantation in the right coronary artery (RCA). Since the last coronary event, the patient has been free of any symptom, he was feeling physically and emotionally fit. His medications included aspirin, beta-blockers, and rosuvastatin.
Patient has been obese (102 kg), and has elevated HbA1c levels with no regular anti-diabetic therapy.
Patient denies smoking, doesn’t have hypertension, and denies alcohol abuse. He has elevated cholesterol levels treated with statins.
On physical examination there was no remarkable finding. His blood pressure was 130/80 mmHg. His heart sounds were normal, without significant murmurs. His lung fields were clear, and there were no signs of heart failure. His ECG was normal with sinus rhythm, heart rate of 62/min, without conduction and rhythm disturbances as well as ST-T changes.
The laboratory values showed normal blood count, elevated low density lipoprotein (LDL)-cholesterol of 2.3 mmol/L, HbA1c was 6.1%, and the renal function was preserved with estimated glomerular filtration rate of 75 mL/min/1.73m2.
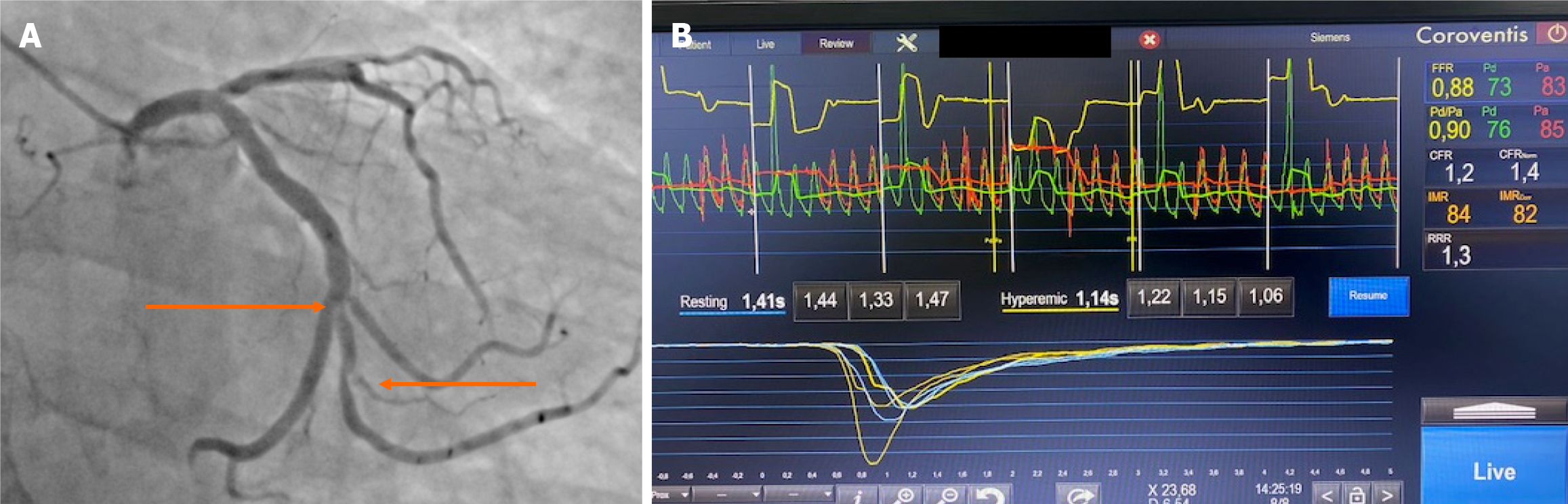
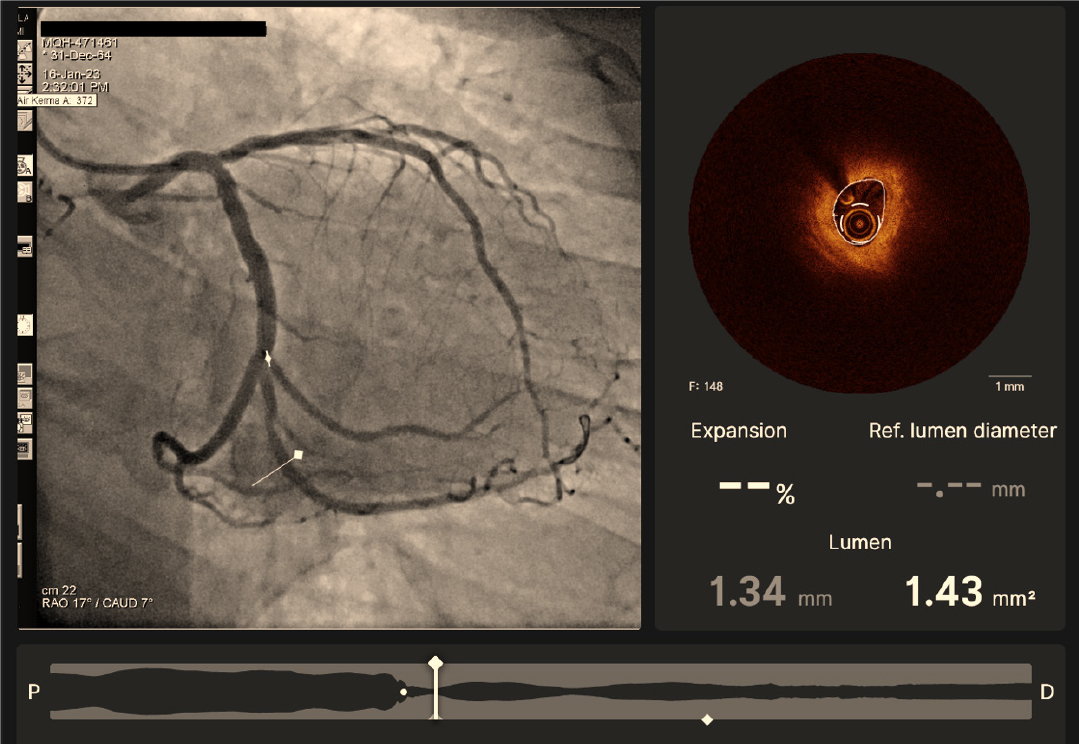
His cardiac ultrasound was normal with preserved ejection fraction, there were no wall motion abnormalities, the heart chambers were of normal dimensions as well as function and appearance of the valves. Coronary angiography showed no signs of restenosis in the left main to Cx stent, mild ostial stenosis/pinching of left anterior descending artery was unchanged to previous procedure, and 2 moderate-to-severe stenoses in the ostio-proximal part of the second obtuse marginal seem slightly tighter (Figure 2A) than 3 years ago. RCA was without signs of stenosis or restenosis. As there was no non-invasive functional testing for evaluation of myocardial ischemia, the decision was made to perform immediately invasive physiologic evaluation of the Cx obtuse marginal artery using Coroventis platform (Coroventis CoroFow Cardiovascular system, Abbot) and pressure wire (PressureWire X, Abbot) for the invasive functional assessment with FFR during hyperemia with i.v. adenosine, resting full-cycle ratio (RFR), coronary flow reserve (CFR) by thermodilution and index of microvascular resistance (IMR) for the assessment of microvascular dysfunction. FFR was preserved with a value of 0.88, RFR was also preserved with a value of 0.90 but CFR was very low (1.2) with a very high IMR of 84 (Figure2B). As there was a discrepancy in functional parameters (FFR preserved, CFR low) pointing out to microvascular dysfunction, OCT imaging (DragonFly OpStar imaging catheter, Abbot) was also applied to evaluate the more detailed anatomical characteristics of the lesion. OCT imaging confirmed the significant fibrotic tandem stenoses but without signs of thin-cup fibroatheroma (Figure 3, co-registration of angiographic and OCT imaging, Ultreon 1.0 software for OCT intravascular imaging, Abbot) or plaque vulnerability.
The diagnosis was that the patient had non-flow limiting coronary stenoses without signs of vulnerable plaque by OCT, and with significantly deteriorated microvascular function according to low coronary CFR and high IMR, which might be clinically defined as microvascular disease producing angina or chest pain syndrome.
As the patient had negative or normal FFR value with no intravascular imaging signs of vulnerable plaque, the revascularization was deferred and the patient was recommended to continue with aspirin and to increase dosage of lipid lowering therapy and add ezetimibe to optimize LDL-cholesterol levels. In addition, due to microvascular dysfunction, as demonstrated with very low CFR and very high IMR, diltiazem and ranolazine were added to his therapy. Gluformine was also added to control diabetes.
His six-month follow-up was uneventful with very rare atypical chest pain episodes.
The optimal diagnostic strategy in patients with diabetes remains controversial and challenging. The previous studies have shown low event rates in asymptomatic patients but also disparities (different cardiovascular risk groups, different non-invasive and invasive testing) in the management and screening of those patients[4]. According to the latest European Society of Cardiology guidelines[5], functional stress testing and computed tomography angiography may be considered and indicated in patients with diabetes as well. On the other hand, earlier studies with stress echocardiography have demonstrated that significantly more patients with diabetes have ischemia on stress testing, and that the prognosis in patients without ischemia is still worse in diabatic than non-diabatic patients[6]. In addition, noninvasively measured (2D echocardiography) CFR provides independent prognostic information in diabetic and non-diabetic patients and negative dipyridamole stress echocardiography - an abnormal CFR is associated with almost twice worse prognoses in diabetic in comparison to non-diabetic patients[7]. Finally, Murthy et al[8] have demonstrated that abnormal CFR by positron emission tomography is independent predictor of cardiac mortality in patients with diabetes and without known coronary artery disease.
Regarding invasive functional testing, Kennedy et al[2] has shown that deferred revascularization in 250 patients according to FFR have been connected with worse outcome in patients with diabetes in comparison to non-diabetic patients, in terms of significant more revascularizations (16% vs 6%) in the mean follow-up time of 40 months. Although earlier studies[9,10] have not shown significant differences in the outcome between diabetic and non-diabetic patients according to FFR values this issue remains controversial. Therefore, COMBINE OCT FFR[3] investigated the impact of OCT-detected thin-cap fibroatheroma (TCFA) on clinical outcomes of patients with diabetes patients with FFR negative lesions. The study[3] revealed that among 550 enrolled diabetic patients with ≥ 1 FFR-negative lesions, TCFA-positive patients represented 25% of this population and were associated with a five-fold higher rate of MACE despite the absence of ischemia as demonstrated by negative FFR > 0.80. This discrepancy between the impact of vulnerable plaque and ischemia on future adverse events may explain worse outcome in diabetic patients with negative FFR. On the other hand, diabetic patients with negative FFR and without TCFA remained to have very low event rate of 3.1% over mean follow-up of 18 months[3]. Still the question remains on the outcome of vulnerable plaques due to the low hard event rates and limited positive predictive value[11]. Regarding therapeutic options, serial intravascular imaging has demonstrated that lipid lowering therapy led to regression of coronary plaque volume and increase in fibroatheroma cup thickness proportional to decrease in cholesterol levels[12].
Our patient presented with anatomically significant but functionally non-significant coronary lesion without signs of plaque vulnerability as shown by thick-cap fibroatheroma, but with significant disturbance of coronary microcirculation as shown by low CFR and very high IMR. The microcirculatory dysfunction may be present in diabetic patients and the cause of positive functional testing and chest pain[13]. In fact, the traditional risk factors may all contribute to coronary microvascular dysfunction and structural remodeling of the microcirculation. In the WISE study[14], chest pain, diabetes, smoking, CAD severity were all independent predictors of hard cardiovascular events. The evaluation of microcirculatory dysfunction has gained a lot of interest in the last years and specific algorithms have been developed to interrogate this clinical condition[15]. Optimal therapy for microcirculatory dysfunction has not been established yet but calcium channel blockers, nebivolol, ranolazine, trimetazidine, ACE inhibitors have been associated with beneficial effects in microvascular angina[15].
The invasive functional evaluation combined with intravascular imaging have complementary diagnostic and prognostic role and therefore a contemporary evaluation of coronary stenosis, particularly in diabetic patients whenever possible and available should include both functional and intravascular imaging data for the best patient management and decision making.
The authors would like to thank research medical nurses Ruwaide Najeeb and chief Cath Lab medical nurse Fadwa el Rawi Ibrahim for their generous support in preparing the manuscript.
| 1. | Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2722] [Cited by in RCA: 4796] [Article Influence: 799.3] [Reference Citation Analysis (0)] |
| 2. | Kennedy MW, Kaplan E, Hermanides RS, Fabris E, Hemradj V, Koopmans PC, Dambrink JH, Marcel Gosselink AT, Van't Hof AW, Ottervanger JP, Roolvink V, Remkes WS, van der Sluis A, Suryapranata H, Kedhi E. Clinical outcomes of deferred revascularisation using fractional flow reserve in patients with and without diabetes mellitus. Cardiovasc Diabetol. 2016;15:100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Kedhi E, Berta B, Roleder T, Hermanides RS, Fabris E, IJsselmuiden AJJ, Kauer F, Alfonso F, von Birgelen C, Escaned J, Camaro C, Kennedy MW, Pereira B, Magro M, Nef H, Reith S, Al Nooryani A, Rivero F, Malinowski K, De Luca G, Garcia Garcia H, Granada JF, Wojakowski W. Thin-cap fibroatheroma predicts clinical events in diabetic patients with normal fractional flow reserve: the COMBINE OCT-FFR trial. Eur Heart J. 2021;42:4671-4679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 213] [Article Influence: 42.6] [Reference Citation Analysis (0)] |
| 4. | Clerc OF, Fuchs TA, Stehli J, Benz DC, Gräni C, Messerli M, Giannopoulos AA, Buechel RR, Lüscher TF, Pazhenkottil AP, Kaufmann PA, Gaemperli O. Non-invasive screening for coronary artery disease in asymptomatic diabetic patients: a systematic review and meta-analysis of randomised controlled trials. Eur Heart J Cardiovasc Imaging. 2018;19:838-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Marx N, Federici M, Schütt K, Müller-Wieland D, Ajjan RA, Antunes MJ, Christodorescu RM, Crawford C, Di Angelantonio E, Eliasson B, Espinola-Klein C, Fauchier L, Halle M, Herrington WG, Kautzky-Willer A, Lambrinou E, Lesiak M, Lettino M, McGuire DK, Mullens W, Rocca B, Sattar N; ESC Scientific Document Group. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J. 2023;44:4043-4140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 999] [Cited by in RCA: 884] [Article Influence: 294.7] [Reference Citation Analysis (0)] |
| 6. | Cortigiani L, Bigi R, Sicari R, Rigo F, Bovenzi F, Picano E. Comparison of prognostic value of pharmacologic stress echocardiography in chest pain patients with versus without diabetes mellitus and positive exercise electrocardiography. Am J Cardiol. 2007;100:1744-1749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Cortigiani L, Rigo F, Gherardi S, Sicari R, Galderisi M, Bovenzi F, Picano E. Additional prognostic value of coronary flow reserve in diabetic and nondiabetic patients with negative dipyridamole stress echocardiography by wall motion criteria. J Am Coll Cardiol. 2007;50:1354-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 129] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Murthy VL, Naya M, Foster CR, Gaber M, Hainer J, Klein J, Dorbala S, Blankstein R, Di Carli MF. Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation. 2012;126:1858-1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 424] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 9. | Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van' t Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG, Ver Lee PN, MacCarthy PA, Fearon WF; FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2974] [Cited by in RCA: 3158] [Article Influence: 185.8] [Reference Citation Analysis (0)] |
| 10. | Domínguez-Franco AJ, Jiménez-Navarro MF, Muñoz-García AJ, Alonso-Briales JH, Hernández-García JM, de Teresa Galván E. [Long-term prognosis in diabetic patients in whom revascularization is deferred following fractional flow reserve assessment]. Rev Esp Cardiol. 2008;61:352-359. [PubMed] |
| 11. | Al-Lamee R, Mintz GS. What are the PROSPECTs and clinical implications of vulnerable plaque? Eur Heart J. 2021;42:4680-4682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 12. | Nissen SE, Nicholls SJ, Sipahi I, Libby P, Raichlen JS, Ballantyne CM, Davignon J, Erbel R, Fruchart JC, Tardif JC, Schoenhagen P, Crowe T, Cain V, Wolski K, Goormastic M, Tuzcu EM; ASTEROID Investigators. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA. 2006;295:1556-1565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1445] [Cited by in RCA: 1524] [Article Influence: 76.2] [Reference Citation Analysis (0)] |
| 13. | Mygind ND, Michelsen MM, Pena A, Frestad D, Dose N, Aziz A, Faber R, Høst N, Gustafsson I, Hansen PR, Hansen HS, Bairey Merz CN, Kastrup J, Prescott E. Coronary Microvascular Function and Cardiovascular Risk Factors in Women With Angina Pectoris and No Obstructive Coronary Artery Disease: The iPOWER Study. J Am Heart Assoc. 2016;5:e003064. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 147] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 14. | Radico F, Zimarino M, Fulgenzi F, Ricci F, Di Nicola M, Jespersen L, Chang SM, Humphries KH, Marzilli M, De Caterina R. Determinants of long-term clinical outcomes in patients with angina but without obstructive coronary artery disease: a systematic review and meta-analysis. Eur Heart J. 2018;39:2135-2146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 125] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 15. | Kunadian V, Chieffo A, Camici PG, Berry C, Escaned J, Maas AHEM, Prescott E, Karam N, Appelman Y, Fraccaro C, Buchanan GL, Manzo-Silberman S, Al-Lamee R, Regar E, Lansky A, Abbott JD, Badimon L, Duncker DJ, Mehran R, Capodanno D, Baumbach A. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. EuroIntervention. 2021;16:1049-1069. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 169] [Cited by in RCA: 152] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United Arab Emirates
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ding H, China S-Editor: Zheng XM L-Editor: A P-Editor: Zhao S