Published online Oct 24, 2025. doi: 10.5306/wjco.v16.i10.110531
Revised: June 24, 2025
Accepted: September 17, 2025
Published online: October 24, 2025
Processing time: 137 Days and 23.5 Hours
Cancer rehabilitation is a critical component of comprehensive cancer care, aiming to improve the quality of life for cancer survivors by addressing physical, psychological, and social challenges following treatment. In India, with rising cancer incidence and a growing survivor population, the need for effective rehabilitation services is more pronounced than ever. However, despite significant progress in cancer treatment, rehabilitation remains an underdeveloped and underutilized area of care in the country. This mini-review explores the current status of cancer rehabilitation in India, highlighting existing gaps in healthcare infrastructure, access, and awareness. It examines the scope of rehabilitation services-including physical therapy, psychosocial support, palliative care, and vocational rehabilitation-and identifies regional variations in service availability. Furthermore, the mini-review outlines challenges faced by healthcare providers, such as a shortage of trained professionals, limited funding, and cultural stigmas surrounding cancer. Future perspectives on cancer rehabilitation in India emphasize the need for policy reforms, integration of rehabilitation into national cancer care programs, and promotion of multidisciplinary care teams. The article concludes with recommendations for expanding cancer rehabilitation services to meet the evolving needs of survivors and to enhance their long-term well-being in India.
Core Tip: Cancer rehabilitation remains an essential yet under-recognized component of oncology care in India. With a rising number of cancer survivors, there is a growing need to address the complex physical, psychological, and social challenges they face after treatment. This mini-review identifies critical gaps in infrastructure, access, and specialized workforce, while outlining the potential of multidisciplinary rehabilitation services. It underscores the importance of policy integration, awareness, and capacity building to establish cancer rehabilitation as a standardized element of survivorship care nationwide.
- Citation: Swarnakar R, Yadav SL. Cancer rehabilitation in India: Current status, scope, and future perspectives. World J Clin Oncol 2025; 16(10): 110531
- URL: https://www.wjgnet.com/2218-4333/full/v16/i10/110531.htm
- DOI: https://dx.doi.org/10.5306/wjco.v16.i10.110531
Cancer rehabilitation is an emerging and essential component of comprehensive cancer care, particularly in the Indian context, where the burden of cancer is steadily increasing. With advances in early detection and treatment, survival rates have improved significantly; however, survivors often face long-term physical, psychological, and social challenges that impair their quality of life. Onco-rehabilitation-a specialized branch of rehabilitation focused on individuals diagnosed with cancer-aims to restore function, reduce disability, and promote independence throughout the cancer care continuum. Unlike general rehabilitation, which addresses a broad spectrum of disabilities, onco-rehabilitation tailor interventions to the unique functional challenges caused by cancer and its treatments[1].
Recognizing the global importance of this field, the International Society of Physical and Rehabilitation Medicine (ISPRM) have designated June 6 as World Cancer Rehabilitation Day, highlighting the need for integrated rehabilitation services for cancer patients and survivors worldwide. Despite its proven benefits, onco-rehabilitation remains underdeveloped in India and other low-income and middle-income countries[2]. This article explores the current status of cancer rehabilitation services, examines the existing scope for growth, and outlines future perspectives to ensure that survivors receive holistic, lifelong care across all phases of their cancer journey.
Cancer remains one of the foremost causes of death across the globe[3]. The most frequently diagnosed types include breast, lung, colorectal, and prostate cancers. The estimated number of incident cases of cancer in India for the year 2022 was found to be 1461427 (crude rate: 100.4 per 100000)[4]. Within childhood cancers (0-14 years), lymphoid leukemia emerged as the predominant site, accounting for 29.2% in boys and 24.2% in girls. According to the Indian Council of Medical Research, the estimated number of incidences of cancer cases was more than 14 Lakhs in 2023 in India[4].
Cancer survivorship encompasses the overall health and quality of life of individuals from the moment they are diagnosed through the remainder of their lives. It addresses a wide range of challenges-physical, emotional, psychological, social, and financial-that may arise during and after treatment[5]. Survivorship also involves managing ongoing care, such as routine health monitoring, dealing with long-term side effects of treatment, the possibility of the cancer returning, the development of new cancers, and maintaining a good quality of life. The experience extends beyond the patient to include the support systems around them, including family members, caregivers, and close friends[5].
Currently, in India, there are many institutes where Physical Medicine and Rehabilitation (PMR) services are provided by specialist doctors. Similarly, several cancer hospitals offer cancer care through specialists. However, there is a significant lack of dedicated onco-rehabilitation services provided by PMR specialists in the country.
Many institutes offer general rehabilitation care to cancer patients through outpatient departments, but specialized rehabilitation remains limited. In both private and government institutions across India, cancer rehabilitation services have gradually been introduced. Among them, the National Cancer Institute, Jhajjar-under the All India Institute of Medical Sciences, New Delhi-is a notable example, as it has initiated specialized rehabilitation services for cancer patients.
Cancer is increasingly being viewed not just as a disease to be cured, but as a condition requiring long-term, holistic care. With rising cancer incidence and improved survival rates in India, there is a growing recognition of the importance of cancer rehabilitation. This essential component of care focuses on improving the quality of life of patients by addressing the physical, psychological, and social challenges that arise during and after treatment. However, the current state of cancer rehabilitation in India reflects both emerging progress and significant challenges.
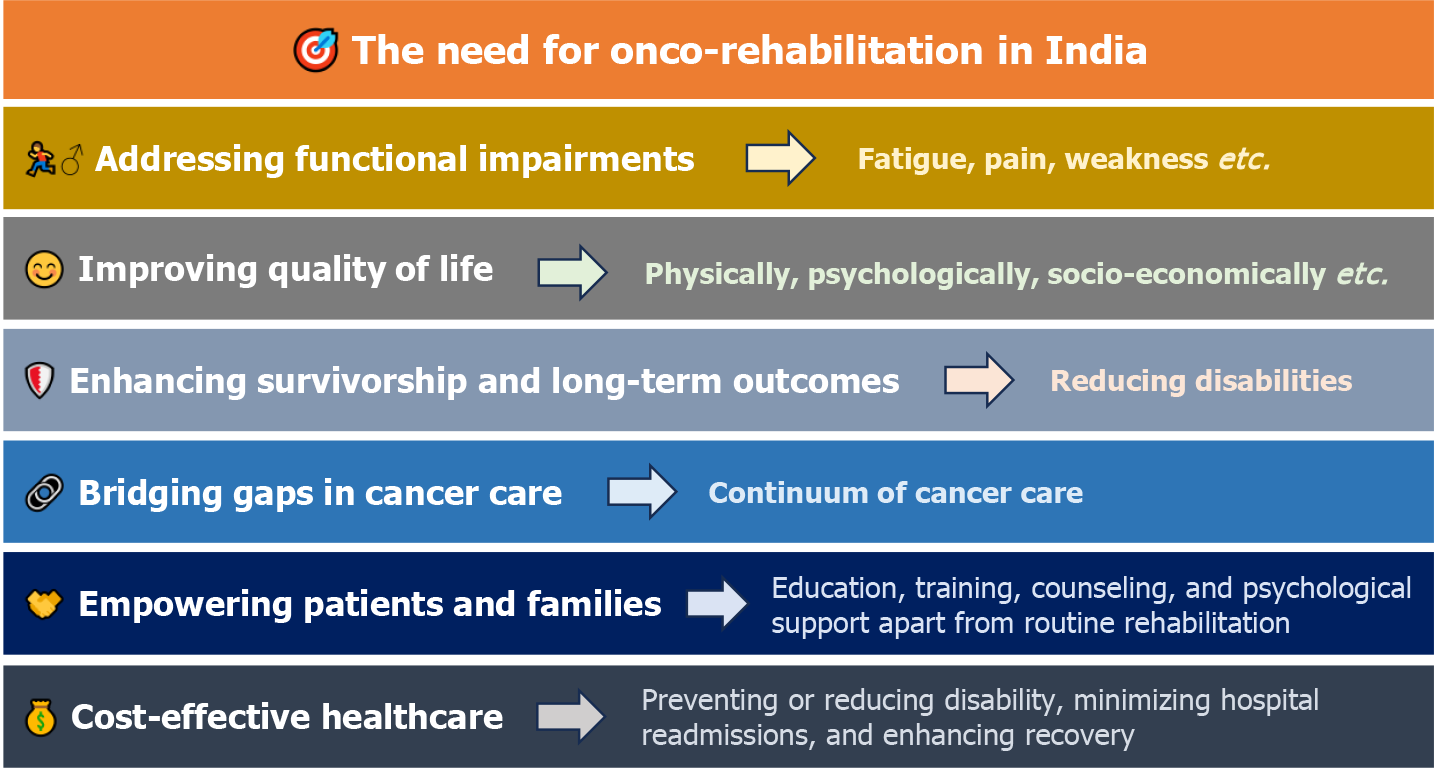
As cancer incidence rises and survival rates improve, the spotlight is increasingly turning toward life after cancer treatment. While diagnosis and curative interventions remain critical, post-treatment conditions can be equally important. Hence, onco-rehabilitation-rehabilitation for individuals diagnosed with cancer-becomes a vital aspect of holistic cancer care (Figure 1)[6-8]. The needs are as follows: (1) Addressing functional impairments: Cancer and its treatments often lead to a range of physical impairments: Fatigue, pain, lymphedema, neuropathy, muscle weakness, speech and swallowing difficulties, joint stiffness or mobility issues. Without timely and structured rehabilitation, these conditions can severely limit a patient's ability to perform daily activities, affecting independence and quality of life; (2) Improving quality of life: Beyond physical issues, many patients face emotional, psychological, and social challenges such as: Anxiety or depression, body image concerns, loss of confidence, difficulty returning to work or social roles. Onco-rehabilitation integrates mental health support, counseling, and social reintegration strategies to address these needs, promoting holistic recovery; (3) Enhancing survivorship and long-term outcomes: Cancer survivorship is not just about living longer, but living well; (4) Rehabilitation supports: Early return to normal function, reduced risk of long-term disability, improved adherence to ongoing medical care, better physical and emotional resilience, rehabilitation helps survivors maintain or regain the best possible level of functioning post-treatment[1,7]; (5) Bridging gaps in cancer care: While many hospitals focus on diagnosis, surgery, chemotherapy, and radiation, rehabilitation is often overlooked. Onco-rehabilitation bridges this gap by offering: Continuity of care from diagnosis to survivorship, integration with medical and supportive services, personalized care plans for each patient’s unique needs; (6) Empowering patients and families: Through education, exercise training, nutritional counseling, and psychological support, onco-rehabilitation empowers patients and caregivers to take an active role in recovery. It also helps reduce caregiver burden and improve home-based care readiness; and (7) Cost-effective healthcare: By preventing or reducing disability, minimizing hospital readmissions, and enhancing recovery, onco-rehabilitation can lead to better health outcomes at lower long-term costs-a crucial factor in resource-constrained settings like India.
Cancer rehabilitation services in India are limited, inconsistently available, and primarily concentrated in urban tertiary centers. While some advanced hospitals have begun integrating rehabilitation within oncology departments, access to structured, specialized care remains sparse. Most patients receive basic physiotherapy through outpatient clinics, often without multidisciplinary input, continuity, or follow-up.
Comprehensive rehabilitation-addressing physical, psychological, and social dimensions-is rarely incorporated as a standard component of cancer care, particularly from the point of diagnosis. Interdepartmental coordination is minimal, and rehabilitation is frequently seen as an optional adjunct rather than a core part of the treatment continuum.
PMR specialists play a central role in onco-rehabilitation, managing complex impairments such as lymphedema, neuropathic pain, post-surgical weakness, and mobility limitations. However, India faces a significant shortage of trained PMR physicians, resulting in most rehabilitation services being delivered by physiotherapists without specialist oversight[9-11].
This lack of specialist-led, individualized rehabilitation planning is a critical barrier to optimizing functional outcomes and independence among cancer survivors. Without early and structured interventions, many patients are left with preventable disabilities and reduced quality of life.
In addition to hospital-based services, some community organizations provide support such as counseling, vocational training, nutritional advice, and temporary accommodation during treatment. These services are particularly valuable for economically disadvantaged patients[12,13]. However, such programs are scattered, often limited in scale, and not formally integrated into the healthcare system.
One of the major challenges in India is the absence of national guidelines mandating cancer rehabilitation as an essential component of oncology care. This results in fragmented implementation and limited institutional commitment. For example, while the National Cancer Institute, Jhajjar, has successfully started PMR-led rehabilitation into cancer care, most centers across the country still need more structured rehab pathways in standardized protocols and policy direction.
There is significant potential to enhance onco-rehabilitation in public health schemes such as in Ayushman Bharat by enhancing customised comprehensive cancer rehabilitation services, such as physiotherapy, occupational therapy, speech therapy, and mental health support. Doing so would reduce out-of-pocket expenses and promote equity in survivorship care.
Awareness among healthcare providers and patients remains low. In many settings, rehabilitation is still perceived as an optional service rather than a necessary part of cancer care. A qualitative study at a tertiary hospital in Maharashtra highlighted that survivors often viewed rehabilitation as something reserved for severe disability or end-stage care, reflecting a gap in patient education and provider training.
In summary, the key systemic challenges include limited policy backing, inadequate insurance coverage, and insufficient awareness. Nonetheless, pilot initiatives and institutional experiences demonstrate that with appropriate policy support and integration into existing health programs, cancer rehabilitation can be expanded effectively to meet the growing needs of India's survivor population.
India is witnessing a steady rise in cancer cases, with over 1.5 million new cases diagnosed annually. Advances in medical technology and treatment modalities have improved cancer survival rates. However, many survivors face lingering effects of treatment-physical disabilities, psychological trauma, fatigue, pain, and loss of functional independence. Cancer rehabilitation (onco-rehabilitation) is a specialized branch of care designed to help individuals overcome these challenges and regain optimal quality of life.
Despite its importance, cancer rehabilitation remains underdeveloped and underutilized in India. There is a significant opportunity to integrate and expand this service to support the growing population of survivors across all socio-economic backgrounds.
Expanding survivor population: India’s growing number of cancer survivors-currently estimated at over 3 million-is a key driver for cancer rehabilitation services. Many survivors live with chronic complications of treatment: (1) Neuropathy; (2) Fatigue; (3) Joint stiffness; (4) Lymphoedema; and (5) Speech and swallowing issues, and more. Without rehabilitation, these conditions can become permanent disabilities, limiting productivity, independence, and overall well-being. This growing survivor population demands long-term support, structured follow-up care, and rehabilitative intervention as part of standard cancer management.
Multidisciplinary opportunities: Cancer rehabilitation requires a team-based approach, offering opportunities for collaboration across multiple specialties: PMR physicians lead in assessing and managing functional impairments. Physiotherapists and occupational therapists address exercises for mobility, strength, endurance, and daily living tasks respectively. Speech and swallowing therapists play a vital role in post-head and neck cancer cases. Psychologists and psychiatrists manage emotional distress, depression, anxiety, and cognitive dysfunction. Nutritionists, social workers, and palliative care specialists contribute to a comprehensive recovery plan. This wide scope allows institutions to create dedicated cancer rehab teams, enhancing patient outcomes and professional collaboration[14].
Applicability across cancer types and stages: Rehabilitation is not confined to a specific phase or type of cancer: (1) Before treatment: Prehabilitation improves physical and mental resilience before surgery or chemotherapy. Safety checklist before rehabilitation is also an important aspect to be looked for[15]; (2) During treatment: Helps manage side effects, reduces hospital stay, and maintains function; (3) After treatment: Aids in recovery, regaining independence, and reintegration into work and social life; and (4) Palliative care: Supports symptom relief and quality of life, even when cure is not the goal. Common cancers requiring rehabilitation support include breast, head and neck, prostate, brain, lung, gynecological, pediatric, and bone tumors.
Untapped rural and community-based potential: India’s vast rural population faces limited access to cancer rehab services: Most services are confined to metro cities and tertiary hospitals. There is enormous potential to develop community-based rehabilitation models: Training local health workers in basic rehab techniques, using mobile health units and tele-rehab platforms, developing linkages between district hospitals and rehab centers. Such models can improve early identification and management of disabilities, especially in low-resource settings[12,13].
Education, training, and research: There is a strong scope to expand academic and research activities in this field: (1) Medical education: Onco-rehabilitation is still not part of standard MBBS or MD curricula in many institutes. Introducing modules in undergraduate and postgraduate training will enhance awareness and interest; (2) Specialized training: Fellowship programs, workshops, and skill-based certifications can increase the pool of trained professionals[16]; and (3) Research potential: India needs more evidence-based data on rehabilitation outcomes, cost-effectiveness, survivorship quality, and culturally relevant rehab protocols. In future it can be one subspecialty of PMR[17].
Policy integration: Cancer rehabilitation is yet to be formally recognized in most national healthcare policies[18]. A future-oriented strategy should include: Making rehabilitation a mandatory part of oncology guidelines (like surgical, medical, and radiation oncology). Incorporating rehab services into cancer control programs.
Capacity building: India faces a shortage of trained PMR doctors and rehab professionals: Increase the number of MD PMR seats in government and private institutions. Create fellowships in onco-rehabilitation, particularly in large cancer centers. Train physiotherapists, nurses, and counselors in cancer-specific rehab protocols. Build interdisciplinary teams in both cancer hospitals and general hospitals to improve coverage.
Technology and innovation: Leveraging technology can revolutionize rehabilitation delivery: Tele-rehabilitation platforms can allow remote physiotherapy, counseling, and monitoring, especially in rural areas[19,20]. Mobile apps can guide patients in performing home exercises, tracking symptoms, and managing appointments. Wearables (e.g., fitness trackers, pressure sensors) can monitor recovery and physical activity. Artificial intelligence-based systems can help personalize rehab plans and predict risks of functional decline. To make technological innovation in cancer rehabilitation more effective in India, solutions must align with local contexts. Hybrid tele-rehabilitation models can link district health centers with tertiary hospitals, leveraging Ayushman Bharat’s Health and Wellness Centers and community health workers for home-based interventions. Culturally tailored approaches such as incorporating yoga, pranayama, and ayurvedic principles into rehab protocols-especially through Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy centers-hold promise, with early institutional studies showing benefits in fatigue and mental wellbeing. Developing low-bandwidth mobile apps in regional languages, using WhatsApp bots or voice-based systems, can enhance accessibility for patients with low digital literacy. Simple, low-cost rehabilitation kits with exercise tools and QR-linked video guides can be distributed via primary health centers or CSR programs. Locally manufactured wearables like GOQii can help monitor fatigue and function, feeding data into remote consultations. Finally, educational content through comic book-style leaflets, community radio, or video stories in regional languages can improve public understanding and adherence, making rehabilitation more acceptable and impactful across socio-economic groups.
Insurance and financial support: Rehabilitation services are rarely covered under health insurance, posing a burden for many families. Future efforts must focus on policy reforms to include rehabilitation under health packages. Government schemes, public-private partnerships, and CSR-driven initiatives can subsidize services for economically weaker sections. Outcome-based funding models can ensure sustainability and accountability in service delivery[21,22].
Integrated cancer care models: The ideal cancer care model of the future will be integrated and continuous: Rehabilitation should be initiated at the time of diagnosis and continued throughout the treatment and survivorship phases. Creating rehab pathways in cancer hospitals will ensure timely referrals and follow-up[23]. Collaboration between oncologists and PMR specialists should be institutionalized. Such models have shown improved patient outcomes, faster return to work, better psychosocial health, and reduced healthcare costs.
Public awareness and advocacy: Cancer rehabilitation remains poorly understood by the public and even by many healthcare professionals. Awareness campaigns can help demystify rehabilitation and reduce stigma. Involving survivor groups and patient advocates can drive demand for services and create community support systems. Educational tools like leaflets, videos, social media content, and survivor success stories can amplify the message[24].
Thus, by investing in specialized cancer rehabilitation infrastructure and training healthcare professionals in evidence-based practices, India can improve cancer rehab services in line with high-income countries (Table 1)[25].
| Focus area | Key actions | How to implement |
| Policy integration | Include cancer rehab in national health policies and oncology guidelines | Via various national program |
| Capacity building | Increase training programs and human resources for onco-rehabilitation | Expand MD PMR seats, start fellowships, train rehab staff |
| Technology and innovation | Utilize digital health, artificial intelligence, culturally adapted models | Develop mobile apps, use tele-rehab, integrate Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy practices |
| Insurance and financial support | Improve financial access to rehabilitation | Include rehab under govt schemes, public-private models |
| Integrated care models | Embed rehab across all phases of cancer care | Hospital rehab pathways, PMR-oncology collaboration |
| Public awareness and advocacy | Increase awareness among patients, providers, policymakers | Campaigns, survivor groups, educational materials |
Cancer rehabilitation in India is still at a nascent stage, but its importance is undeniable in the evolving landscape of cancer care. While a few centers have begun to integrate rehabilitation into oncology services, access remains limited, particularly in rural and underserved regions. The scope for expanding these services is vast, encompassing clinical, educational, technological, and policy domains. The recognition of June 6 as World Cancer Rehabilitation Day by ISPRM serves as a timely reminder for healthcare systems, policymakers, and institutions in India to prioritize and mainstream rehabilitation as a core element of cancer care. Moving forward, India must adopt a multi-pronged strategy-strengthening infrastructure, increasing specialist training, leveraging telehealth, and integrating rehabilitation into national cancer policies. By recognizing rehabilitation as a vital component of survivorship, India can ensure that cancer survivors not only live longer but live with dignity, functionality, and a better quality of life.
| 1. | Smith SR, Zheng JY, Silver J, Haig AJ, Cheville A. Cancer rehabilitation as an essential component of quality care and survivorship from an international perspective. Disabil Rehabil. 2020;42:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Cai R, Lin H, Mao Q, Zhang C, Tan Y, Cheng Q. Research hotspots and trends in cancer rehabilitation: a bibliometric analysis (2013-2023). Support Care Cancer. 2025;33:296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | World Health Organization website. Cancer. 2025. Available from: https://www.who.int/news-room/fact-sheets/detail/cancer. |
| 4. | Sathishkumar K, Chaturvedi M, Das P, Stephen S, Mathur P. Cancer incidence estimates for 2022 & projection for 2025: Result from National Cancer Registry Programme, India. Indian J Med Res. 2022;156:598-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 305] [Article Influence: 76.3] [Reference Citation Analysis (0)] |
| 5. | National Cancer Institute. The NCI Dictionary of Cancer Terms: Survivorship. [accessed on June 1, 2025]. Available from: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/survivorship. |
| 6. | Cheville AL, Mustian K, Winters-Stone K, Zucker DS, Gamble GL, Alfano CM. Cancer Rehabilitation: An Overview of Current Need, Delivery Models, and Levels of Care. Phys Med Rehabil Clin N Am. 2017;28:1-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 102] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 7. | Thorsen L, Gjerset GM, Loge JH, Kiserud CE, Skovlund E, Fløtten T, Fosså SD. Cancer patients' needs for rehabilitation services. Acta Oncol. 2011;50:212-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 8. | Lehmann JF, DeLisa JA, Warren CG, deLateur BJ, Bryant PL, Nicholson CG. Cancer rehabilitation: assessment of need, development, and evaluation of a model of care. Arch Phys Med Rehabil. 1978;59:410-419. [PubMed] |
| 9. | Palacio A, Calmels P, Genty M, Le-Quang B, Beuret-Blanquart F. Oncology and physical medicine and rehabilitation. Ann Phys Rehabil Med. 2009;52:568-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Cheville AL, Basford JR. Role of rehabilitation medicine and physical agents in the treatment of cancer-associated pain. J Clin Oncol. 2014;32:1691-1702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Lopez-Aponte C, Ramos-Guasp W, Sepulveda-Irrizary F, Lopez-Acevedo CE, Rosario-Concepcion R. Physiatrists' Attitudes and Knowledge About Cancer Rehabilitation. Cureus. 2022;14:e28622. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Wood KC, Hidde M, Kendig T, Pergolotti M. Community-based outpatient rehabilitation for the treatment of breast cancer-related upper extremity disability: an evaluation of practice-based evidence. Breast Cancer. 2022;29:1099-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Rajotte EJ, Yi JC, Baker KS, Gregerson L, Leiserowitz A, Syrjala KL. Community-based exercise program effectiveness and safety for cancer survivors. J Cancer Surviv. 2012;6:219-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Kudre D, Chen Z, Richard A, Cabaset S, Dehler A, Schmid M, Rohrmann S. Multidisciplinary Outpatient Cancer Rehabilitation Can Improve Cancer Patients' Physical and Psychosocial Status-a Systematic Review. Curr Oncol Rep. 2020;22:122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 15. | Maltser S, Cristian A, Silver JK, Morris GS, Stout NL. A Focused Review of Safety Considerations in Cancer Rehabilitation. PM R. 2017;9:S415-S428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Yadav RR, Ngo-Huang AT, Ng A, Fu JB, Custodio C, Wisotzky E, Mitra R, Bruera E. Characteristics of Cancer Rehabilitation Fellowship Training Programs in the USA. J Cancer Educ. 2018;33:1364-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Gamble GL, Gerber LH, Spill GR, Paul KL. The future of cancer rehabilitation: emerging subspecialty. Am J Phys Med Rehabil. 2011;90:S76-S87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Hewitt M, Maxwell S, Vargo MM. Policy issues related to the rehabilitation of the surgical cancer patient. J Surg Oncol. 2007;95:370-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Tay SS, Zhang F, Neo EJR. The use of technology in cancer prehabilitation: a systematic review. Front Oncol. 2024;14:1321493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 20. | Amarelo A, Mota M, Amarelo B, Ferreira MC, Fernandes CS. Technological Resources for Physical Rehabilitation in Cancer Patients Undergoing Chemotherapy: A Scoping Review. Cancers (Basel). 2024;16:3949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 21. | The Relationship Between Insurance Coverage and Cancer Care: A Literature Synthesis [Internet]. Research Triangle Park (NC): RTI Press; 2009 May- . [PubMed] |
| 22. | Politi MC, Grant RL, George NP, Barker AR, James AS, Kuroki LM, McBride TD, Liu J, Goodwin CM. Improving Cancer Patients' Insurance Choices (I Can PIC): A Randomized Trial of a Personalized Health Insurance Decision Aid. Oncologist. 2020;25:609-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Swarnakar R, Yadav SL. Integration of rehabilitation and palliative care in cancer management: A futuristic model. World J Clin Cases. 2025;13:102326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Qin E, Lim S, Essman M, Howard I. Increasing cancer rehabilitation awareness and referrals in the Veterans Health Administration-A quality improvement initiative. PM R. 2023;15:1292-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 25. | Silver JK, Stout NL, Fu JB, Pratt-Chapman M, Haylock PJ, Sharma R. The State of Cancer Rehabilitation in the United States. J Cancer Rehabil. 2018;1:1-8. [PubMed] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/