Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.4991
Peer-review started: November 8, 2021
First decision: February 7, 2022
Revised: March 3, 2022
Accepted: March 25, 2022
Article in press: March 25, 2022
Published online: May 26, 2022
Processing time: 197 Days and 10.2 Hours
Paraganglioma occurring at the lateral skull base is a rare tumor. Surgery is the primary treatment of benign paragangliomas. Postoperative infection of the surgical site at the lateral skull base is very dangerous and hard to manage.
A 30-year-old man with a 1-year history of left-side progressive hearing loss, tinnitus, facial palsy, and choking failed conventional treatment and is the focus of this case report. Imaging revealed a mass around the left jugular foramen that was approximately 47 mm × 38 mm × 34 mm in size and had eroded the bone of the vertebral and horizontal segments of the internal carotid artery. The tumor breached the meninges and occupied the cerebella pontine region. A two-stage surgery was designed for the resection of the mass. In the first-stage, the epidural portion of the mass was removed. The abdominal fat and the temporal muscle flap were transposed within the surgical site. The surgery was successful; however, 25 d after surgery, he developed suppurative parotitis, and the infection spread to the surgical site at the skull base. Broad-spectrum antibiotics were used, and debridement was deployed. After that, the wound was cleaned daily. Five months after the first-stage surgery, the wound was still unclosed, and there was intermittent purulent exudation within the surgical site. vacuum sealing drainage (VSD) was used, and the wound healed in a month. One year after the first surgery, the second-stage of the operation was performed to remove the intracranial portion of the tumor. Recurrence of the tumor was not detected after a 6-month follow-up.
After a lateral skull base surgery, suppurative parotitis can spread into the operative cavity leading to infection of the surgical site. VSD can help to effectively heal the infected wound. A two-stage surgical approach offers a safer option for removing the lateral skull base paraganglioma that involves the meninges.
Core Tip: This is a case report of a 30-year-old male patient with a left jugular foramen paraganglioma who underwent first-stage surgical resection of the epidural portion of the tumor. On postoperative day 25, he developed fever, swelling, and tenderness under the left ear. Investigation and retrospective analyses revealed an infection of the skull base surgical site caused by pseudomonas aeruginosa, due to postoperative suppurative parotitis. The infection was successfully treated with vacuum sealing drainage and antibiotic therapy. The second-stage operation took place 6 mo later, and tumor recurrence was not detected after a 6-month follow-up.
- Citation: Zhao Y, Zhao Y, Zhang LQ, Feng GD. Postoperative infection of the skull base surgical site due to suppurative parotitis: A case report. World J Clin Cases 2022; 10(15): 4991-4997
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/4991.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.4991
Paragangliomas are a rare neuroendocrine tumor of the autonomic nervous system[1]. The diagnosis depends on pathology findings. Malignant paragangliomas are diagnosed based on the presence of distant metastasis. It is reported that benign paragangliomas account for 76.1% of the total number of paragangliomas[2]. For benign paragangliomas, surgical resection is currently the only possible cure for the disease[3].
Attention should be paid to postoperative infection of the lateral skull base surgical site. Once infection occurs, the transplanted tissue may become necrotic, the length of hospital stay increases significantly, and the time of postoperative adjuvant treatment may be delayed. In the case of meningitis or encephalitis, patients are in life-threatening danger[4]. Incomplete filling of the cavity defect, poor localized blood supply of the free tissue flap, and a postradiotherapy state are all risk factors of postoperative infection at the surgical site of the lateral skull base[5]. Suppurative parotitis can be a complication of general anesthesia surgery and has an incidence rate of 1 in every 1000 postoperative cases[6]. Predisposing factors of suppurative parotitis are dehydration, malnutrition, oral neoplasms, immunodeficiency, sialolithiasis, and medications that diminish salivation[7].
Herein, we report a patient presenting with a paraganglioma of the lateral skull base that was surgically treated, followed by postoperative surgical site infection due to suppurative parotitis. We need to be alert to the emergence of postoperative suppurative parotitis, find the inflammation evidence in the adjacent area of the surgical site as soon as possible, and prevent it from spreading, which could result in adverse consequences for patients. Vacuum sealing drainage (VSD) is worth considering for such complicated postoperative infections of the lateral skull base.
A 30-year-old male patient with a 1-year history of left-side tinnitus.
The patient had 1-year of persistent tinnitus and 5 mo of hearing loss on the left side. He developed progressive facial paralysis on the left side, accompanied by hoarseness, left tongue extension, choking while drinking, and occasional difficulty swallowing. Contrast-enhanced magnetic resonance imaging (MRI) of the head revealed a mass surrounding the jugular foramen.
The patient had no systematic diseases, and no significant personal and family history.
The patient had no systematic diseases, and no significant personal and family history.
He presented with a swollen external auditory canal containing a dark red mass within the tympanic cavity that pulsated in sync with his pulse rate, facial (House-Brackmann IV grade), glossopharyngeal, and vagal palsy, as well as hearing loss. All the symptoms above appeared on his left side.
The blood serum levels of norepinephrine were 84.86 μg/24 h (normal reference ≤ 40.65 μg/24 h) and all serum inflammatory biomarkers were normal.
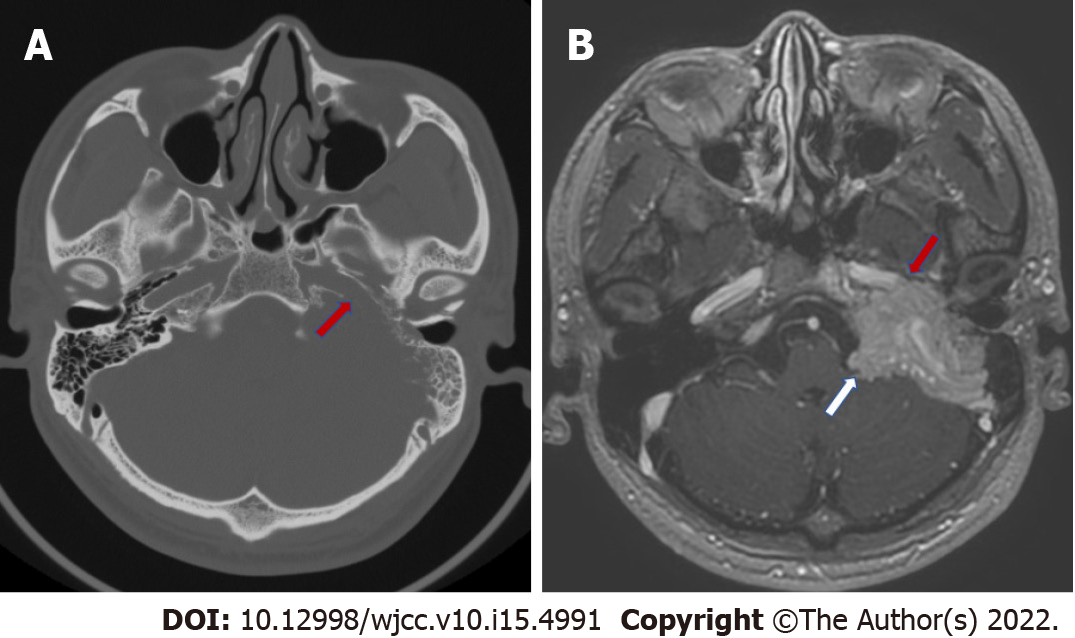
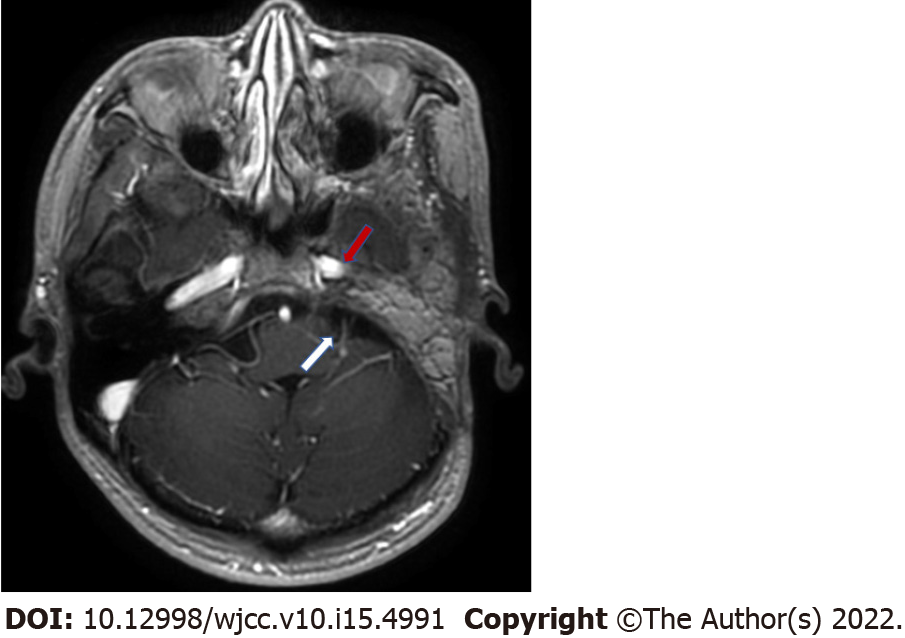
Computed tomography (CT) of the temporal bone showed bone destruction of the left jugular foramen and the horizontal segment of the internal carotid artery (Figure 1A). Enhanced MRI of the temporal bone showed an uneven enhanced mass with a size of 47 mm × 38 mm × 34 mm involving the left jugular foramen, which partially wrapped around the internal carotid artery and extended to the cerebellar pontine region with invasion within the meninges (Figure 1B).
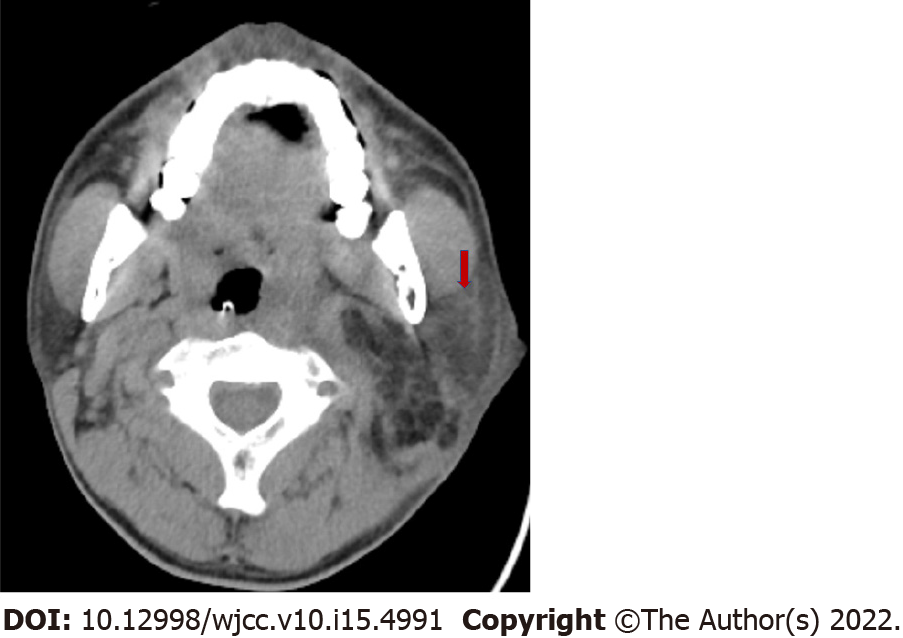
According to the patient's medical history, and physical examination results, the tumor is likely a paraganglioma. A two-stage surgery was designed for the resection of the mass. The patient underwent first-stage surgery to remove the extradural portion of the tumor. The pathological findings suggested a paraganglioma. Furthermore, the abdominal fat and the temporal flap were transposed in order to fill the cavities deficit. The surgery was successful. The patient received an intravenous infusion of ceftriaxone (2 g qd) for 7 d after surgery and was replaced with ceftazidime (1 g q12h) due to elevated blood transaminase. After the replacement, the antibiotics were continued for 2 wk until the inflammatory biomarkers returned to normal and then therapy was stopped. However, 25 d post-surgery, the patient suddenly developed swelling and tenderness under his left ear, with his body temperature reaching 40.5℃. A yellow purulent secretion appeared on the left buccal mucosa, followed by ulceration of the swollen area under the left ear. Laboratory examination indicated a 15.12 × 109/L total white blood cell count (normal reference ≤ 9.5 × 109/L) and a neutral granule percentage of 83.1% (normal reference ≤ 75%). Neck CT showed a hypodensity shadow in the caudal lobe of the left parotid gland (Figure 2). The diagnosis of suppurative parotitis was confirmed, and ceftazidime was given intravenously (2 g q8h) for 9 d. The swelling and tenderness in the parotid gland area gradually subsided, and no abnormalities were found within the surgical incision. However, the skin under the left ear ruptured and yellow fluid was discharged. Liquefaction necrosis occurred within the transposed abdominal fat of the skull base surgical site. Bacterial culture revealed a pseudomonas aeruginosa infection. According to the time sequence of suppurative parotitis and liquefaction necrosis, the infection of the surgical site was considered to be caused by suppurative parotitis.
Postoperative infection of the skull base surgical site, with pseudomonas aeruginosa.
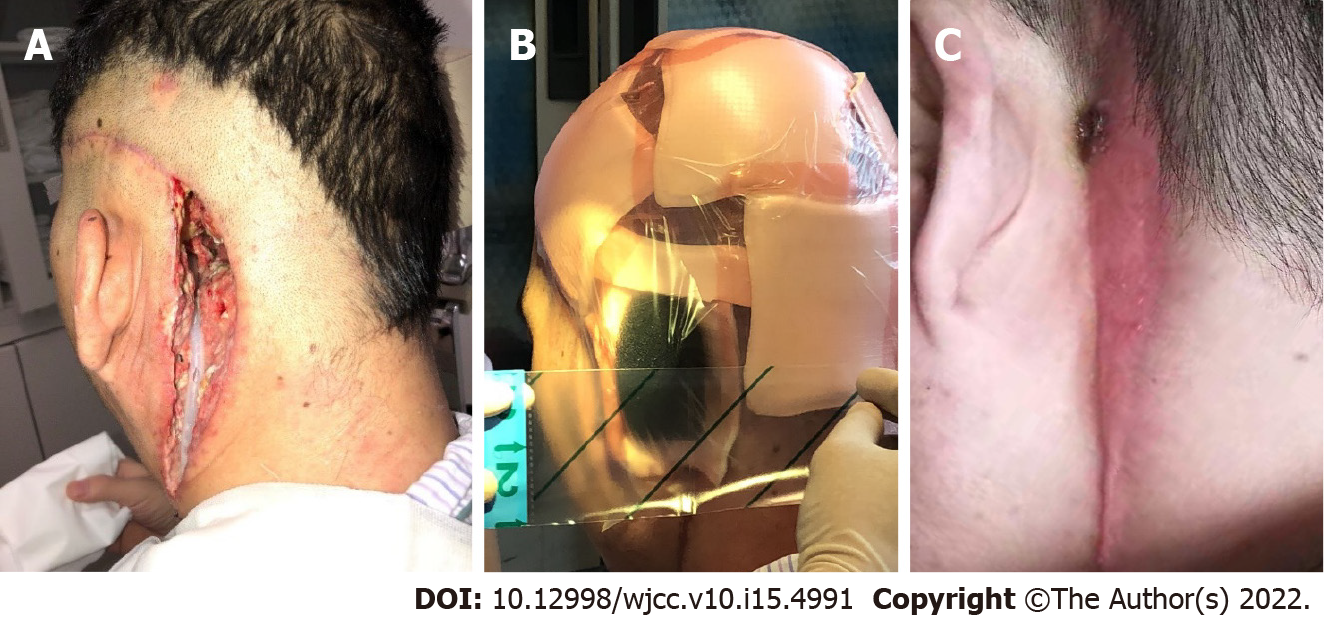
Debridement was performed, the wound was kept clean, and received daily wound dressing changes (Figure 3A). Broad-spectrum antibiotics were used for infection control. The antibiotic regimen initially included ceftazidime (1 g q8h) and metronidazole (0.5 g bid) intravenous drips. During the dressing changes, bacteria culture and drug sensitivity tests were performed. Pseudomonas aeruginosa was cultivated intermittently, and ciprofloxacin (0.4 g qd) was replaced according to the drug sensitivity test. After the serum inflammatory biomarkers returned to normal, there were no other abnormalities except for a small amount of purulent exudation when changing the wound dressing. An infectious disease physician evaluated the advantages and disadvantages of continuous use of systemic antibiotics and considered that continually antibiotic therapy might not further effectively control the infection; however, might lead to the emergence of antibiotic resistant bacteria. The appropriate method to promote local wound healing should be continuous dressing changes and adequate drainage. The antibiotics were stopped, and the duration of systemic antibiotic usage after debridement was 3 wk.
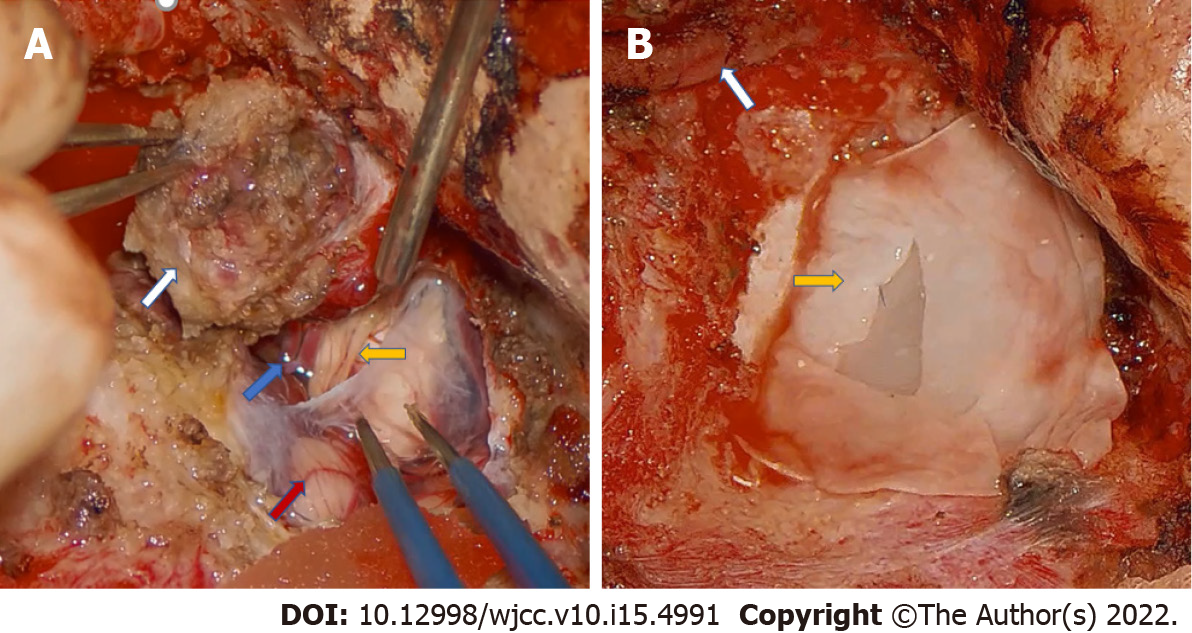
Half a year later, the residual cavity remained at a size of 4 cm x 3 cm x 5 cm. The cavity could not be reduced further and there was intermittent purulent exudation within the surgical site. VSD was chosen to control wound infection. With one month of persistent VSD, the wound eventually healed (Figure 3C). One year after the first operation, he underwent the second-stage operation to remove the intracranial portion of the tumor. The tumor that invaded the meninges was resected (Figure 4A), and artificial dura mater was used to repair the meninges of the posterior fossa (Figure 4B). The abdominal fat and the temporal muscle flap were transposed to the lateral skull base deficit.
The operation wound healed without infection. There were no signs of infection or tumor recurrence on MRI at 6 mo after the second-stage surgery (Figure 5).
Postoperative parotitis is rare and is detrimental to a patient's recovery[9]. Due to the close relationship between the parotid gland and the surgical site at the skull base, once suppurative parotitis occurs, the inflammation may spread to the operative area where the transposed free fat tissue can become infected or necrotic. Once the fat becomes necrotic, the affected tissue should be removed and the wound opened for adequate drainage. In severe cases, meningitis and even encephalitis are possible and are life-threatening[4]. Through the review of this case, the occurrence of suppurative parotitis 25 d after surgery may be related to insufficient oral food intake and decreased parotid gland secretion[9]. It is necessary to pay attention to the patient's oral intake after surgery; therefore, timely intervention is needed if there is insufficient food intake.
The two stage-surgery strategy is safe for large paragangliomas within the skull base which may induce significant meningeal defects. During the first-stage surgery, the extradural portion of the tumor needs to be removed and the surgical site deficit needs to be filled with the pedicled tissue flap or abdominal fat. After the transposed tissue survives, the residual tumor can be safely removed during the second-stage operation. The two stage-surgical strategy has some obvious advantages. First, when dealing with the epidural portion of the tumor, the meninges remain intact. Even if the surgical site gets infected, the probability of meningitis or encephalitis is low. Second, once the surgery is divided into two stages the local blood supply becomes relatively rich when the transposed tissue survives and becomes significantly more favorable for the growth of the repaired meninges after the second stage-surgery. Third, structure of the lateral skull base region is so complex that the operation often has an extended duration of up to more than 20 h. If the operation is divided into two parts, it can avoid excessive fatigue of the doctors and is safer for the patients. In addition, the removal of the epidural portion might induce a tumor reduction effect[8]. When the extracranial region has been resected, the portion of the tumor that protrudes inwards into the meninges may retract outwards. This can help reduce brain damage and leads to an increased distance between the tumor and brain stem or other vital structures, improving the safety of the second-stage surgery.
VSD, proposed by Fleischmann et al[10], is a highly effective treatment for wound drainage. The combination of saline irrigation and negative pressure suction promotes the discharge of wound exudation and healing. Compared with traditional dressing changes, the VSD flushing area is larger, the drainage effect is more significant, the infection control period is shorter, and the local blood circulation is improved[11,12], which is conducive to the growth of granulation tissue.
Given the rarity of this condition, the unforgettable setbacks we experienced, and the lessons we learned, we consider this case report clinically significant.
After a lateral skull base surgery, suppurative parotitis can spread into the operative cavity leading to infection of the surgical site. VSD can help to effectively heal the infected wound. A two-stage surgical approach offers a safer option for removing the lateral skull base paraganglioma that involves the meninges.
| 1. | Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet. 2005;366:665-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1154] [Cited by in RCA: 1172] [Article Influence: 55.8] [Reference Citation Analysis (0)] |
| 2. | Pasini B, Stratakis CA. SDH mutations in tumorigenesis and inherited endocrine tumours: lesson from the phaeochromocytoma-paraganglioma syndromes. J Intern Med. 2009;266:19-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 229] [Cited by in RCA: 194] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 3. | Neumann HPH, Young WF Jr, Eng C. Pheochromocytoma and Paraganglioma. N Engl J Med. 2019;381:552-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 442] [Article Influence: 63.1] [Reference Citation Analysis (0)] |
| 4. | Grigoryan YA, Onopchenko CV. Persistent trigeminal neuralgia after removal of contralateral posterior cranial fossa tumor. Report of two cases. Surg Neurol. 1999;52:56-60; discussion 60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Nishizawa S, Yokota N, Yokoyama T, Mukodaka H, Watanabe T, Hoshino T, Ueda Y. Prevention of postoperative complications in skull base surgery for nasal or paranasal sinus carcinoma invading the skull base. J Clin Neurosci. 2001;8 Suppl 1:67-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Lary BG. Postoperative Suppurative Parotitis. Arch Surg. 1964;89:653-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Brook I. Diagnosis and management of parotitis. Arch Otolaryngol Head Neck Surg. 1992;118:469-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 43] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Nakase H, Ohnishi H, Matsuyama T, Morimoto T, Sakaki T. Two-stage skull base surgery for tumours extending to the sub- and epidural spaces. Acta Neurochir (Wien). 1998;140:891-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Belczak SQ, Cleva RD, Utiyama EM, Cecconello I, Rasslan S, Parreira JG. Acute postsurgical suppurative parotitis: current prevalence at Hospital das Clínicas, São Paulo University Medical School. Rev Inst Med Trop Sao Paulo. 2008;50:303-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Fleischmann W, Strecker W, Bombelli M, Kinzl L. [Vacuum sealing as treatment of soft tissue damage in open fractures]. Unfallchirurg. 1993;96:488-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 87] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Huang Q, Wang JT, Gu HC, Cao G, Cao JC. Comparison of Vacuum Sealing Drainage and Traditional Therapy for Treatment of Diabetic Foot Ulcers: A Meta-Analysis. J Foot Ankle Surg. 2019;58:954-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Petzina R, Gustafsson L, Mokhtari A, Ingemansson R, Malmsjö M. Effect of vacuum-assisted closure on blood flow in the peristernal thoracic wall after internal mammary artery harvesting. Eur J Cardiothorac Surg. 2006;30:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Otorhinolaryngology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chrcanovic BR, Sweden; Gupta SK, India; Syahputra DA, Indonesia S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ