Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.4998
Peer-review started: November 6, 2021
First decision: February 7, 2022
Revised: February 19, 2022
Accepted: March 27, 2022
Article in press: March 27, 2022
Published online: May 26, 2022
Processing time: 199 Days and 5.4 Hours
Blunt aortic injury is a special type of aortic disease. Due to its low incidence, high prehospital mortality and high probability of leakage diagnosis, the timely identification of patients with blunt aortic injury who survive the initial injury has always been a clinical challenge.
We report a case of traumatic aortic pseudoaneurysm with right iliac artery dissection aneurysm that was diagnosed 3 mo after a traffic accident. The patient is a 76-year-old male who was knocked down by a fast-moving four-wheel motor vehicle while crossing the road (the damage mechanism was side impact). He received chest, cranial computed tomography (CT) and whole abdomen enhanced CT in the local hospital. The images suggested subarachnoid hemorrhage, right frontoparietal scalp hematoma, fracture of the right clavicle and second rib, lump-shaped mediastinal shadow outside the anterior descending thoracic aorta (mediastinal hematoma), mesenteric vascular injury with hematoma formation, pelvic fracture, and subluxation of the left sacroiliac joint. After the pelvic fracture was fixed with an external stent, he was sent to our hospital for further treatment. In our hospital, he successfully underwent partial resection of the small intestine and CT-guided screw internal fixation of the left sacroiliac joint and returned to the local hospital for rehabilitation treatment. However, since the accident, the patient has been suffering from mild chest pain, which has not aroused the attention of clinicians. During rehabilitation, his chest pain gradually worsened, and the thoracic aorta computed tomography angiography performed in the local hospital showed a pseudoaneurysm in the initial descending segment of the aortic arch. After transfer to our hospital, a dissecting aneurysm of the right external iliac artery was incidentally found in the preoperative evaluation. Finally, endovascular stent graft repair was performed, and he was discharged on the 10th day after the operation. No obvious endo-leak was found after 4 years of follow-up.
We highlight that emergency trauma centers should consider the possibility of aortic injury in patients with severe motor vehicle crashes and repeat the examination when necessary to avoid missed diagnoses.
Core Tip: The era of high-speed motor vehicles has brought an increase in the incidence of blunt aortic injury, and the high mortality rate from traumatic aortic injury points toward vigilance. We report a 76-year-old man who was diagnosed with traumatic aortic pseudoaneurysm with right iliac artery dissection aneurysm 3 mo after severe trauma due to mild chest pain that gradually worsened. After interventional surgery, resolution of symptoms was observed, and there were no long-term complications. The aim of our case report is to alert clinicians to identify aortic injuries in light of history and diagnosing symptoms for proper treatment and the prevention of complications and mortality.
- Citation: Fang XX, Wu XH, Chen XF. Blunt aortic injury–traumatic aortic isthmus pseudoaneurysm with right iliac artery dissection aneurysm: A case report. World J Clin Cases 2022; 10(15): 4998-5004
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/4998.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.4998
Blunt aortic injury occurs in less than 1% of motor vehicle crashes but is responsible for 16% of deaths[1], and up to 80% of patients die before they arrive at the hospital. Of those who survive the initial injury, a majority die without definitive diagnosis[1,2] but are found and reported at autopsy. Approximately 15% of individuals with traumatic aortic rupture survive temporarily, and 90% die within four months[3,4]. A traumatic pseudoaneurysm is formed in survivors[4]. The natural course from aortic rupture to pseudoaneurysm formation with secondary rupture of the aneurysm may be brief or can extend over many years[2]. Clinical presentations of pseudoaneurysms include local mass, severe chest pain, myocardial ischemia, and heart failure secondary to valvular regurgitation or cardiac compression. The diagnosis of pseudoaneurysms with typical clinical manifestations is relatively easy, but nonobvious symptoms of pseudoaneurysms are prone to misdiagnosis or are missed[5]. For patients who survive the initial injury, rapid detection and diagnosis are critical.
A 76-year-old man transferred from the local hospital complained of chest pain after trauma for 3 mo that had been aggravated for half a month.
He had a history of a motor vehicle collision 3 mo prior to this admission. Continuous mild chest pain since he had been injured. After positive treatment in our hospital, he was transferred to the local hospital for rehabilitation treatment. Half a month ago, without obvious inducement, his chest pain was transiently aggravated, radiated to the back and was accompanied by chest tightness, which lasted approximately 20 min but resolved on its own. This emergency did not attract the attention of clinicians, and the clinicians did not pursue further diagnostics and treatments. Then, the same symptoms occurred again 5 d before admission. The local hospital performed thoracic aorta computed tomography angiography (CTA) and found that the CTA suggested a pseudoaneurysm in the initial descending segment of the aortic arch. For further treatment, the man was transferred to our hospital.
The patient had been diagnosed with diabetes for 2 years and hyperlipidemia for 10 years before this admission. Three months ago, he underwent partial resection of the small intestine and CT-guided screw fixation of the left sacroiliac joint after the trauma.
He had a smoking history of 40 years, he smoked approximately 10 cigarettes a day, and he quit smoking more than 10 years prior to admission. He denied a history of alcohol consumption and any relevant family history.
He had a blood pressure of 161/75 mmHg, with a pulse rate of 79 beats per minute (bpm). He had clear lungs and normal heart sounds. Abdominal tenderness and rebound tenderness were not detected. All peripheral pulses were present, and no carotid or subclavian bruit was observed.
The laboratory results showed normal routine laboratory parameters and normal blood biochemistry, and the patient’s troponin T (TnT), troponin I (TnI), myocardial enzymes, thrombin time (TT), prothrombin time (PT), activated partial thromboplastin time (APTT), fibrinogen (FIB), thromboela-stogram (TEG), tumor abnormal protein (TAP), C-reactive protein (CRP), and procalcitonin (PCT) were all normal. An ECG suggested sinus bradycardia, and the patient’s heart rate was 57 beats per minute.
When thoracic and abdominal aorta CTA were used to evaluate the pseudoaneurysm in the initial descending segment of the aortic arch, a dissecting aneurysm of the right external iliac artery was unexpectedly found.
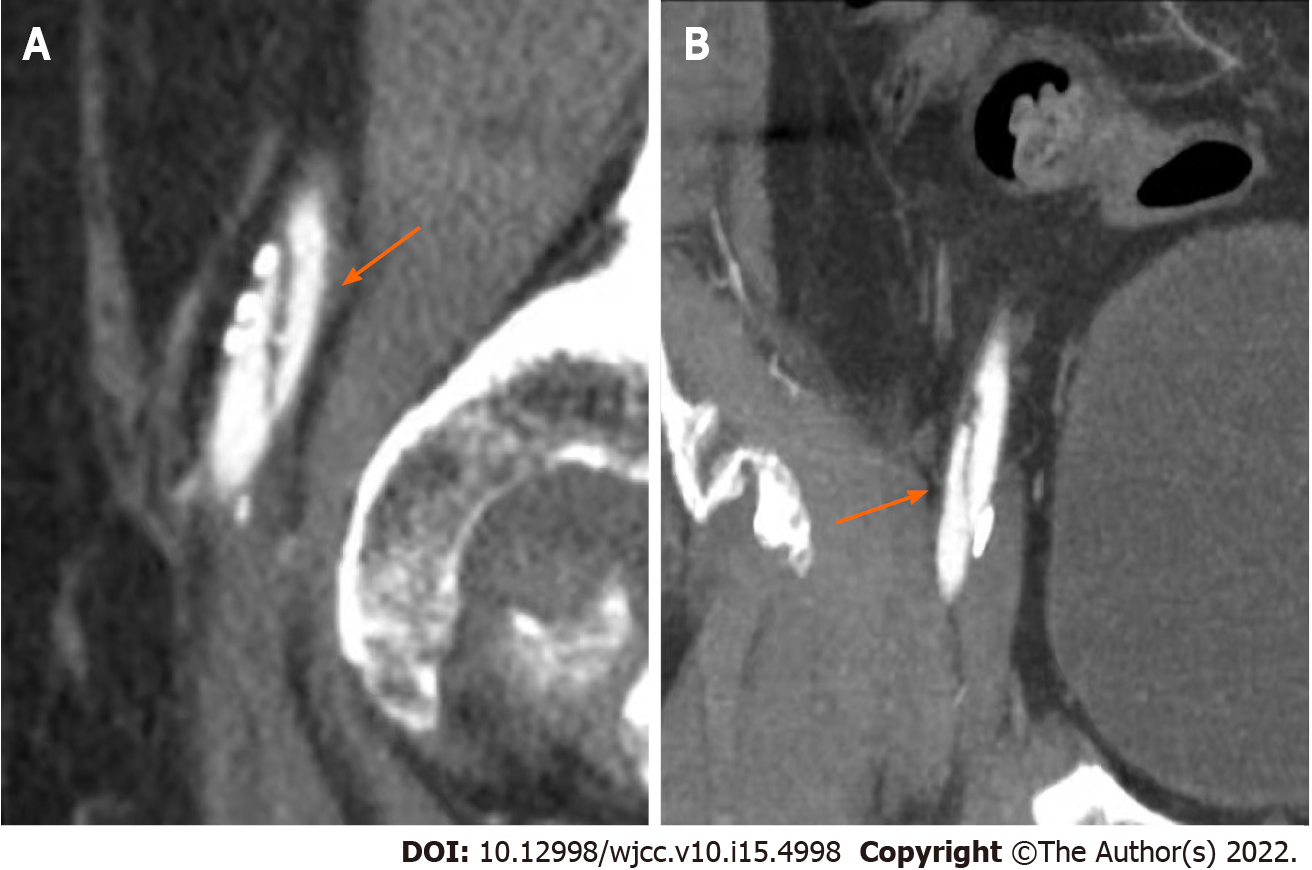
The former thoracic and abdominal aorta CTA images showed sagittal and transverse views of the traumatic aortic isthmus pseudoaneurysm. On the sagittal view (Figure 1A), bulging of the anterior wall of the aortic isthmus was observed. The base was approximately 1.1 cm wide, and the protruding height was approximately 1.5 cm. In the transverse view (Figure 1B), the lumen of the aorta, the crevasse, and the false lumen of this dissection vessel were observed.
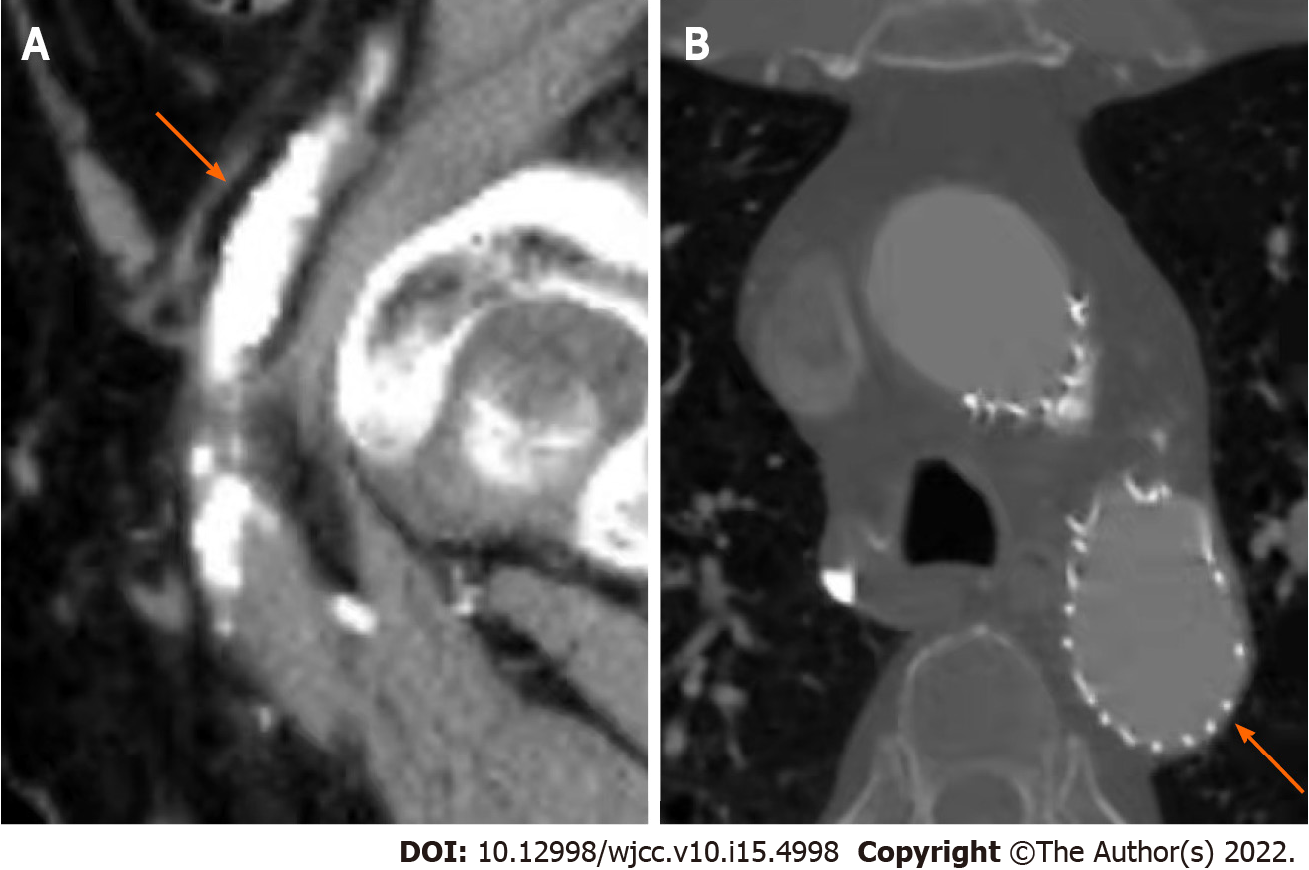
The latter thoracic and abdominal aorta CTA images showed sagittal and coronal views (Figure 2) of the dissecting aneurysm of the right external iliac artery, and a double-lumen structure was observed.
The final diagnosis of this case was a traumatic aortic pseudoaneurysm and a traumatic right iliac artery dissection aneurysm.
No obvious contraindications were found in the patient's preoperative auxiliary examination. With the informed consent of his family, endo-vascular stent graft repair was performed in the operating room. Half an hour before the operation, cefuroxime (1.5 g iv drip) was used once to prevent infection. The operation process was smooth. After the operation, a cefuroxime injection (1.5 g iv drip bid) was given for prophylactic anti-infection treatment.
On the first day after the operation, the patient had a fever, the patient’s highest temperature was 38.1 °C, his routine blood examinations were rechecked, his PCT and CRP were high, indicating a reaction after stent implantation, and his antibiotics were not adjusted. He still had a fever on the third day after the operation, and his highest temperature was 38.0 °C. Considering the possibility of infection after stent implantation, piperacillin sodium and tazobactam sodium 4.5 g IVGTT bid were used to strengthen the anti-infective treatment. After that, his fever symptoms were controlled, and the inflammatory indexes gradually decreased to normal. The patient was discharged on the 10th postoperative day and received long-term antiplatelet therapy. After 4 years, the follow-up CTA showed that the covered stent was well formed, and no obvious endo-leak was found (Figure 3).
Blunt aortic injury is a rare but fatal condition associated with motor vehicle collisions, and there are multiple mechanisms involved with blunt aortic injuries. Despite the improved safety measures designed to minimize the occurrence of aortic injuries, the incidence of blunt aortic injury in fatal motor vehicle crashes has not decreased during the past decades[6].
Only 2% to 5% of aortic injuries develop into partial aneurysms or aortic pseudoaneurysms. More than 90% of aortic pseudoaneurysms involve the aortic isthmus[7-9]. Deceleration injury is the most common type of trauma, and the most commonly quoted cause is the differential forces that occur within the chest by deceleration in either the horizontal or vertical plane. The descending aorta remains fixed to the posterior chest wall, while the heart and ascending aorta swing forward and tear at the isthmus[5,10-12].
Clinical presentations of pseudoaneurysms include the presence of a local mass, severe chest pain, myocardial ischemia, and heart failure secondary to valvular regurgitation or cardiac compression[5]. The mortality of aortic pseudoaneurysms is historically more than 95% if the injury is left untreated[13].
The patient we reported here had a deceleration injury from a motor vehicle collision and was admitted to the hospital 3 mo later due to continuous mild but transient aggravation of chest pain. The imaging examinations found pseudoaneurysm of the aortic isthmus, which was logical from the perspective of the course of blunt aortic injury. The patient's first visit to our hospital was 3 mo prior, and the patient complained of pain in multiple parts of his body after his trauma, especially in his abdomen and pelvis. Since his chief complaint was associated with nonthoracic symptoms and since routine screening plain chest radiography in the emergency department showed no obvious aortic injury, pseudoaneurysm or mediastinal abnormality, thoracic aortic CTA was not performed to evaluate whether a potential aortic vascular injury had occurred at that time.
According to Downing’s report[14], after reviewing 54 cases of thoracic aortic injury, all of the patients had other serious injuries-17% were neurological, 60% were abdominal, 35% were pelvic fractures, and 65% consisted of fractures that were elsewhere.
Our clinicians ignored the possibility of a chest injury due to excessive attention to the other injuries in the patient and because the patient had no signs of aortic injury on plain chest radiography. Even if the patient had persistently mild chest pain, no further imaging examinations, such as CTA or magnetic resonance imaging, had ruled out the possibility of blunt aortic injury. Finally, the intermittent aggravation of chest pain aroused the attention of clinicians, and a traumatic aortic isthmus pseudoaneurysm was found by thoracic CTA imaging. Preoperative thoracic and abdominal aorta CTA was used to evaluate the vascular condition, which accidentally found a right iliac artery dissection aneurysm, which was speculated to be caused by the extrusion effect of the motor vehicle collision. According to the Society for Vascular Surgery clinical practice guidelines for the management of blunt aortic injury proposed in 2009, traumatic aortic injury was classified into four categories based on the severity on CTA imaging. These included grade 1, intimal tear; grade 2, intramural hematoma; grade 3, aortic pseudoaneurysm; and grade 4, free rupture. Currently, surgical repair is recommended for grade 2-4 injuries. Since most grade 1 injuries heal spontaneously, expectant management with serial imaging is advised[15,16].
The patient’s pseudoaneurysm of the aortic isthmus was a grade 3 injury, and the aneurysm of right iliac artery dissection was a grade 1-2 injury. Endovascular stent graft repair was performed in the operating room. The patient was followed up for 4 years after the operation and eventually recovered well.
Traumatic aortic injury has an incidence of less than 1% in all trauma patients but occurs in one-third of blunt traumatic fatalities, with the majority of deaths occurring at the scene[14]. Due to the extremely low incidence and high mortality, early diagnosis may be difficult but is very important to reduce mortality and improve the prognosis of patients with trauma. Emergency trauma centers should emphasize the identification with clinical cues, which include gross asymmetry in systolic blood pressure (between the two upper limbs or between the upper and lower limbs), widened pulse pressure (as in our case), and chest wall contusion (as in our case, the initial chest CT revealed a mediastinal hematoma). We need to be vigilant for symptoms persisting or developing, even when the initial screening results are negative. Dynamic thoracic and abdominal aortic CTA review should be performed if necessary.
| 1. | Neschis DG, Scalea TM, Flinn WR, Griffith BP. Blunt aortic injury. N Engl J Med. 2008;359:1708-1716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 201] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 2. | Parmley LF, Mattingly TW, Manion WC, Jahnke EJ Jr. Nonpenetrating traumatic injury of the aorta. Circulation. 1958;17:1086-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 933] [Cited by in RCA: 830] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 3. | Nzewi O, Slight RD, Zamvar V. Management of blunt thoracic aortic injury. Eur J Vasc Endovasc Surg. 2006;31:18-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 53] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Beel T, Harwood AL. Traumatic rupture of the thoracic aorta. Ann Emerg Med. 1980;9:483-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 19] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | He S, Chen X, Zhou X, Hu Q, Ananda S, Zhu S. Sudden death due to traumatic ascending aortic pseudoaneurysms ruptured into the esophagus: 2 case reports. Medicine (Baltimore). 2015;94:e716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Schulman CI, Carvajal D, Lopez PP, Soffer D, Habib F, Augenstein J. Incidence and crash mechanisms of aortic injury during the past decade. J Trauma. 2007;62:664-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Fattori R, Russo V, Lovato L, Di Bartolomeo R. Optimal management of traumatic aortic injury. Eur J Vasc Endovasc Surg. 2009;37:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Meyer A, Bal A, Kuefner MA, Schmid A, Lang W. Aortic pseudo-aneurysm due to traumatic avulsion of an intercostal artery. EJVES Extra. 2011;22:e40-e43. [DOI] [Full Text] |
| 9. | Numata S, Ogino H, Sasaki H, Ando M. Traumatic pseudoaneurysm located at distal descending aorta. Interact Cardiovasc Thorac Surg. 2003;2:452-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | O'Conor CE. Diagnosing traumatic rupture of the thoracic aorta in the emergency department. Emerg Med J. 2004;21:414-419. [PubMed] |
| 11. | Mouawad NJ, Paulisin J, Hofmeister S, Thomas MB. Blunt thoracic aortic injury - concepts and management. J Cardiothorac Surg. 2020;15:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 83] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 12. | Lundervall J. The Mechanism of traumatic rupture of the aorta. Acta Pathol Microbiol Scand. 1964;62:34-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 86] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 13. | Elganayni F, Abdulghaffar W, Sale HA, Abou-Issa AH, Abouelcibaa O, Bafaraj M, Bayomi MA. Acute traumatic injuries of thoracic aorta: role of 64-MDCTA in diagnosis and management. Egypt J Radiol Nuclear Med. 2012;43:203-210. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Downing SW, Sperling JS, Mirvis SE, Cardarelli MG, Gilbert TB, Scalea TM, McLaughlin JS. Experience with spiral computed tomography as the sole diagnostic method for traumatic aortic rupture. Ann Thorac Surg. 2001;72:495-501; discussion 501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 52] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Azizzadeh A, Keyhani K, Miller CC 3rd, Coogan SM, Safi HJ, Estrera AL. Blunt traumatic aortic injury: initial experience with endovascular repair. J Vasc Surg. 2009;49:1403-1408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 289] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 16. | Lee WA, Matsumura JS, Mitchell RS, Farber MA, Greenberg RK, Azizzadeh A, Murad MH, Fairman RM. Endovascular repair of traumatic thoracic aortic injury: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg. 2011;53:187-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 523] [Cited by in RCA: 457] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jain S, India; Papazafiropoulou A, Greece; Syahputra DA, Indonesia S-Editor: Fan JR L-Editor: A P-Editor: Fan JR