INTRODUCTION
Pancreatogenic diabetes, often referred to as type 3c diabetes mellitus, is a distinct subtype of diabetes that results from pancreatic dysfunction. Unlike other forms of diabetes, pancreatogenic diabetes is secondary to pancreatic diseases, including chronic pancreatitis, pancreatic cancer, cystic fibrosis, or pancreatic surgery (Figure 1). Additionally, pancreatogenic diabetes can develop following acute pancreatitis, cystic fibrosis, and hereditary chronic pancreatitis, which are associated with distinct disease courses and, in the case of hereditary chronic pancreatitis, a higher frequency of pancreatic cancer. It accounts for a significant but often overlooked portion of the diabetes burden, especially in patients with chronic pancreatic diseases. Recent epidemiological studies indicate that up to 12% of all diabetes cases in Western populations are classified as pancreatogenic diabetes, with an even higher prevalence in cohorts with chronic pancreatitis or pancreatic cancer[1,2]. Additionally, the prevalence of pancreatogenic diabetes in patients with chronic pancreatitis can be as high as 60%, a statistic that underscores the need for increased awareness and early diagnosis in these high-risk groups[3-5]. The association between pancreatogenic diabetes and pediatric populations has also been noted, although the incidence is lower compared to adults[6]. Recent studies have explored the mechanisms and risk factors contributing to pancreatogenic diabetes in these diverse populations, with findings suggesting that both acute and chronic pancreatitis, as well as cystic fibrosis, play significant roles in its development[7,8]. Despite its clinical importance, pancreatogenic diabetes is frequently underdiagnosed or misclassified as type 2 diabetes due to the similarity in symptoms and lack of awareness regarding the distinct pathophysiological mechanisms at play.
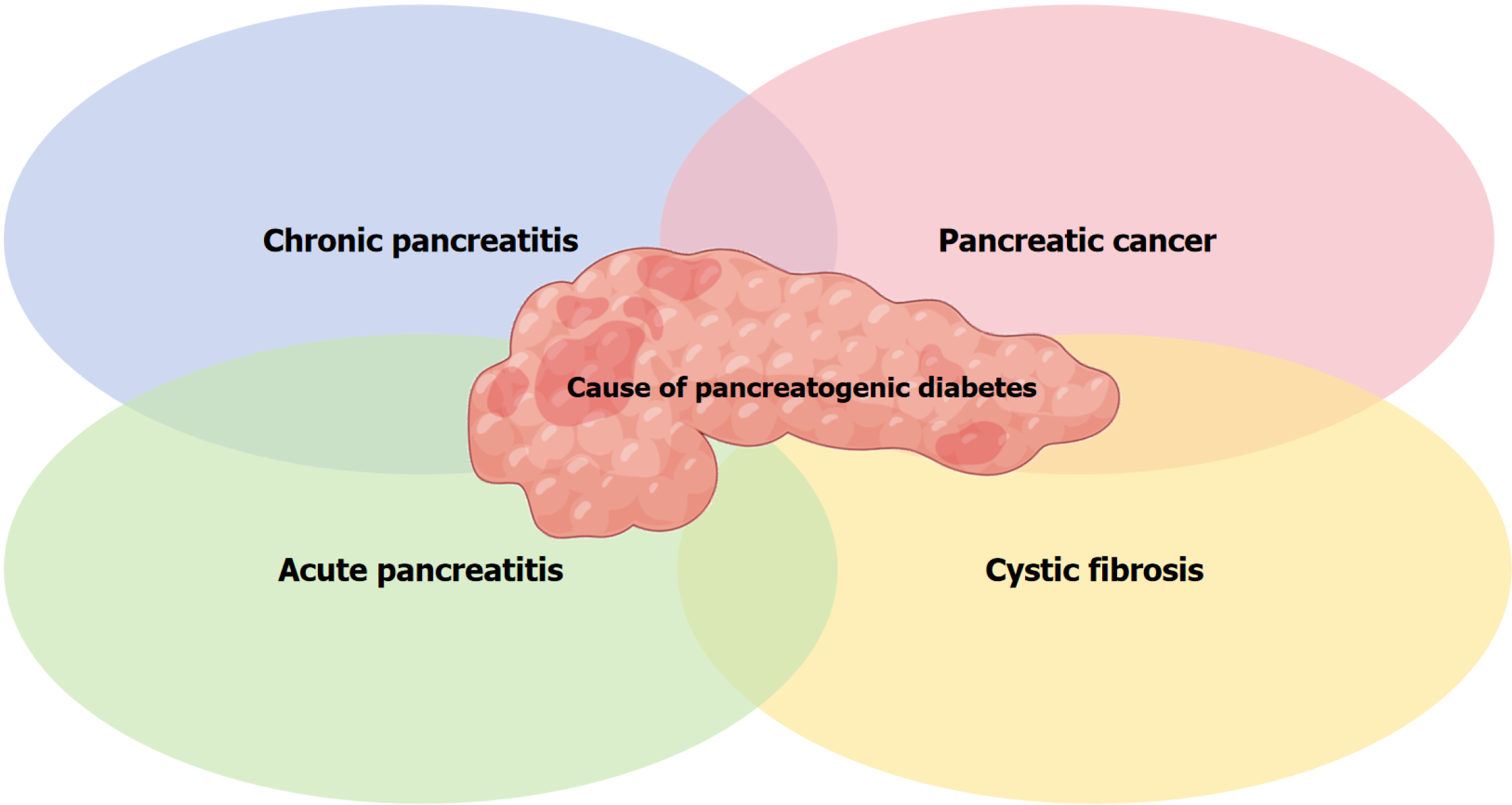
Figure 1 Causes of pancreatogenic diabetes.
This Venn diagram illustrates the various causes of pancreatogenic diabetes, including chronic pancreatitis, pancreatic cancer, acute pancreatitis, and cystic fibrosis.
The pathophysiology of pancreatogenic diabetes is multifaceted, involving both endocrine and exocrine pancreatic dysfunction. Endocrine dysfunction arises from the progressive loss of insulin-producing beta cells in the islets of Langerhans, while exocrine insufficiency is due to the impairment of the pancreas’ ability to secrete digestive enzymes. These dual factors lead to disturbances in both glucose homeostasis and nutrient absorption. The resulting condition is characterized by a combination of insulin deficiency, glycemic instability, malnutrition, and increased risk of complications such as infections, cancer, and pancreatic insufficiency[9,10]. Moreover, the pathophysiology of this form of diabetes is often compounded by oxidative stress, inflammation, and other metabolic disturbances that contribute to glycemic variability and poor overall control.
PATHOPHYSIOLOGY
The development of pancreatogenic diabetes involves several interconnected mechanisms that begin with pancreatic damage. One of the earliest events is the destruction of pancreatic beta cells due to chronic inflammation or tumor invasion. This leads to a significant reduction in insulin secretion, which is a hallmark feature of diabetes. However, the pathogenesis of pancreatogenic diabetes is not limited to beta-cell destruction alone; there is also a dysfunction of glucagon-secreting alpha cells, which normally function to regulate blood glucose levels in response to hypoglycemia[11]. Unlike type 2 diabetes, where α-cell dysfunction is primarily qualitative, characterized by an impaired response to glucose and other regulatory signals, the dysfunction in pancreatogenic diabetes is both qualitative and quantitative. In pancreatogenic diabetes, there is a more pronounced impairment in α-cell function, leading to an inability to appropriately regulate blood glucose during both hyperglycemic and hypoglycemic events. Recent studies have shown that beta-cell area loss in pancreatogenic diabetes can reach up to 70%, which reflects more recent findings and a broader understanding of the degree of pancreatic beta-cell destruction. This combined defect in both insulin and glucagon secretion results in unstable blood glucose levels, with patients frequently experiencing episodes of both hyperglycemia and hypoglycemia.
In addition to endocrine dysfunction, exocrine pancreatic insufficiency contributes to the pathophysiology of pancreatogenic diabetes. The pancreas is not only responsible for insulin secretion but also for the production of digestive enzymes. When the exocrine function is compromised, as in chronic pancreatitis, patients suffer from maldigestion and malabsorption of essential nutrients. This exacerbates nutritional deficiencies, which further complicate the management of diabetes. The metabolic disturbances caused by inadequate enzyme secretion and nutrient absorption can lead to weight loss, muscle wasting, and the exacerbation of glycemic control issues[12].
Furthermore, the involvement of oxidative stress, inflammation, and lipid metabolism in the disease process is becoming increasingly recognized. Inflammatory mediators, including cytokines, play a significant role in the progression of pancreatic damage and the worsening of insulin resistance[4]. Additionally, metabolic disturbances such as altered lipid profiles and fatty acid dysregulation are observed in pancreatogenic diabetes patients, which contribute to the pathophysiological complexity of the disease and its variability in clinical presentations[13].
DIAGNOSTIC CHALLENGES AND STRATEGIES
The diagnosis of pancreatogenic diabetes remains challenging due to its overlapping features with type 1 and type 2 diabetes, as well as the lack of clear diagnostic criteria. Many patients with pancreatogenic diabetes present with symptoms that resemble type 2 diabetes, such as polyuria, polydipsia, and weight loss. However, unlike type 2 diabetes, which is primarily associated with insulin resistance and beta-cell dysfunction, pancreatogenic diabetes is caused by pancreatic damage leading to a combination of insulin deficiency and exocrine insufficiency[14].
Currently, there is no universally accepted diagnostic protocol for pancreatogenic diabetes. As a result, many patients are misdiagnosed, leading to suboptimal management. The most common diagnostic approaches include a thorough clinical history, which should include a detailed assessment of the patient’s history of pancreatitis, pancreatic surgery, or other pancreatic diseases. Imaging studies such as computed tomography, magnetic resonance imaging, or endoscopic ultrasound can help identify structural changes in the pancreas, such as calcifications or tumors, that are indicative of pancreatogenic diabetes[15]. Additionally, biochemical tests, including C-peptide levels and fecal elastase, are commonly used to assess beta-cell function and exocrine insufficiency, respectively.
Mixed meal tolerance tests have been suggested as a useful tool to differentiate pancreatogenic diabetes from other types of diabetes. The mixed meal tolerance tests assesses both insulin secretion and glucose tolerance in response to a standardized meal, providing a comprehensive view of pancreatic function[15]. However, these tests are not widely available and require specialized equipment, which limits their practical application in clinical settings. The need for better diagnostic markers and more accessible tests remains a critical gap in the diagnosis of pancreatogenic diabetes.
TREATMENT AND CLINICAL MANAGEMENT
The treatment of pancreatogenic diabetes requires an individualized approach that addresses both endocrine and exocrine deficiencies. The cornerstone of management is insulin therapy, as most patients exhibit significant insulin deficiency due to beta-cell loss. Insulin therapy must be tailored to each patient’s specific needs, with a focus on preventing both hyperglycemia and hypoglycemia. Insulin regimens often involve a combination of long-acting and rapid-acting insulin to mimic normal pancreatic function and maintain tight glucose control[2].
In addition to insulin therapy, pancreatic enzyme replacement therapy (PERT) is critical for managing exocrine insufficiency. PERT helps to replace the digestive enzymes that are deficient in patients with chronic pancreatitis or pancreatic cancer. A typical dosing range for PERT is 40000-50000 units of lipase per meal and 20000 units per snack, adjusted based on the patient’s individual nutritional and digestive needs. By improving nutrient absorption, PERT can reduce symptoms of malnutrition and improve glycemic control, as better nutritional status can enhance insulin sensitivity[10,16]. While glucagon-like peptide 1 receptor agonists and dipeptidyl peptidase-4 inhibitors are commonly used in the treatment of type 2 diabetes, their role in pancreatogenic diabetes remains limited. These agents have shown minimal efficacy in improving glycemic control in patients with pancreatic dysfunction, likely due to the complex interplay of both endocrine and exocrine pancreatic insufficiency. Therefore, their use is not generally recommended for managing pancreatogenic diabetes.
Nutritional support is another essential aspect of managing pancreatogenic diabetes. Since patients with this condition often suffer from maldigestion, they may require vitamin and mineral supplementation, as well as adjustments to their diet to accommodate impaired absorption. Particular attention should be paid to fat-soluble vitamins, including vitamin A, D, E, and K, which are often deficient due to exocrine pancreatic insufficiency. These vitamins require regular monitoring and supplementation to prevent deficiencies and associated complications such as bone disorders (vitamin D), night blindness (vitamin A), and coagulopathy (vitamin K). A diet high in easily digestible nutrients and low in fats may help alleviate some of the malabsorption symptoms and prevent further complications[17]. Lifestyle modifications, particularly alcohol and smoking cessation, are strongly recommended for patients with pancreatogenic diabetes, as these factors can exacerbate pancreatic damage and worsen both exocrine and endocrine function[12]. Additionally, weight management through a balanced diet and regular physical activity can help mitigate insulin resistance and improve overall glycemic control.
EPIDEMIOLOGY AND RISK FACTORS
Epidemiological data show that pancreatogenic diabetes is most commonly seen in patients with chronic pancreatitis, pancreatic cancer, or those who have undergone pancreatic surgery. In these populations, the cumulative incidence of pancreatogenic diabetes can be as high as 60%, significantly greater than in the general population[18,19]. This figure refers to the cumulative incidence observed over the course of the disease, reflecting the long-term risk for patients with chronic pancreatitis and pancreatic cancer. The risk of developing pancreatogenic diabetes increases with the duration of chronic pancreatitis and the severity of exocrine insufficiency. Furthermore, lifestyle factors such as alcohol abuse and smoking significantly elevate the risk, underscoring the need for early identification and intervention in at-risk populations[20,21]. Gender and socioeconomic status (SES) differences in the incidence of pancreatogenic diabetes are influenced by both biological and socio-behavioral factors. Biologically, gender differences may stem from hormonal variations, which can affect insulin resistance and pancreatic function. Socio-behavioral drivers, such as access to healthcare, SES, and lifestyle factors, play a critical role in the disparities observed, as individuals in lower SES groups may have higher exposure to risk factors like smoking and alcohol consumption. Geographic and demographic variations in the prevalence of pancreatogenic diabetes are also important considerations. Studies have shown that the condition is more prevalent in men and among individuals of lower SES. Racial and ethnic disparities are evident, with higher rates of pancreatogenic diabetes observed in populations with high rates of chronic pancreatitis[17,22]. These differences highlight the need for targeted screening and personalized care in diverse patient populations.
CONCLUSION
Pancreatogenic diabetes is a complex and often underdiagnosed condition that arises as a result of pancreatic exocrine and endocrine dysfunction. Its diagnosis is challenging, and current methods lack standardization, leading to frequent misclassification as type 1 or type 2 diabetes. Management involves a multifaceted approach, including insulin therapy, pancreatic enzyme replacement, and nutritional support. Long-term monitoring for glycemic control, hypoglycemia, and pancreatic cancer surveillance is critical for improving patient outcomes. Further research is needed to establish clearer diagnostic criteria, more effective treatment protocols, and better epidemiological data, particularly in diverse populations, to ensure optimal care for individuals with pancreatogenic diabetes.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade A, Grade B, Grade B, Grade B
Novelty: Grade A, Grade B, Grade B, Grade C
Creativity or Innovation: Grade A, Grade B, Grade B, Grade C
Scientific Significance: Grade A, Grade A, Grade B, Grade C
P-Reviewer: Chen JY, Researcher, China; Dąbrowski M, MD, PhD, Associate Professor, Poland S-Editor: Wu S L-Editor: A P-Editor: Wang WB