Published online Nov 27, 2025. doi: 10.4240/wjgs.v17.i11.112182
Revised: August 7, 2025
Accepted: September 18, 2025
Published online: November 27, 2025
Processing time: 128 Days and 23 Hours
Laparoscopic appendectomy (LA) is the standard treatment for acute appendicitis in children, offering reduced postoperative pain and quicker recovery compared to open surgery. A critical aspect of LA is the secure closure of the appendiceal stump to avoid complications such as leakage and abscess formation. Various closure techniques are employed, including endoloops (ELs), staplers, clips, and energy devices; however, the optimal method remains unclear due to inconsistent evidence.
To systematically evaluate and rank the effectiveness and safety of different appendiceal stump closure techniques used in pediatric LA. By assessing out
This systematic review and network meta-analysis, conducted according to PRISMA and Cochrane guidelines, compared the effectiveness and safety of stump closure methods in pediatric LA. Databases searched included PubMed, Cochrane Central, Web of Science, and Scopus up to May 1, 2025. Eligible studies included both randomized and non-randomized designs reporting surgical outcomes in pediatric patients. Two reviewers independently extracted data and assessed the risk of bias using the Newcastle-Ottawa Scale. A frequentist network meta-analysis with a random-effects model was conducted using R software to evaluate total complications (primary outcome), as well as operative time and hospital stay (secondary outcomes). P-scores were used to rank the effectiveness of treatments.
Fourteen studies comprising over 50000 pediatric patients were included in the network meta-analysis comparing appendiceal stump closure techniques in LA. No significant differences in total postoperative complications or hospital stay were observed among techniques, including EL, endostapler, polymer clip, LigaSure, harmonic scalpel (HS), and sutures. HS showed a statistically significant reduction in operative time compared to EL (mean difference: -13.5 minutes), while other methods did not demonstrate significant time savings. No technique was associated with a statistically significant increase or decrease in postoperative complications or length of stay. Publication bias was minimal, and the methodological quality of included studies was moderate to good.
While all closure techniques show similar safety profiles, HS offers shorter operating times. These findings support tailoring stump closure method selection based on operative efficiency and resource availability.
Core Tip: Laparoscopic appendectomy (LA) is the standard treatment for acute appendicitis in children, offering reduced postoperative pain and quicker recovery compared to open surgery. A critical aspect of LA is the secure closure of the appendiceal stump to avoid complications such as leakage and abscess formation. Various closure techniques are used, including endoloops, staplers, clips, and energy devices, but the optimal method remains unclear due to inconsistent evidence.
- Citation: Elsayed WA, Elhadi SA, Gad D, Mohamed HM, Elsaid T, Omar MF, Almousa AA, Elkhouly A. Effectiveness of different appendiceal stump closure methods in laparoscopic appendectomy in children: A systematic review and network meta-analysis. World J Gastrointest Surg 2025; 17(11): 112182
- URL: https://www.wjgnet.com/1948-9366/full/v17/i11/112182.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i11.112182
Acute appendicitis is one of the most common surgical emergencies in the pediatric population, often requiring prompt surgical intervention to prevent serious complications such as perforation and peritonitis[1,2]. Since its introduction by Semm in the early 1980s, laparoscopic appendectomy (LA) has become the preferred surgical approach for treating appendicitis in children[3,4]. It offers several advantages over open surgery, including reduced postoperative pain, shorter hospital stays, lower risk of wound infection, and quicker return to daily activities[5]. As LA becomes increasingly common in pediatric practice, attention has turned to optimizing each procedure step, particularly the method used to secure the appendiceal stump[6].
Closure of the appendiceal stump is a critical step in LA, as inadequate sealing can lead to severe postoperative complications such as stump leakage, intra-abdominal abscesses (IAAs), postoperative ileus, wound infection, and small bowel obstruction (SBO)[7]. Various stump closure methods are currently employed in pediatric surgery to address this. These include pre-tied ligatures, such as endoloops (ELs), mechanical devices like endostaplers (ESs), and other options, including polymeric clips (PCs), titanium clips, and energy-based sealing systems like the LigaSure (LS) or harmonic scalpel (HS). Each technique offers unique benefits and limitations regarding ease of use, security, operative time, cost, and associated complication risks, contributing to considerable variability in surgical practice[8].
Several studies have compared these stump closure methods across various clinical outcomes. In addition to postoperative complications, essential factors include operative time, length of hospital stay (LOS), and the need for reoperation or readmission. Shorter operative durations and reduced hospital stays are desirable as they are generally associated with faster recovery and lower healthcare costs[9-11]. However, literature remains inconclusive, with some studies suggesting ESs may be quicker or more reliable[12]. In contrast, others report no significant difference in com
Methodological issues further limit the quality of available evidence. Many retrospective studies include small sample sizes and are conducted in single centers with heterogeneous patient populations. Furthermore, there is often in
Given the wide use of LA in pediatric surgery, the number of available stump closure techniques, and the inconsistencies in existing evidence, there is a clear need for a robust, comprehensive comparison of all methods. A network meta-analysis is ideally suited for this purpose, as it enables the simultaneous comparison of multiple interventions, even when direct head-to-head comparisons are limited.
This study aimed to systematically evaluate and rank the effectiveness and safety of different appendiceal stump closure techniques used in pediatric LA. By assessing outcomes such as postoperative complications, operative time, and LOS, this analysis seeks to provide evidence-based guidance to inform clinical decision-making and optimize patient care.
This systematic review and network meta-analysis complied with the PRISMA criteria. It conformed to the methodological standards specified in the Cochrane Handbook[15,16].
A thorough literature search was performed on PubMed, Cochrane Central, Web of Science, and Scopus until May 1, 2025. The search technique utilized a synthesis of keywords: ((((appendic* OR appendec*) AND stump) AND ("endo
We included studies that were randomized controlled trials, non-randomized designs including cohort (retrospective, prospective), case-control, and cross-sectional studies that involved patients with appendicitis who underwent LA, reported the stump closure method, and surgical outcomes. The exclusion criteria comprised studies involving patients who underwent conventional (open) appendectomy, those with multiple comorbidities that could affect surgical out
In this review, the commonly reported interventions for stump closure were EL, ES, PC, LS, HS, loop ligature (LL), and sutures (SU). For clarity and consistency, each of these interventions was analyzed and reported separately according to the terminology used in the original studies.
The screening and selection process was executed using Rayyan[17]. Two independent reviewers conducted a two-step screening of titles and abstracts. The full-text papers of possibly qualifying research were further examined for final inclusion. Disputes were settled via consensus deliberations.
Two reviewers separately extracted data using a standardized data collection instrument, and the extracted variables included author, year, country, intervention specifics, and outcomes. Baseline participant characteristics encompassed group allocation, sample size, male distribution, age of each group, cost of each group, and follow-up duration. All differences were addressed through dialogue.
Two authors independently assessed the quality of the included cohort studies using the Newcastle-Ottawa Scale, which evaluates the risk of bias across multiple domains, including selection of participants, comparability of study groups, and assessment of outcomes or exposures. Each study was assigned a total score and an overall quality rating based on these domains[18].
The primary outcome was the incidence of total complications, while the secondary outcomes were the LOS (in days) and operative time (in minutes).
We conducted a frequentist network meta-analysis utilizing the “netmeta” and “meta” packages in R. We aggregated data from cohort studies evaluating various appendiceal stump closure techniques. This approach incorporates both direct and indirect comparisons within an interconnected treatment network.
Effect estimates were determined as relative risks for dichotomous outcomes (e.g., complications) and mean differences for continuous outcomes (e.g., LOS and operative time), each accompanied by 95% confidence intervals (95%CIs). A random-effects model was consistently employed, utilizing restricted maximum likelihood estimation for inter-study variance.
We computed τ² to denote between-study variance and I² to measure the proportion of overall variability ascribed to heterogeneity rather than random chance. An I² score exceeding 50% was deemed indicative of considerable heterogeneity.
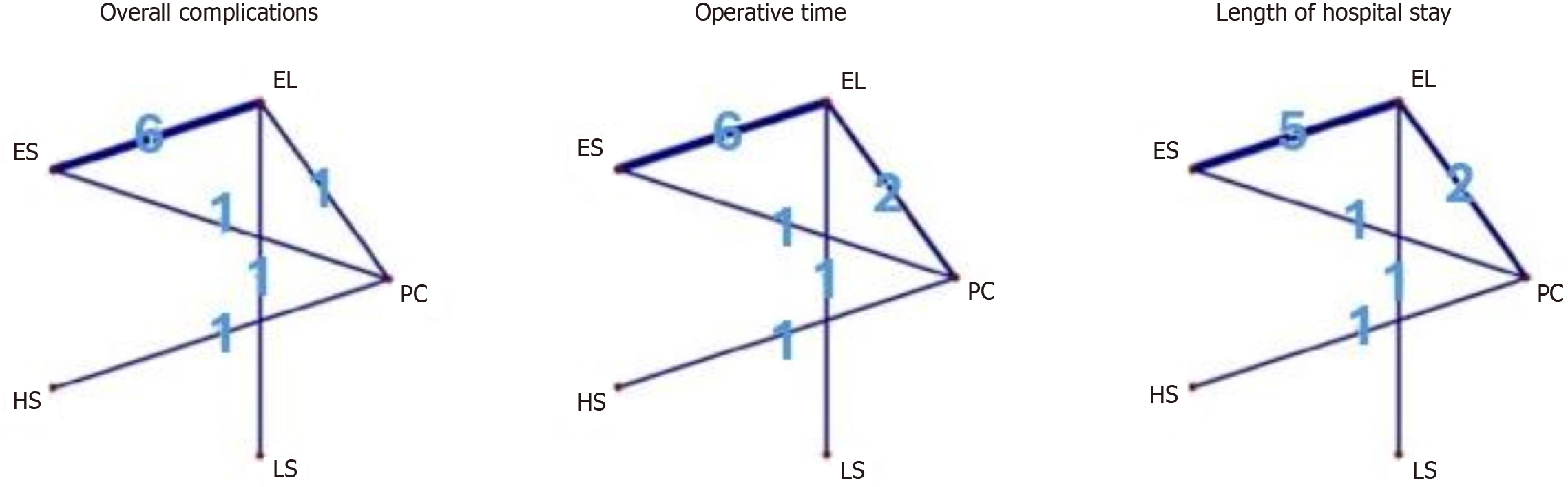
Network geometry was illustrated by network plots, where line thickness represented the quantity of studies per comparison.
Treatment ranking was conducted using P-scores, which measure the probability that a specific treatment surpasses others based on the average degree of superiority over competing therapies. P-scores span from 0 to 1, with elevated values signifying superior ranks. Forest plots, league tables, and contour-enhanced funnel plots were employed to illustrate effect sizes, rank treatments, and identify small-study effects or publication bias.
All analyses were conducted using R (version 4.4.3), with statistical significance established at P < 0.05.
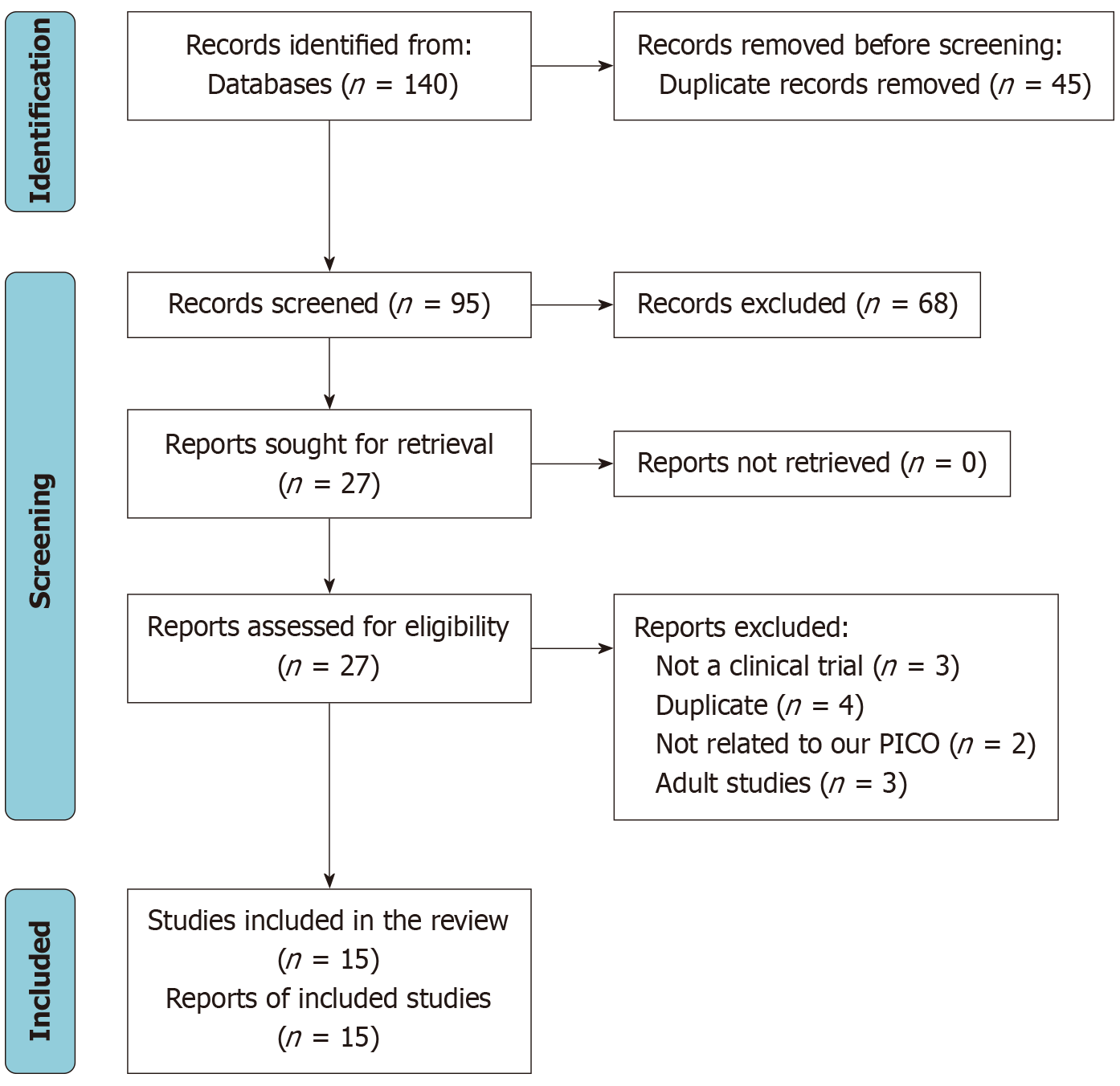
Our comprehensive search yielded 140 potential studies; 45 were discarded as duplicates. After title and abstract screening, an additional 68 research articles were removed, followed by the exclusion of 13 articles after full-text screening. Ultimately, we identified fourteen suitable papers for inclusion in the quantitative and qualitative synthesis of this systematic review (Figure 1).
The included studies compared various appendiceal stump closure techniques in pediatric LA across different countries and settings. Commonly assessed interventions included EL, ES, PC, LS, HS, LL, and SU. Most studies were retrospective cohort designs, with a few prospective cohorts and cross-sectional studies. Outcomes analyzed involved postoperative complications such as IAAs, wound infections, stump leaks, operative time, reoperation rates, hospital stay length, and cost (refer to Table 1).
| Ref. | Study design | Setting | Population | Intervention | Comparison | Outcomes |
| Akbiyik et al[24] | Prospective cohort | Türkiye | Pediatric patients underwent laparoscopic appendectomy with appendiceal stump closure using either endoloop ligatures or nonabsorbable polymer clips | Nonabsorbable pre-tied endoloop ligature | Two Hem-o-lok® clips (nonabsorbable polymeric clips) | Nonabsorbable polymer clips are a safe, efficient, and cost-effective alternative to endoloop ligatures for pediatric laparoscopic appendectomy, offering shorter ligation time and lower cost without added complications |
| Akkoyun and Akbiyik[25] | Retrospective cohort | Türkiye | Pediatric patients underwent laparoscopic appendectomy with appendiceal stump closure using nonabsorbable polymeric clips (Hem-o-lok) | In all cases, the appendiceal stump was closed using nonabsorbable polymeric clips (Hem-o-lok): Either a double clip closure or a single clip closure | Polymeric clips demonstrated safety and effectiveness for pediatric laparoscopic appendectomy, with short operative and recovery times, minimal complications confined to perforated cases, and no long-term clip-related issues during 13 months of follow-up | |
| Escolino et al[12] | Retrospective cohort | Multicenter | Pediatric patients underwent laparoscopic appendectomy with appendiceal stump closure using endoloop vs endostapler | Endoloop | Endo stapler | Compared with endoloop ligation, endostapler closure yielded fewer postoperative complications and lower overall costs despite higher supply expenses, with comparable operative and recovery outcomes, supporting its superior safety and cost-effectiveness |
| Juan et al[19] | Cross-sectional | Colombia | Pediatric patients underwent laparoscopic appendectomy with appendiceal stump closure using a bipolar sealing device (Ligasure) | The bipolar sealing device (LigaSure) closes the appendiceal stump by applying multiple consecutive seals with controlled energy delivery | The median operative time was 60 minutes with an average hospital stay of 2.8 days, and no stump leakage occurred; complications were rare (1% organ-space infection) and showed no association with stump closure method or appendix condition (P = 0.450) | |
| Kocaman et al[23] | Retrospective cohort | Türkiye | Patients underwent laparoscopic appendectomy with appendiceal stump ligation using endoloop vs LigaSure | Endoloop | LigaSure | LigaSure significantly reduced operative time compared with endoloop (29.6 minutes vs 39.2 minutes, P < 0.001), with no stump leakage or intra-abdominal abscess in either group, though port site infection was slightly more frequent with endoloop (P = 0.043) |
| Martinez et al[14] | Retrospective cohort | United States | Pediatric patients underwent a laparoscopic appendectomy for acute, uncomplicated appendicitis, for which the appendiceal stump was managed with either a Surgical stapler or a polymeric clip | Polymeric clip | Surgical stapler | Both groups had comparable safety with no significant differences in complications, ED visits, reinterventions, or mortality; however, polymeric clips were associated with lower implant cost and longer operative time, while the stapler group involved slightly older patients and a nonsignificant increase in complications |
| Miyano et al[13] | Prospective cohort | Japan | Pediatric patients underwent a laparoscopic appendectomy for acute, uncomplicated appendicitis, for which the appendiceal stump was managed with either an endoloop or an endostapler | Endoloop | Endostapler | Loop and stapler techniques showed comparable safety and outcomes across demographic, clinical, and postoperative parameters, with low complication rates managed conservatively; stapling offered slightly shorter anesthesia time but at a significantly higher cost |
| Miyano et al[26] | Prospective cohort | Japan | Pediatric patients underwent a laparoscopic appendectomy for acute, complicated appendicitis, for which the appendiceal stump was managed with either an endoloop or an endostapler | Endoloop | Endostapler | Endostapler is more expensive, but there was no significant difference in morbidity for this technique, particularly with regard to the incidence of postoperative intra-abdominal abscess |
| Naiditch et al[20] | Retrospective cohort | United States | Pediatric patients underwent a laparoscopic appendectomy for acute appendicitis, for which the appendiceal stump was managed with either an endoloop or an endostapler | Endoloop | Endostapler | Endoloop and endostapler showed similar overall complication rates, though superficial wound infections were more frequent with endoloop in nonperforated cases (5.5% vs 0.9%, P = 0.007), while endoloop achieved shorter operative time in perforated appendicitis (52.2 minutes vs 58 minutes, P = 0.047) |
| Parikh et al[27] | Retrospective cohort | United States | Pediatric patients underwent a laparoscopic appendectomy for acute, for which the appendiceal stump was managed with either a looped suture or a stapler | Looped suture | Stapler | In pediatric laparoscopic appendectomy, looped suture and stapler techniques yielded comparable clinical outcomes, but looped suture was significantly more cost-effective, supporting its role as a safe and economical alternative |
| Pogorelić et al[22] | Prospective cohort | Egypt and Croatia | Pediatric patients underwent a laparoscopic appendectomy for acute appendicitis, for which the appendiceal stump was managed with either a polymeric clip or a harmonic stapler | Polymeric clip | Harmonic stapler | Compared with polymeric clips, the clipless technique in pediatric laparoscopic appendectomy was associated with fewer complications, shorter operative time and hospital stay, and less postoperative fever, suggesting a safer and more efficient alternative |
| Pogorelić et al[21] | Prospective cohort | Croatia | Pediatric patients underwent a laparoscopic appendectomy for acute appendicitis, for which the appendiceal stump was managed with either a polymeric clip or an endoloop | Polymeric clip | Endoloop | Polymeric clips provided comparable safety to endoloops in pediatric laparoscopic appendectomy, with similar complication rates but significantly shorter operative time and slightly reduced hospital stay, reflecting greater surgical efficiency |
| Safavi et al[10] | Retrospective cohort | Canada | Pediatric patients underwent a laparoscopic appendectomy for acute appendicitis, for which the appendiceal stump was managed with either an endoloop or an endostapler | Endoloop | Endostapler | In perforated appendicitis, endostapler use was linked to a higher rate of intra-abdominal abscess than endoloop (50% vs 12.7%) and was an independent predictor of abscess formation, while no significant differences were observed between techniques in non-perforated cases |
| Zeineddin et al[9] | Retrospective cohort | United States | Pediatric patients underwent a laparoscopic appendectomy | Endoloop | Stapler | Small bowel obstruction or reoperation after laparoscopic appendectomy is uncommon and mainly predicted by complicated appendicitis, with stapler use not significantly affecting these outcomes, leaving surgeon preference as the primary determinant of stump closure method |
Table 2 presents demographic and economic data from the included studies. Over 50000 pediatric patients were assessed, with interventions including EL, ES, PC, LS, HS, LL, and SU. Participants' ages ranged from 1 to 15 years, with most studies including both sexes. Reported closure costs varied widely, with ES being the most expensive (up to 10329.3 USD for 35788 cases), while PC and EL were more cost-effective in several settings. Follow-up durations ranged from 30 days to over one year.
| Ref. | Intervention | Number | Number of boys | Age (years) | Cost | Follow-up |
| Akbiyik et al[24] | Polymeric clip | 28 | 18 | From 1 to 15 | 40 USD per two clips | 1 week to 1 year |
| Endoloop | 21 | 14 | From 3 to 15 | 121.5 USD per two endoloop | ||
| Akkoyun and Akbiyik[25] | Polymeric clip | 121 | 67 | From 3 to 15 | 10 USD for one clip | 1-23 months |
| Escolino et al[12] | Endostapler | 334 | 267 | 8.9 | 57.836 EUR for supplies | NA |
| Endoloop | 374 | 196 | 10.8 | 91.56 EUR for supplies | ||
| Juan et al[19] | LigaSure | 209 | 116 | 9.7 | NA | 30 days |
| Kocaman et al[23] | LigaSure | 94 | 51 | 12.5 | NA | NA |
| Endoloop | 39 | 18 | 11.4 | |||
| Martinez et al[14] | Polymeric Clip | 17 | 10 | 10.06 | 35.36 USD total closure cost | 30 days |
| Surgical Stapler | 90 | 50 | 11.95 | 375.67 USD total closure cost | ||
| Miyano et al[13] | Endostapler | 81 | 48 | 10.8 | 1296 USD (anesthesia and one stapling set) | NA |
| Endoloop | 75 | 49 | 10.5 | 891 USD (anesthesia and 3 Loops) | ||
| Miyano et al[26] | Endostapler | 31 | 13 | 9.7 | Endostaple set at 550 USD | NA |
| Endoloop | 37 | 15 | 9.1 | Endoloop at 48 USD | ||
| Naiditch et al[20] | Endostapler | 391 | 223 | 9.92 | NA | Median follow-up 15.5 days (range 0–51) for non-perforated; 19.3 days (range 0–135) for perforated |
| Endoloop | 388 | 233 | 9.69 | |||
| Parikh et al[27] | Stapler | 128 | 80 | 12 | 254.58 USD/stapler device | 30 days |
| Looped Suture | 110 | 57 | 12.1 | 40.77 USD/unit | ||
| Pogorelić et al[22] | Polymeric Clip | 197 | 119 | 11 | NA | 30 days |
| Harmonic Scalpel | 115 | 72 | 11 | |||
| Pogorelić et al[21] | Polymeric clip | 101 | 63 | 13 | 17.64 EUR | 1-4 weeks |
| Endoloop | 176 | 84 | 13.5 | 34.16 EUR | ||
| Safavi et al[10] | Endostapler | 24 | NA | 10.58 | 251.68 per ndostapler per case (in Canadian dollars) | NA |
| Endoloop | 208 | 11.55 | 57.57 per Endoloop per case (in Canadian dollars) | |||
| Zeineddin et al[9] | Stapler | 35788 | 21677 | 10.7 | 10329.3 USD for all cases | 30 days |
| Endoloop | 13403 | 8056 | 10.2 | 9569.2 USD for all cases |
The Newcastle-Ottawa Scale assessment of 14 studies evaluating the appendiceal stump closure reveals varied methodological quality. Most studies (10 out of 14) achieved a "moderate quality" rating, scoring 5 or 6 stars, typically missing points in the comparability domain. Four studies were rated "good quality", reflecting strong performance in selection, comparability, and outcome/exposure domains. No study was rated "poor quality". Overall, while all studies demon
| Ref. | Selection (stars; max 4) | Comparability (stars; max 2) | Outcome/exposure (stars; max 3) | Total score (stars; max 9) | Quality rating |
| Akbiyik et al[24] | 4 | 2 | 3 | 9 | Good quality |
| Akkoyun and Akbiyik[25] | 3 | 3 | 6 | Moderate quality | |
| Escolino et al[12] | 4 | 2 | 3 | 9 | Good quality |
| Juan et al[19] | 2 | 1 star | 3 | 6 | Moderate quality |
| Kocaman et al[23] | 3 | 2 | 5 | Moderate quality | |
| Martinez et al[14] | 3 | 2 | 5 | Moderate quality | |
| Miyano et al[13] | 3 | 3 | 6 | Moderate quality | |
| Miyano et al[26] | 3 | 3 | 6 | Moderate quality | |
| Naiditch et al[20] | 3 | 3 | 6 | Moderate quality | |
| Parikh et al[27] | 3 | 3 | 6 | Moderate quality | |
| Pogorelić et al[22] | 3 | 3 | 6 | Moderate quality | |
| Pogorelić et al[21] | 3 | 3 | 6 | Moderate quality | |
| Safavi et al[10] | 3 | 2 | 3 | 8 | Good quality |
| Zeineddin et al[9] | 4 | 2 | 3 | 9 | Good quality |
The network diagram depicts the layout of treatment comparisons among the included studies, where each node represents a specific intervention, and the connecting lines indicate direct comparisons between them; the thickness of each line reflects the number of studies supporting that comparison (Figure 2).
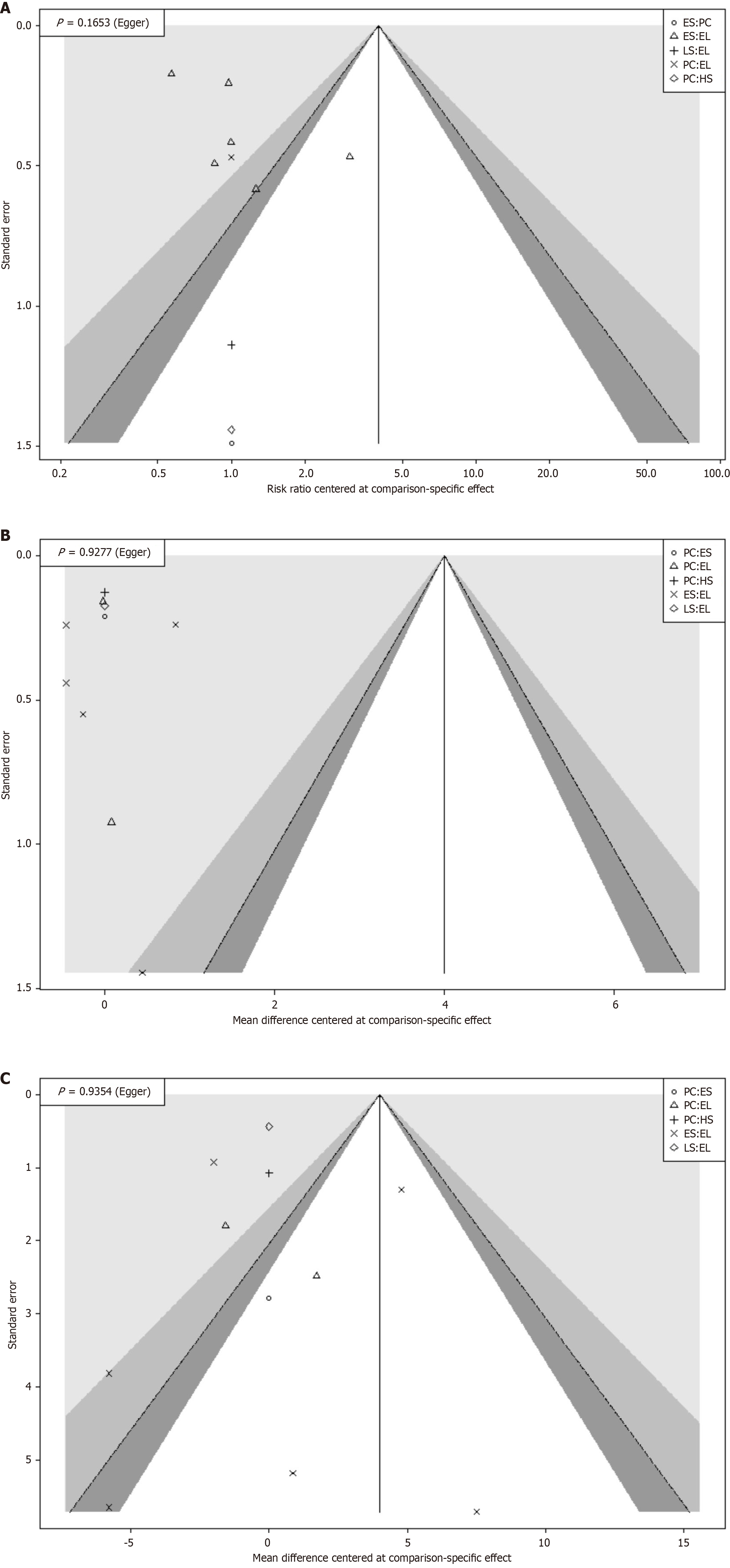
Funnel plot assessments and Egger’s tests indicated minimal publication bias for most outcomes, as the observed symmetry suggested the absence of significant publication bias (Figure 3).
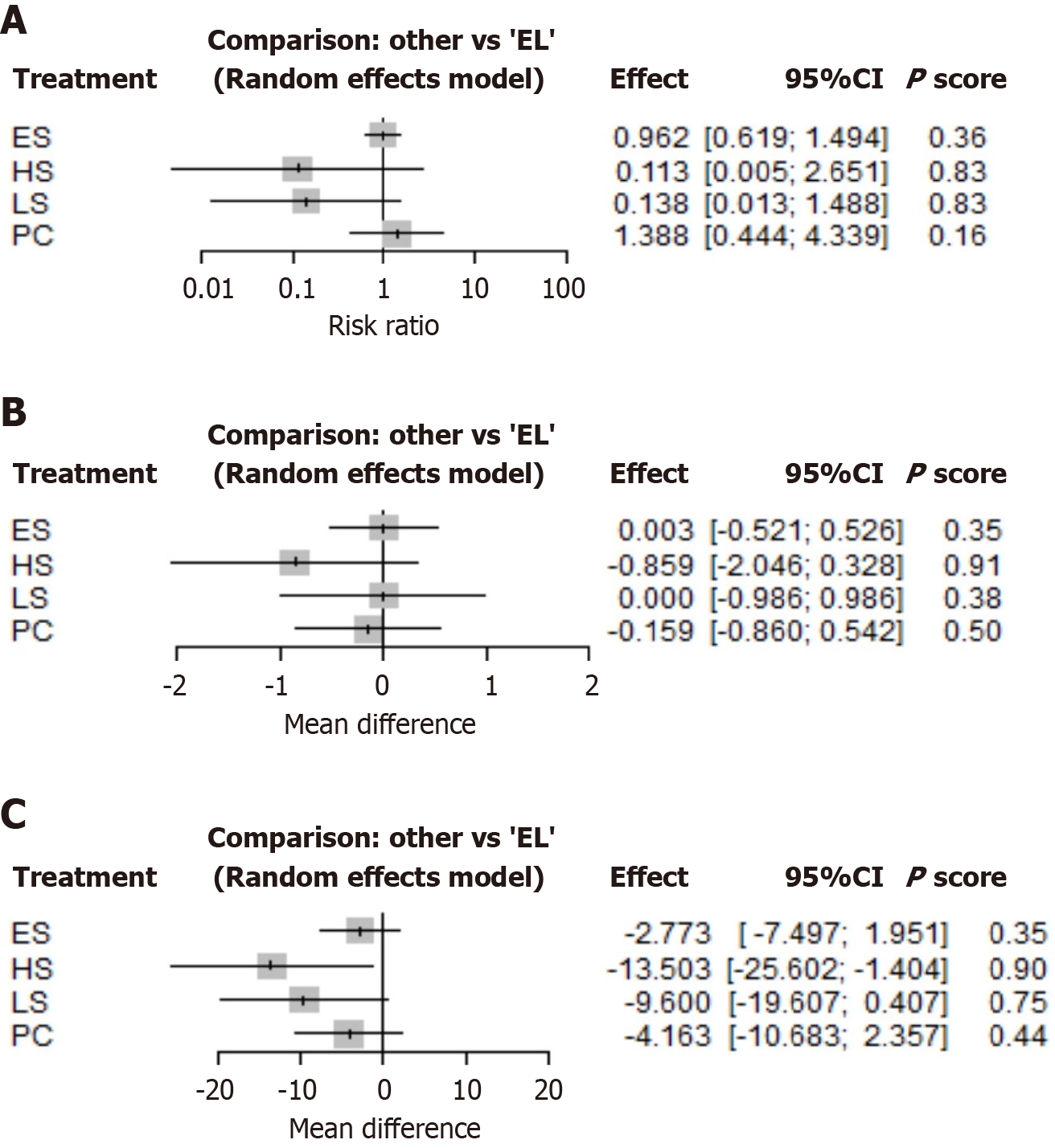
Using a random-effects model, the forest plot compares several treatments (HS, LS, PC, ES) with EL. It reveals that none of the treatments show a statistically significant difference in risk ratio compared to EL, as all 95%CIs cross 1. While HS and LS present the lowest risk ratios (0.113 and 0.138, respectively) and the highest P-scores (0.83), these results are imprecise due to wide confidence intervals, indicating statistical insignificance. PC and ES have risk ratios closer to 1 (1.388 and 0.962, respectively) and lower P-scores (0.16 and 0.36), suggesting a lack of statistical difference from EL. The findings indicate no significant difference in favoring alternative interventions over EL (Figure 4).
The league table presents risk ratios for pairwise comparisons between the treatments EL, ES, HS, LS, and PC, along with their 95%CIs. Most risk ratios span a wide range and frequently include 1.0 within their confidence intervals, indicating no statistically significant difference in risk between treatments. For example, the risk ratio between EL and ES is 1.04 (0.67, 1.62), and between HS and LS is 0.82 (0.02, 42.42), with intervals that reflect considerable imprecision and overlap. Some comparisons, such as EL vs HS [8.85 (0.38, 207.66)], display extensive confidence intervals, signifying high uncertainty and low reliability in the effect estimate. Overall, this league table suggests no consistent or statistically significant risk reduction or increase for any single treatment relative to the others, as evidenced by the frequent inclusion of 1.0 and wide intervals in nearly every comparison (Table 4).
| Endoloop | Endostapler | Harmonic Scalpel | LigaSure | Polymeric clip | ||
| The overall complications (risk ratios) | Endoloop | - | 1.0397 (0.6691; 1.6153) | 8.8503 (0.3772; 207.6631) | 7.2308 (0.6721; 77.7929) | 0.7207 (0.2305; 2.2532) |
| Endostapler | - | - | 8.5127 (0.3549; 204.1865) | 6.9550 (0.6208; 77.9199) | 0.6932 (0.2089; 2.3003) | |
| Harmonic scalpel | - | - | - | 0.8170 (0.0157; 42.4231) | 0.0814 (0.0043; 1.5439) | |
| LigaSure | - | - | - | - | 0.0997 (0.0071; 1.3897) | |
| Polymeric clip | - | - | - | - | - | |
| Length of hospital stays (mean difference) | Endoloop | - | -0.0025 (-0.5263; 0.5212) | 0.8590 (-0.3280; 2.0460) | 0.0000 (-0.9859; 0.9859) | 0.1590 (-0.5422; 0.8603) |
| Endostapler | - | - | 0.8616 (-0.3413; 2.0645) | 0.0025 (-1.1138; 1.1189) | 0.1616 (-0.5663; 0.8895) | |
| Harmonic scalpel | - | - | - | -0.8590 (-2.4020; 0.6840) | -0.7000 (-1.6577; 0.2577) | |
| LigaSure | - | - | - | - | 0.1590 (-1.0508; 1.3689) | |
| Polymeric clip | - | - | - | - | - | |
| Operative time (mean difference) | Endoloop | - | 2.7732 ( -1.9506; 7.4970) | 13.5030 (1.4045; 25.6016) | 9.6000 ( -0.4075; 19.6075) | 4.1630 ( -2.3568; 10.6828) |
| Endostapler | - | - | 10.7299 ( -1.7110; 23.1707) | 6.8268 ( -4.2395; 17.8932) | 1.3899 (-5.7451; 8.5248) | |
| Harmonic scalpel | - | - | - | -3.9030 (-19.6041; 11.7981) | -9.3400 (-19.5315; 0.8515) | |
| LigaSure | - | - | - | - | -5.437 (-17.3809; 6.5070) | |
| Polymeric clip | - | - | - | - | - |
The forest plot comparing the length of hospitalization across treatments relative to EL shows that none of the alternative treatments (ES, HS, LS, PC) result in a statistically significant change in hospital stay duration compared to EL. The mean differences are close to zero, ranging from -0.859 for HS (95%CI: -2.046 to 0.328) to 0.00 for LS (95%CI: -0.986 to 0.986). All 95%CIs cross zero, indicating no significant reduction or increase in length of hospitalization with any treatment. Although HS shows a trend toward a shorter stay (-0.85 days), the wide confidence interval suggests considerable uncertainty. Overall, these findings demonstrate that there is no clear advantage of any alternative interventions over EL in reducing the LOS. The HS had the highest P-score (0.91), followed by PC (0.5; Figure 4).
The league table for length of hospitalization shows that the mean differences between all treatment pairs (EL, ES, HS, LS, and PC) are minor and none are statistically significant, as indicated by 95%CIs that all cross zero. For example, the comparison between EL and ES yields a mean difference of -0.0025 days (95%CI: -0.53 to 0.52), and between HS and LS is -0.86 days (95%CI: -2.4 to 0.68); both reflect substantial uncertainty and no clear advantage for either treatment. Similar patterns are observed across other comparisons, with effect estimates close to zero and confidence intervals indicating no reliable difference. Overall, the findings suggest that none of the treatments significantly reduce or increase hospitalization duration relative to the others, and the evidence is insufficient to recommend one treatment over another based on this outcome (Table 4).
The forest plot comparing operative time shows that all alternative treatments (HS, LS, PC, and ES) are associated with shorter mean operative times compared to EL, with point estimates ranging from -2.77 minutes for ES to -13.5 minutes for HS. Notably, HS demonstrates statistically significant reductions in operative time, as its 95%CIs (HS: -25.6 to -1.404) do not cross zero, suggesting a meaningful decrease in operative duration relative to EL. In contrast, PC and ES have zero confidence intervals (PC: -10.68 to 2.36; ES: -7.5 to 1.95), indicating no statistically significant difference from EL for those groups. Overall, these findings suggest that HS may significantly reduce operative time compared to EL. At the same time, PC, LS, and ES do not show clear evidence of shorter surgical duration. The P-scores further support this pattern, ranking HS higher than PC, LS and ES (Figure 4).
The league table comparing operative time between treatments (EL, ES, HS, LS, PC) shows that, while some treatments appear to have shorter mean operative times than others, the statistical significance of these differences is often limited due to wide confidence intervals. For example, HS is associated with a notably shorter operative time than EL (mean difference: 13.5 minutes, 95%CI: 1.4-25.6), as the confidence intervals do not cross zero, suggesting statistically significant differences. However, many other comparisons, such as ES vs PC (mean difference: 1.39 minutes, 95%CI: -5.75 to 8.52) or PC vs LS (mean difference: -5.437 minutes, 95%CI: -17.38 to 6.5), have confidence intervals that include zero, indicating no significant difference in operative time between those pairs. Overall, the findings suggest that HS consistently reduces operative time compared to EL. Still, the evidence is not strong enough for most other pairwise comparisons to confirm a significant difference, given overlapping confidence intervals (Table 4).
LA has become the standard surgical procedure for treating acute appendicitis in children due to its advantages over open surgery[5]. However, the optimal method for appendiceal stump closure remains a subject of debate[12,14,19]. The technique used is clinically significant, as improper closure has been linked to postoperative complications such as IAA, stump leakage, and SBO[9,12,19].
Multiple techniques are used for stump closure, with EL and ES being the most common. PC and energy-based devices, such as LS and the HS, are also used, but to a lesser extent. The surgeon's preference often guides the choice.
Postoperative complication rates are a central metric in evaluating stump closure methods. However, the findings are inconsistent. Escolino et al[12] reported that EL use in complicated appendicitis was linked to a significantly higher rate of IAA, ileus, and reoperations/readmissions compared to ES. In contrast, Naiditch et al[20] found no significant difference in IAA or SBO between ES and EL. However, they reported a higher rate of superficial wound infections in the EL group. Zeineddin et al[9] similarly found no significant differences were found in SBO or reoperations between stapler and EL groups after adjusting for confounders. Meanwhile, Pogorelić et al[21] found no differences in postoperative complications between EL and PC. Pogorelić et al[22] observed no postoperative complications with HS vs a 5.1% complication rate with PC in a prospective study. Still, the severity of appendicitis, particularly when complicated by perforation or peritonitis, remains a stronger predictor of postoperative outcomes than the closure method itself[9,12,19].
Operative time is another critical factor. Kocaman et al[23] reported that LS reduced surgical time compared to EL. Martinez et al[14] found longer surgeries with PC vs staplers, attributing this to the learning curve of newer tools. Naiditch et al[20], however, observed shorter operative times for EL over ES in perforated cases. Pogorelić et al[22] also showed that the HS reduced operative duration compared to PC. These discrepancies highlight the influence of case complexity and surgeon familiarity.
LOS is frequently assessed as a measure of recovery. Pogorelić et al[21] reported shorter LOS with LS and PC, res
Cost considerations are also important. ES is generally more expensive than EL, with costs reported as 915.60 EUR for ES vs 578.36 EUR for EL in one study[12]. PC has emerged as a cost-effective alternative, with significantly lower implant costs (35.36 USD for PC vs 375.67 USD for SS in Martinez et al[14]; 17.64 EUR for PC vs 34.16 EUR for EL in Pogorelić et al[21]. Although staplers have higher upfront costs, some studies suggest they may be cost-effective in complicated appendicitis due to fewer complications and reduced need for re-intervention[12].
Despite extensive literature, several limitations hinder definitive conclusions. Many studies are retrospective, single-center, and subject to selection bias from surgeon preference[9,12,13,19]. Variability in patient selection (e.g., inclusion of simple vs complicated cases) and inconsistent outcome definitions further complicate comparisons[12,18,20]. Limited generalizability was also noted due to the dominance of a single study[9], which contributed approximately 98% of the total cases, especially as the study is retrospective in nature.
Given these limitations and the variety of techniques in use, network meta-analysis is a valuable tool to synthesize existing evidence. This method allows simultaneous comparison of multiple stump closure methods by combining direct and indirect evidence, offering a more comprehensive understanding of each method’s effectiveness regarding complications, operative time, hospital stay, and cost. Such analysis can resolve conflicting findings and inform surgical decision-making in pediatric LA. While patient-specific factors like stump anatomy and surgeon experience remain critical, robust evidence synthesis is key to optimizing outcome.
HS significantly reduces operative time compared to EL, while no technique shows superiority in postoperative complications or hospital stay. Thus, all methods appear clinically comparable, with efficiency and resource considerations guiding the selection of techniques.
| 1. | Li D, Zhang Z, Wan J, Zhao J, Wei G, Pan W, Yan Y, Zhang Y, Chen F. Clinical features and perforation predictors of appendicitis in infants and toddlers under 3: A retrospective two-center study. Sci Rep. 2025;15:14338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, Boermeester M, Sartelli M, Coccolini F, Tarasconi A, De' Angelis N, Weber DG, Tolonen M, Birindelli A, Biffl W, Moore EE, Kelly M, Soreide K, Kashuk J, Ten Broek R, Gomes CA, Sugrue M, Davies RJ, Damaskos D, Leppäniemi A, Kirkpatrick A, Peitzman AB, Fraga GP, Maier RV, Coimbra R, Chiarugi M, Sganga G, Pisanu A, De' Angelis GL, Tan E, Van Goor H, Pata F, Di Carlo I, Chiara O, Litvin A, Campanile FC, Sakakushev B, Tomadze G, Demetrashvili Z, Latifi R, Abu-Zidan F, Romeo O, Segovia-Lohse H, Baiocchi G, Costa D, Rizoli S, Balogh ZJ, Bendinelli C, Scalea T, Ivatury R, Velmahos G, Andersson R, Kluger Y, Ansaloni L, Catena F. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 697] [Cited by in RCA: 691] [Article Influence: 115.2] [Reference Citation Analysis (109)] |
| 3. | Stringel G, Zitsman JL, Shehadi I, Kithir S. Laparoscopic appendectomy in children. JSLS. 1997;1:37-39. [PubMed] |
| 4. | Bhattacharya K. Kurt Semm: A laparoscopic crusader. J Minim Access Surg. 2007;3:35-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Biondi A, Di Stefano C, Ferrara F, Bellia A, Vacante M, Piazza L. Laparoscopic versus open appendectomy: a retrospective cohort study assessing outcomes and cost-effectiveness. World J Emerg Surg. 2016;11:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 79] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Kumar A, Mustafa MS, Shafique MA, Haseeb A, Rangwala HS, Kumar H, Rangwala BS, Raja A, Raja S, Ali SMS. Comparison of polymeric clip and endoloop in laparoscopic appendectomy: A systematic review and meta-analysis. Surgery. 2024;176:1329-1336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Makaram N, Knight SR, Ibrahim A, Patil P, Wilson MSJ. Closure of the appendiceal stump in laparoscopic appendectomy: A systematic review of the literature. Ann Med Surg (Lond). 2020;57:228-235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Najah Q, Makhlouf HA, Abusalah MA, Aboelkhier MM, Rashed MA, Kashbour M, Awwad SA, Ali FY, Hendi NI, Diab S, Abdallh F, Abozaid AM, Alabdallat YJ. Effectiveness of different appendiceal stump closure methods in laparoscopic appendectomy a network meta-analysis. Langenbecks Arch Surg. 2024;409:270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Zeineddin S, Hu A, Linton S, Zhang V, De Boer C, Raval MV, Abdullah F, Goldstein SD. Association between appendiceal stump closure method and post-operative bowel obstruction after laparoscopic appendectomy. J Pediatr Surg. 2023;58:643-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Safavi A, Langer M, Skarsgard ED. Endoloop versus endostapler closure of the appendiceal stump in pediatric laparoscopic appendectomy. Can J Surg. 2012;55:37-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | White C, Hardman C, Parikh P, Ekeh AP. Endostapler vs Endoloop closure of the appendiceal stump in laparoscopic appendectomy: Which has better outcomes? Am J Surg. 2021;222:413-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Escolino M, Becmeur F, Saxena A, Till H, Holcomb GW 3rd, Esposito C. Endoloop versus endostapler: what is the best option for appendiceal stump closure in children with complicated appendicitis? Results of a multicentric international survey. Surg Endosc. 2018;32:3570-3575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Miyano G, Urao M, Lane GJ, Kato Y, Okazaki T, Yamataka A. A prospective analysis of endoloops and endostaples for closing the stump of the appendix in children. J Laparoendosc Adv Surg Tech A. 2011;21:177-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Martinez C, Drennan C, Vachhrajani S, Aranda A. Safety and Cost Savings Using Polymeric Clips in Appendectomies in the Pediatric Population: Single-Center Experience. J Pediatr Surg. 2023;58:1281-1284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.5. The Cochrane London: Collaboration, 2024. |
| 16. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 50265] [Article Influence: 10053.0] [Reference Citation Analysis (2)] |
| 17. | Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5711] [Cited by in RCA: 14112] [Article Influence: 1411.2] [Reference Citation Analysis (1)] |
| 18. | Gierisch JM, Nieuwsma JA, Bradford DW, Wilder CM, Mann-Wrobel MC, McBroom AJ, Hasselblad V, Williams JW Jr. Pharmacologic and behavioral interventions to improve cardiovascular risk factors in adults with serious mental illness: a systematic review and meta-analysis. J Clin Psychiatry. 2014;75:e424-e440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Juan HL, Nicolas AM, Daniela CL, Lineth OM, María RA, Camila RM, Gabriela TP, Felipe CL, Catalina C. Use of a Bipolar Device (LigaSure) to Seal the Appendiceal Stump in Pediatric Laparoscopic Appendectomy: 10-year Latin-American Experience. J Pediatr Surg. 2023;58:1471-1475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 20. | Naiditch J, Lautz T, Chin A, Browne M, Rowell E. Endoloop as the first line tool for appendiceal stump closure in children with appendicitis. Eur J Pediatr Surg. 2015;25:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Pogorelić Z, Kostovski B, Jerončić A, Šušnjar T, Mrklić I, Jukić M, Jurić I. A Comparison of Endoloop Ligatures and Nonabsorbable Polymeric Clips for the Closure of the Appendicular Stump During Laparoscopic Appendectomy in Children. J Laparoendosc Adv Surg Tech A. 2017;27:645-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Pogorelić Z, Beara V, Jukić M, Rashwan H, Šušnjar T. A new approach to laparoscopic appendectomy in children-clipless/sutureless Harmonic scalpel laparoscopic appendectomy. Langenbecks Arch Surg. 2022;407:779-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 23. | Kocaman OH, Günendi T, Dörterler ME, Boleken ME. Comparison of the Electrothermal Bipolar Sealing System (LigaSure) Versus Endoloop in Pediatric Laparoscopic Appendectomy. J Laparoendosc Adv Surg Tech A. 2022;32:1126-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 24. | Akbiyik F, Senel E, Bayram-Kabacam G, Demirkan H, Atayurt H, Tiryaki T. A comparison of polymer clips and endoloop applications for securing the appendiceal stump during laparoscopic surgery in children. Surg Laparosc Endosc Percutan Tech. 2011;21:349-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Akkoyun I, Akbiyik F. Closing the appendicular stump with a polymeric clip in laparoscopic appendectomy: analysis of 121 pediatric patients. Eur J Pediatr Surg. 2012;22:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Miyano G, Urao M, Lane G, Kato Y, Okazaki T, Yamataka A. Appendiceal stump closure in children with complicated appendicitis: a prospective analysis of endoloops versus endostaples. Asian J Endosc Surg. 2011;4:116-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Parikh PP, Tashiro J, Wagenaar AE, Curbelo M, Perez EA, Neville HL, Hogan AR, Sola JE. Looped suture versus stapler device in pediatric laparoscopic appendectomy: a comparative outcomes and intraoperative cost analysis. J Pediatr Surg. 2018;53:616-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |