©The Author(s) 2025.
World J Clin Cases. Nov 16, 2025; 13(32): 111796
Published online Nov 16, 2025. doi: 10.12998/wjcc.v13.i32.111796
Published online Nov 16, 2025. doi: 10.12998/wjcc.v13.i32.111796
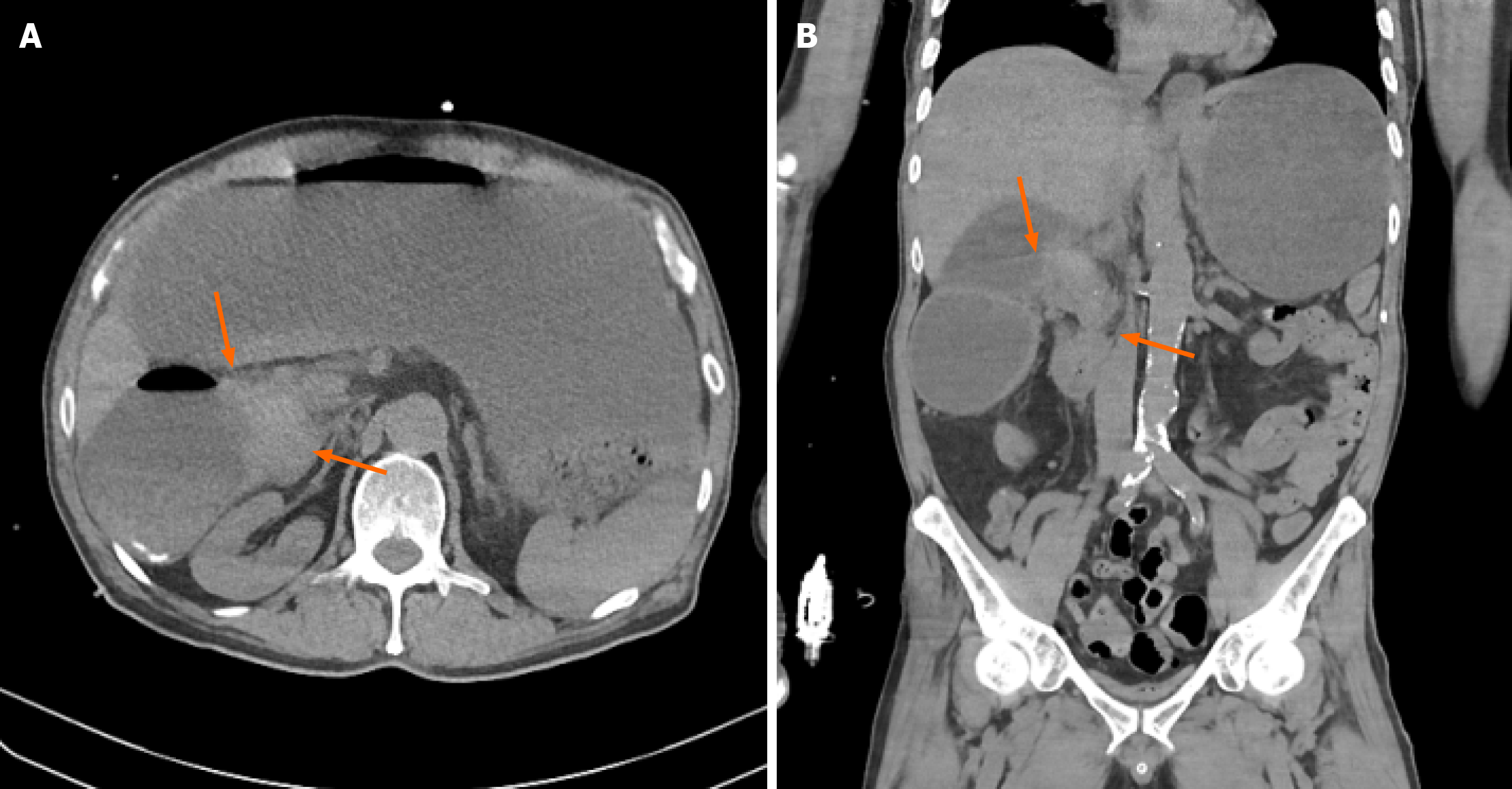
Figure 1 Computed tomography imaging findings.
Non-contrast abdominal computed tomography scan showing a mass-like lesion (orange arrow) causing a severe luminal stricture in the second portion of the duodenum and marked dilatation of the stomach and first portion of the duodenum. A: Non-contrast axial image; B: Non-contrast coronal image.
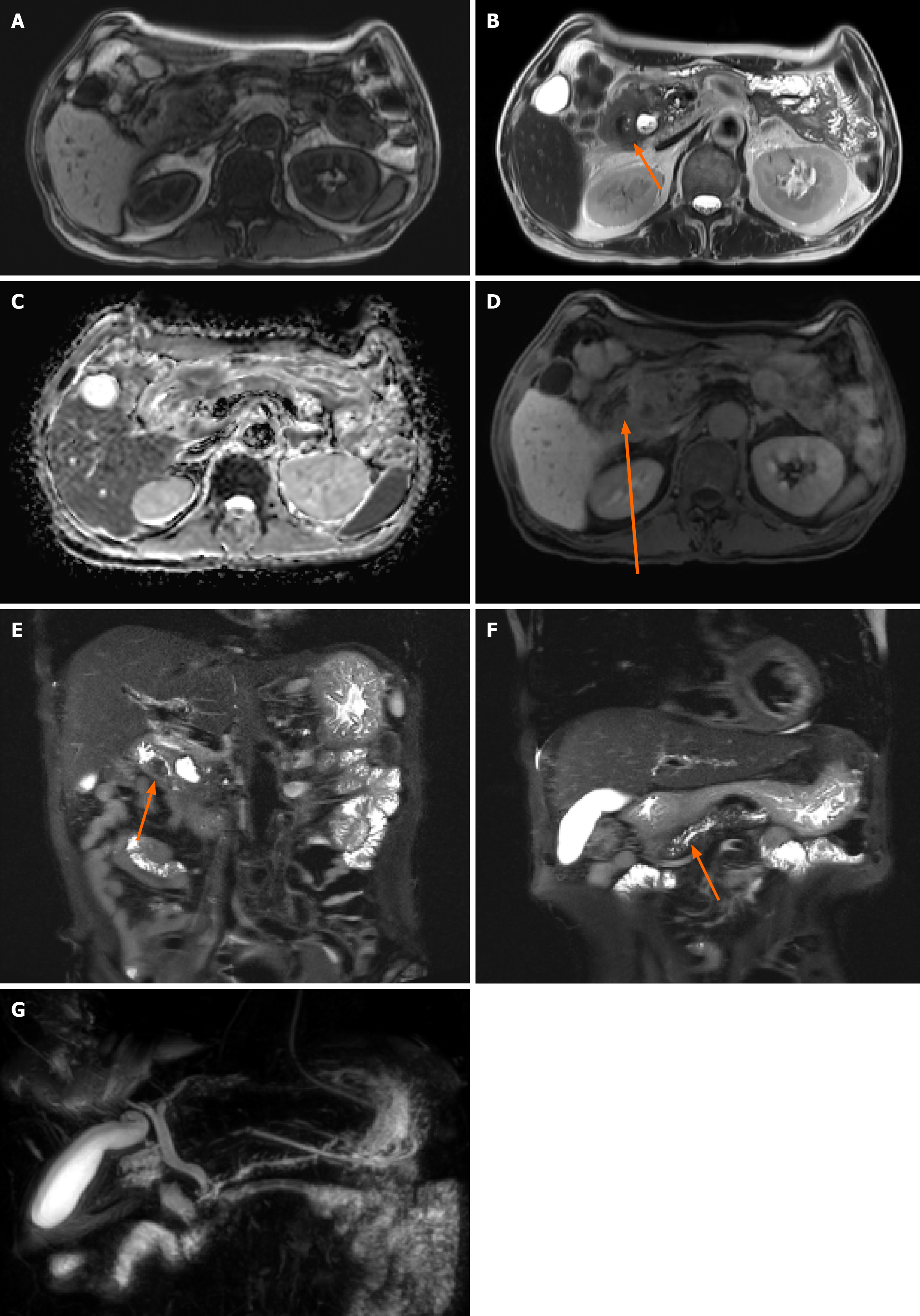
Figure 2 Pancreatic magnetic resonance imaging findings.
A: T1 weighted image; B: T2 weighted axial image; C: Diffusion weighted image; D: Vibe image; E and F: T2 weight coronal image; G: Magnetic resonance cholangiopancreatography. Magnetic resonance imaging showing a lesion in the ampulla of Vater with no clear T1 weighted and diffusion restriction image (A and C) but prominent enhancement, which is suspicious for ampulla of Vater cancer (B, D and E); magnetic resonance imaging showing main pancreatic duct upstream dilatation (F and G).
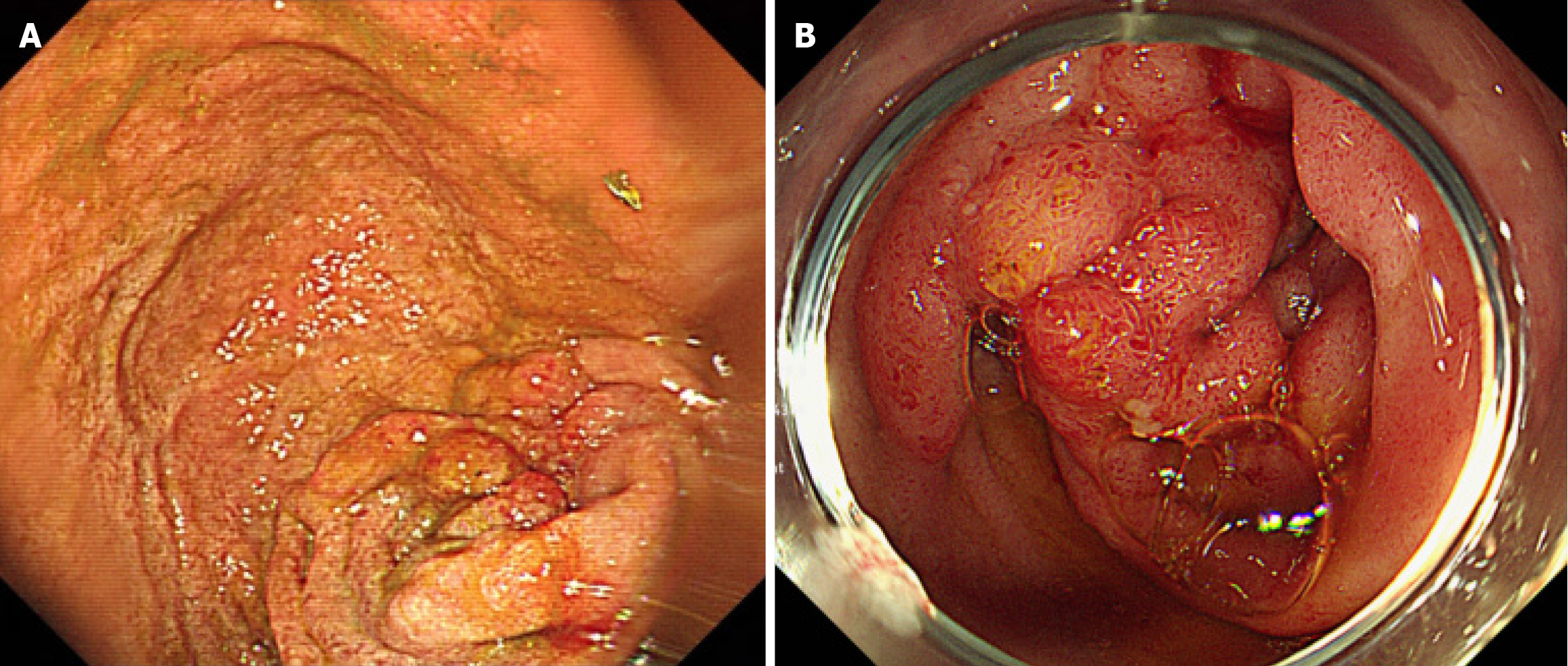
Figure 3 Esophagogastroduodenoscopy findings.
A: A mass-like lesion located at the pyloric antrum to the duodenal bulb with complete obstruction, preventing the esophagogastroduodenoscopy scope from passing through the duodenal bulb; B: Esophagogastroduodenoscopy performed to biopsy the suspected ampulla of Vater cancer showing no ampulla of Vater mass, but instead a duodenal bulb mass-like lesion.
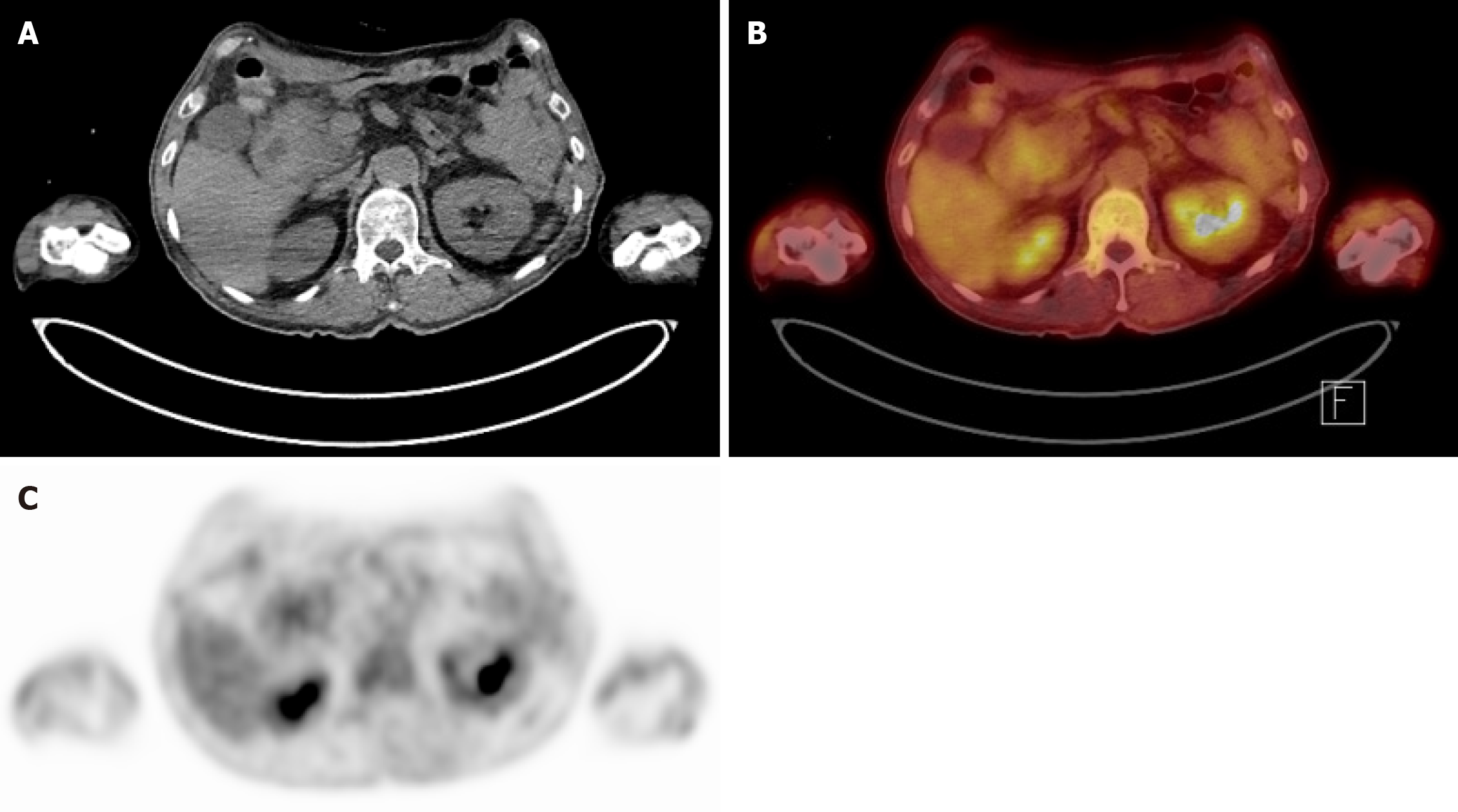
Figure 4 Positron emission tomography-computed tomography images.
A: Axial computed tomography torso image. Mass at periampullary area; B: Fusion positron emission tomography-computed tomography image demonstrating a mild hypermetabolic mass-like lesion in the second portion of the duodenum near the ampulla of Vater of unknown clinical significance; C: Axial positron emission tomography image showing the corresponding focal uptake in the same region of (B).
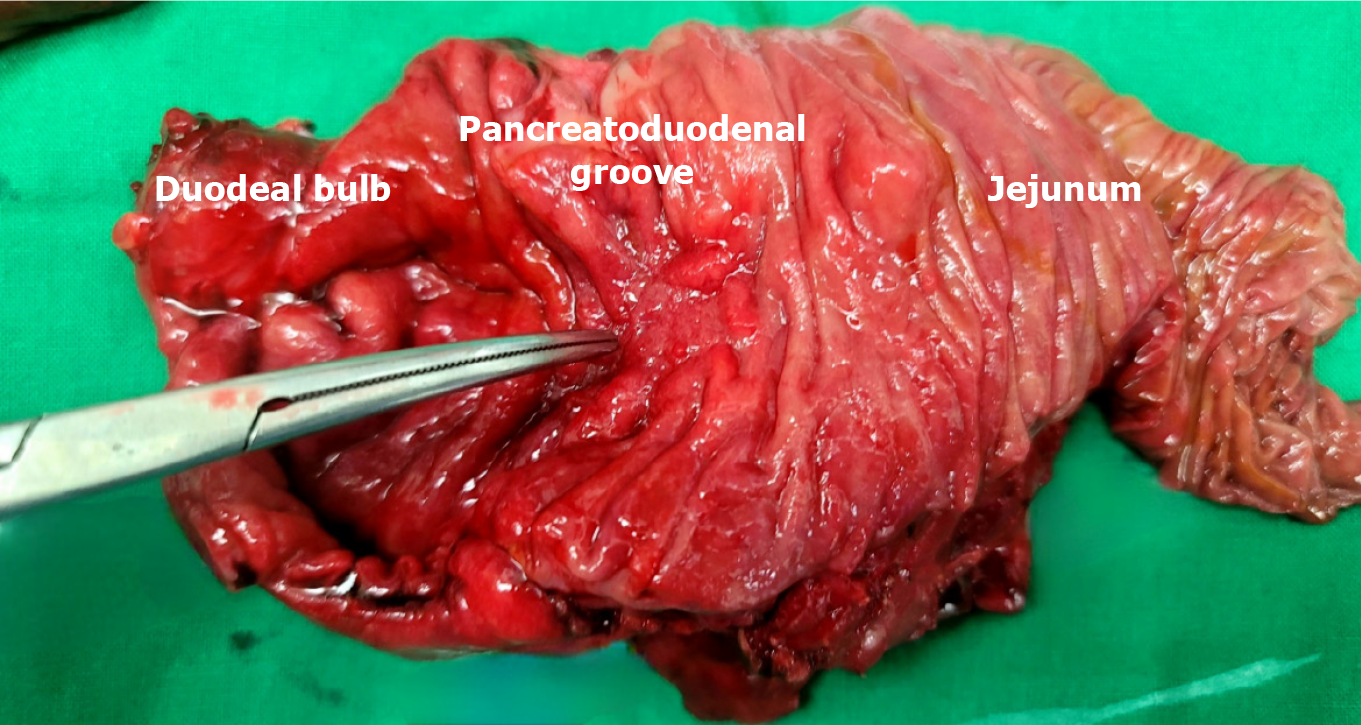
Figure 5 The specimen findings after pylorus-resecting pancreaticoduodenectomy.
No mass-like lesion suspected upon preoperative imaging is observed on the postoperative specimen. However, grossly inflammatory changes are observed in the duodenal mucosa at the pancreaticoduodenal groove due to chronic pancreatitis.
Figure 6 One-year follow-up abdominal contrast-enhanced computed tomography after pancreaticoduodenectomy.
The images demonstrate postoperative anatomical changes without evidence of surgical complications such as anastomotic leakage or intra-abdominal abscess. However, after the patient resumed alcohol consumption, the computed tomography revealed a perihepatic fluid collection in the perihepatic space. A: Axial view; B: Coronal view.
- Citation: Kim N, Lee H, Park D. Challenging diagnosis of groove pancreatitis with severe gastric outlet obstruction: A case report. World J Clin Cases 2025; 13(32): 111796
- URL: https://www.wjgnet.com/2307-8960/full/v13/i32/111796.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i32.111796