Published online May 6, 2024. doi: 10.12998/wjcc.v12.i13.2263
Peer-review started: December 19, 2023
First decision: January 10, 2024
Revised: January 24, 2024
Accepted: March 26, 2024
Article in press: March 26, 2024
Published online: May 6, 2024
Processing time: 127 Days and 12.9 Hours
There is limited literature on managing the airway of patients with linear im
A 45-year-old African American female presented to our ambulatory surgical center for right corneal transplantation due to corneal perforation after blunt trauma in the setting of cicatricial conjunctivitis and diffuse corneal neovascula
A multidisciplinary approach to treating this disease is the best course of action before a surgical procedure. In our case, key communication between the surgery, anesthesia, and dermatology teams led to the quick and safe treatment of our pa
Core Tip: Linear immunoglobulin A bullous dermatosis, a rare mucocutaneous disorder, can lead to significant airway bleeding due to the presence of friable bullae. Airway emergencies in ambulatory surgical centers can be very high risk. A multidisciplinary discussion of the disease and patient optimization needs to be performed before the day of surgery. These cases should be treated in the inpatient setting where resources are most easily accessible, and an ear, nose, and throat team should be available.
- Citation: Nin OC, Hutnik R, Chheda NN, Hutchinson D. Airway management of a patient with linear immunoglobulin A bullous dermatosis: A case report. World J Clin Cases 2024; 12(13): 2263-2268
- URL: https://www.wjgnet.com/2307-8960/full/v12/i13/2263.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i13.2263
Linear immunoglobulin A (IgA) bullous dermatosis (LABD) is an autoimmune mucocutaneous disease involving dis
Decreased vision in the right eye.
A 45-year-old African American female presented to our ambulatory surgical center for right corneal transplantation due to corneal perforation in the setting of cicatricial conjunctivitis, as well as diffuse corneal neovascularization from LABD. At the time of the surgery, the severity of the disease was unknown. The patient had been lost to follow-up with der
The patient’s medical history consisted of anxiety, depression, chronic benzodiazepine dependence, chronic back pain, hypertension, constipation, genital herpes, prior cocaine abuse, and LABD.
The patient had a strong family history of autoimmune disease, with paternal cousins having sarcoidosis, systemic lupus erythematosus, and multiple sclerosis. The patient was married and lived a few hours away from our hospital location. She was of a lower socioeconomic background and had trouble affording medications for her treatment.
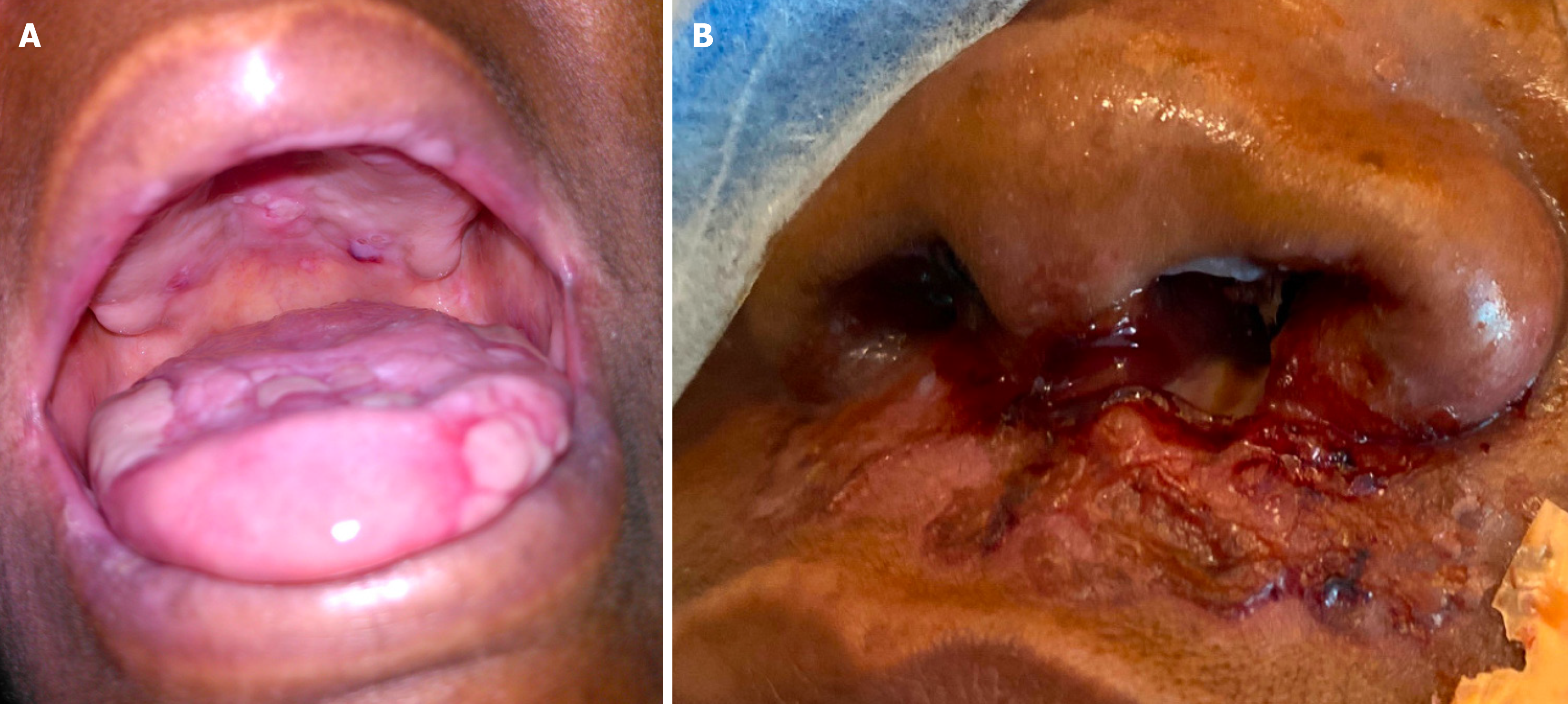
The patient had visible nasal ulcers and some white ulcers on her tongue (Figure 1). There was no history of bleeding in her mouth or of previous anesthetic complications. The rest of the physical exam was normal.
No laboratories were needed for preoperative evaluation before this emergent case.
Figure 1 shows the preoperative oral and nasal lesions.
On August 10, 2021, the patient presented to the free-standing ambulatory surgical center for a corneal transplant of the right eye under general anesthesia. On the day of surgery, an anesthetic preoperative evaluation and a focused physical examination were performed. The patient had visible clear nasal ulcers and white ulcers on her tongue (Figure 1). There was no history of bleeding in her mouth or of previous anesthetic complications. General anesthesia was indicated, given the type of surgery; therefore, airway manipulation was required. The decision was made to intubate using a C-MAC for optimal airway visualization due to the unknown extent of mucosal involvement of her disease, and complete visualization of the oropharynx was desirable. A peripheral intravenous catheter was placed, and 2 mg of intravenous mida
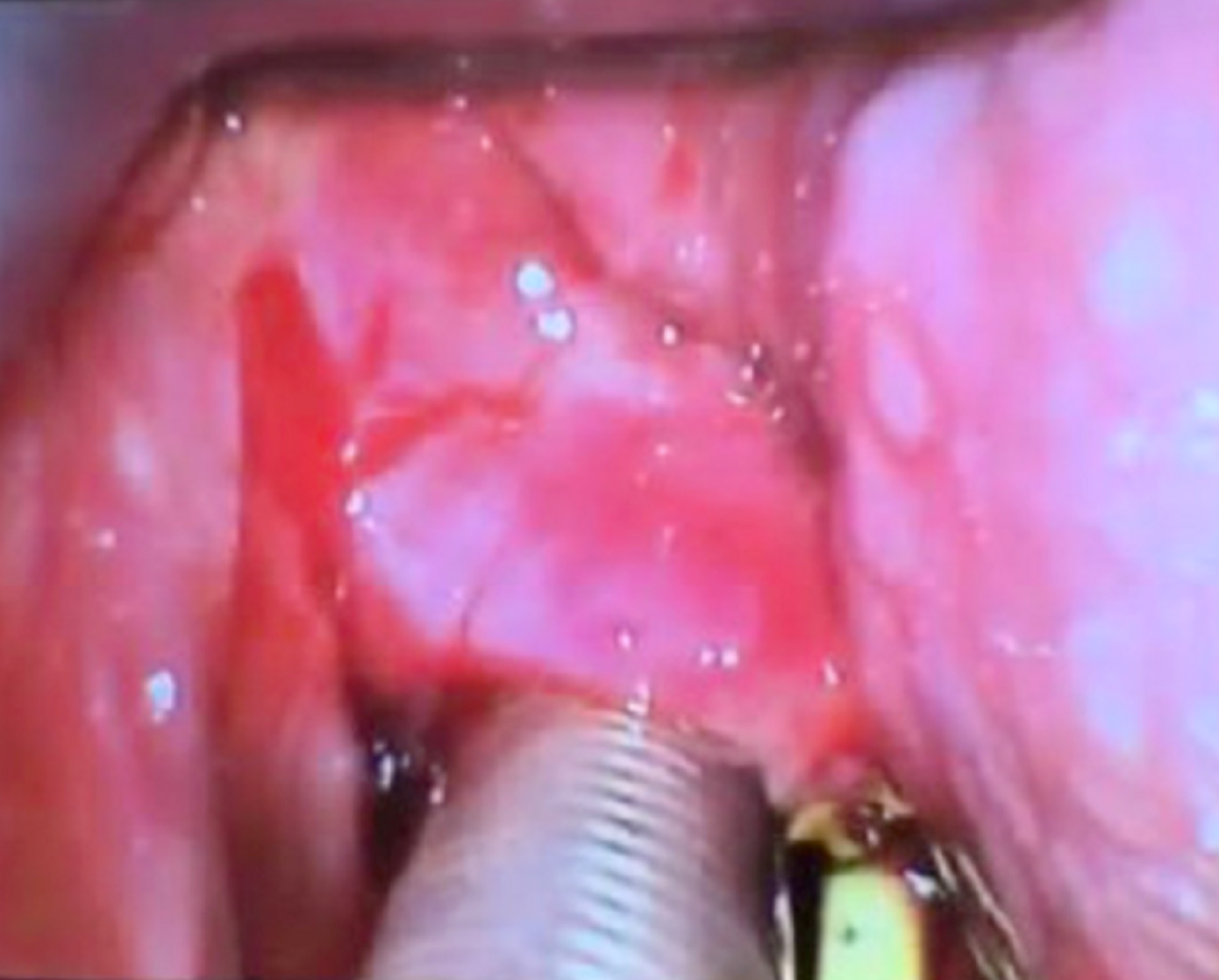
Upon careful placement of the C-MAC Mac 3 blade, ulcerative lesions were observed throughout the oropharynx, epiglottis, and vallecula. There was spontaneous and diffuse bleeding from lesions in the vallecula, even with minimal manipulation, and the airway was quickly secured using a wire-reinforced 7.0 endotracheal tube. A wire-reinforced tube was chosen so the endotracheal tube could be taped to the chin for surgical exposure. The ear, nose, and throat (ENT) team was called to the operating room to evaluate the bleeding, where they performed a visual examination by C-MAC, suctioned, and placed five epinephrine-soaked (0.1 mg/mL) cottonoids in the oropharynx. After a discussion between the ENT and ophthalmology teams, the decision was made to proceed with the surgery and transfer the patient intubated after surgery to our institution’s main hospital surgical intensive care unit under the care of the ENT team. This hospital is located 20 min from our free-standing outpatient facility. Upon successful completion of the surgical procedure, the patient was transferred intubated to the surgical intensive care unit via ambulance.
The patient was transferred in stable condition to the main hospital by ambulance under the direct supervision of the attending anesthesiologist. To assess the extent of the ulcerative lesions before trial extubation, a bedside bronchoscopy was performed that revealed no ulcerative lesions in the trachea or bronchi. Ventilator weaning commenced, and ex
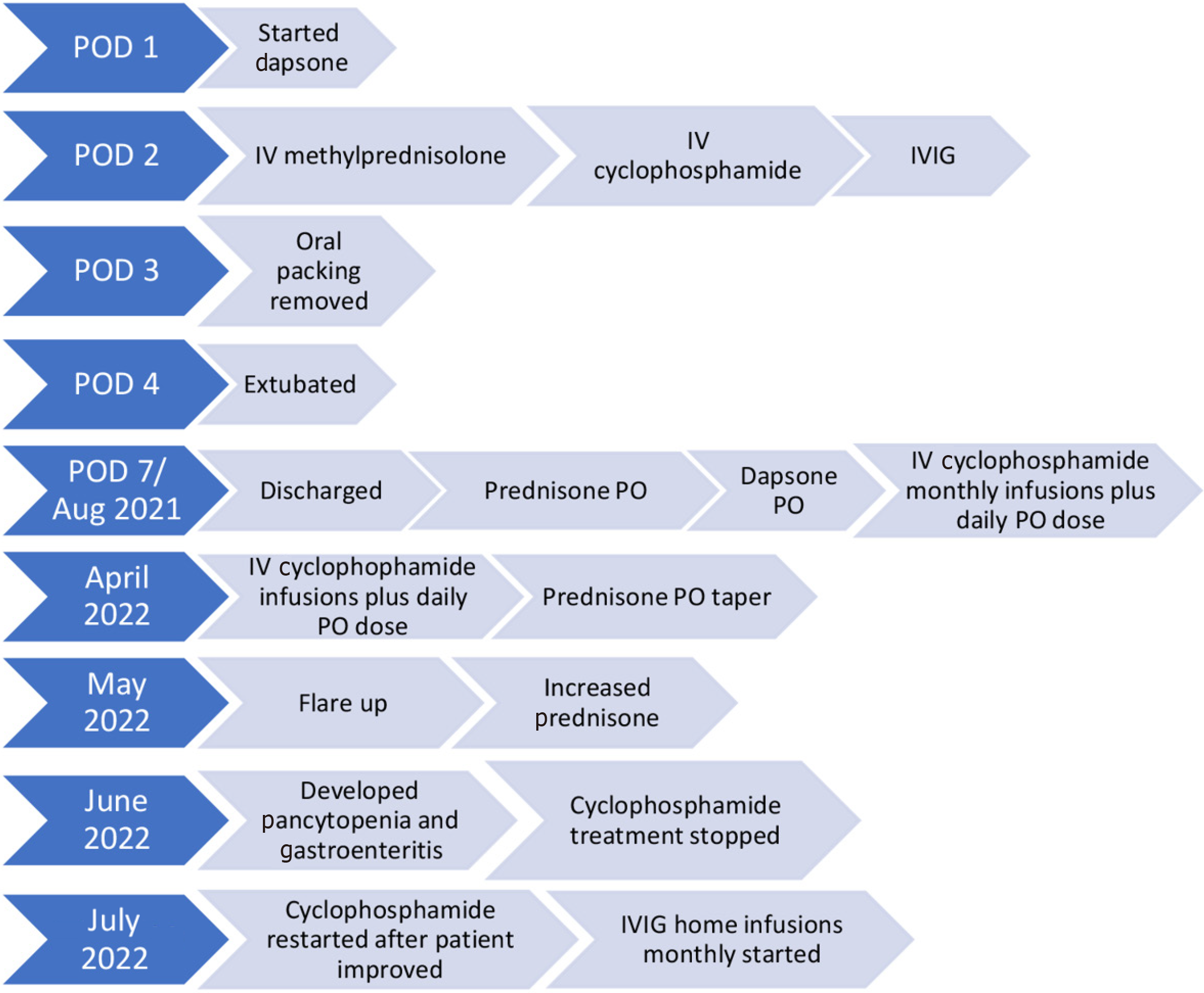
Due to the severity and extent of the disease, the dermatology team re-initiated dapsone therapy and prescribed a course of intravenous methylprednisolone and a single dose of both cyclophosphamide and IVIG. Overnight, the patient was observed to have a few isolated episodes of agitation that resulted in spontaneous bleeding; therefore, the oro
Right corneal perforation due to cicatricial conjunctivitis and diffuse corneal neovascularization from LABD.
Patient was treated with dapsone and a course of prednisone. In the hospital the patient was given a course of intra
The patient continues on monthly cyclophosphamide infusions and daily oral prednisone and dapsone. She is seeing her dermatologist monthly.
LABD is a markedly rare disease, so very few anesthesiologists have experience managing these patients. In Europe, the incidence is approximately 0.1 per million. It presents in a bimodal age distribution: children aged six months to 10 years old (mean age five years old, rarely persisting past puberty) and adults over 60 years old. LABD is typically triggered by infection but can also be drug-induced by exposure to antibiotics (most notably vancomycin), antihypertensives, and nonsteroidal anti-inflammatory drugs. While some LABD presentations are idiopathic, associations with other systemic diseases have been demonstrated, such as ulcerative colitis, systemic lupus erythematosus, and lymphoproliferative disorders. Up to 5% of reported cases of LABD have been associated with lymphoid malignancies including Hodgkin’s or B-cell lymphoma. Idiopathic LABD may persist for decades with episodes of relapse/remission. In our patient, LABD was diagnosed in February 2021 and deemed idiopathic[3].
Diagnosis is confirmed by clinical, histopathological, and immunological data. Treatment varies depending on the degree of severity of disease and the potential inciting event. In suspected drug-induced LABD, removal of the offending medication may result in gradual resolution. The mainstay of treatment in LABD is dapsone (50-150 mg daily in adults), which can begin resolution of lesions within 72 h. Per a collection of case reports, median length of dapsone treatment is 26 mo[4]. Common side effects of dapsone include hemolytic anemia (G6PD deficiency), methemoglobinemia, motor neuropathy, hepatitis, cholestatic jaundice, and hypoalbuminemia. Routine complete blood count, liver function tests, and G6PD levels should be checked while on dapsone therapy. Immunosuppressants (azathioprine, methotrexate, mycophenolate mofetil, and cyclophosphamide) and corticosteroids are other modalities used for treatment. Chronic use of cyclophosphamide can lead to the onset of malignancies, such as bladder cancer[5]. Other treatment options include colchicine, tetracyclines, sulfonamides, nicotinamides, and IVIG.
Dermatology input and medication management were key to improving our patient’s outcome. She continued on dapsone and was also given intravenous methylprednisolone, IVIG, and a dose of cyclophosphamide to treat her mucous membrane lesions and allow for extubation.
For an anesthesiologist caring for patients with LABD, the most critical information needed is the presence of mucous membrane involvement and airway compromise. In the event of airway bleeding with this disease, ENT intervention to control bleeding with epinephrine and tranexamic acid is necessary to protect the airway as medical treatment begins to take effect. Our ambulatory surgical center and the ENT clinics are all in the same building, helping our team initiate treatment quickly.
For our case, the severity and details of the disease were unknown at the time of the surgery. The surgery was em
To our knowledge, this is the first case report of the anesthetic implications of LABD[4] involving the mucous membranes of the nasal cavities and oropharynx. Given the lack of information on this disease and its extent in this patient, our anesthesia team was unaware of the lesions we would encounter throughout both the oropharynx and hypopharynx. Upon intubation, we understood the extent of the lesions and their friability. In retrospect, we should have consulted the ENT team preoperatively for a preoperative nasopharyngoscopy to determine the extent of the lesions. Had the patient attended her preoperative clinic appointment, our team may have had more information available.
A multidisciplinary approach to treating this disease is the best course of action before a surgical procedure. Ambu
This manuscript was prepared in compliance with the Health Insurance Portability and Accountability Act (HIPAA) of 1996 privacy regulations and adheres to applicable Enhancing the Quality and Transparency of Health Research gui
Learning points: (1) Mucous lesions in the oropharynx and hypopharynx can be extremely friable and cause bleeding upon minimal manipulation; (2) Early dermatology intervention and medication administration is key to a quick recovery from an acute exacerbation; and (3) Proper planning of operating room intervention in a hospital setting is vital to mitigate potential airway complications. These cases should not be done in an ambulatory setting.
The authors thank Bryan Penberthy, MFA, of the University of Florida College of Medicine Department of Anesthe
| 1. | Chen S, Mattei P, Fischer M, Gay JD, Milner SM, Price LA. Linear IgA bullous dermatosis. Eplasty. 2013;13:ic49. [PubMed] |
| 2. | Guide SV, Marinkovich MP. Linear IgA bullous dermatosis. Clin Dermatol. 2001;19:719-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 89] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Lammer J, Hein R, Roenneberg S, Biedermann T, Volz T. Drug-induced linear IgA bullous dermatosis: a case report and review of the literature. Acta Derm Venereol. 2019;99:508-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 4. | Lings K, Bygum A. Linear IgA bullous dermatosis: a retrospective study of 23 patients in Denmark. Acta Derm Venereol. 2015;95:466-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Vale ECSD, Dimatos OC, Porro AM, Santi CG. Consensus on the treatment of autoimmune bullous dermatoses: dermatitis herpetiformis and linear IgA bullous dermatosis - Brazilian Society of Dermatology. An Bras Dermatol. 2019;94:48-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Esch M, Germany S-Editor: Liu JH L-Editor: A P-Editor: Xu ZH