Published online Jan 15, 2026. doi: 10.4239/wjd.v17.i1.110528
Revised: September 19, 2025
Accepted: November 12, 2025
Published online: January 15, 2026
Processing time: 220 Days and 1.9 Hours
Prediabetes increases the risk of cardiovascular and cerebrovascular mortality. This study examines the relationship between prediabetes and mortality in post-stroke patients.
To determine whether prediabetes is associated with increased post-stroke mortality in adults with acute ischemic stroke (IS).
A systematic search was conducted in PubMed/MEDLINE, Scopus, and Google Scholar databases until May 2023 to identify relevant articles reporting on the association of prediabetes with IS mortality. A random-effects model was used to calculate odds ratio (OR), heterogeneity was assessed using I2 statistics, and sensitivity analysis was performed using the leave-one-out method.
Our analysis of 11 studies included 84833 prediabetic patients with a mean follow-up time of 20.9 months. The prediabetes cohort comprised patients of an average age of 67 years from various countries, including Korea, Italy, Japan, China, Spain, and the Netherlands. Although, the unadjusted analysis showed no significant association between prediabetes and post-stroke mortality (OR = 1.06, 95%CI: 0.51-2.19) with high heterogeneity (I2 = 94.7%,
Our findings suggest that prediabetes is associated with a nearly 68% higher mortality risk following a stroke. Thereby warranting more prospective studies with prediabetes to validate these findings.
Core Tip: This meta-analysis synthesizes 11 studies (> 84000 participants) evaluating whether prediabetes is associated with mortality after acute ischemic stroke. Unadjusted results were heterogeneous; however, adjusted analyses showed a significant association between prediabetes and higher poststroke mortality. These findings support early identification of prediabetes after stroke and emphasize rigorous secondary prevention while definitive interventional studies are pursued.
- Citation: Patel B, Mahajan K, Mahadevan A, Trivedi R, Dhingra A, Brar SS, Dixit S, Desai R. Association between prediabetes and higher risk of mortality following acute ischemic stroke: A meta-analysis. World J Diabetes 2026; 17(1): 110528
- URL: https://www.wjgnet.com/1948-9358/full/v17/i1/110528.htm
- DOI: https://dx.doi.org/10.4239/wjd.v17.i1.110528
Prediabetes is a metabolic condition that falls between normal glucose metabolism and diabetes. It includes impaired fasting glucose, impaired glucose tolerance, and impaired hemoglobin A1c (HbA1c). According to current guidelines, impaired plasma glucose (PG) is defined as fasting PG (FPG) of 6.1-6.9 mmol/L (110-125 mg/dL) as per World Health Organization, whereas American Diabetes Association defines it as the cutoff of 5.6-6.9 mmol/L (100-125 mg/dL)[1]. The prevalence of prediabetes among individuals who have experienced an ischemic stroke (IS) or transient ischemic attack but do not have diabetes ranges from 23% to 53%[2-4].
It is important to note that several studies indicate prediabetes may have varying impacts on different types of vascular diseases, such as ischemic heart disease, IS, and hemorrhagic stroke. This suggests either heterogenous prediabetic states or various mechanisms through which abnormal blood glucose levels contribute to each vascular event. Individuals diagnosed with pre-diabetes exhibit similar vascular risk factors to those found in people with type 2 diabetes (hypertension, dyslipidemia, dysglycemia, obesity, sedentary lifestyle, insulin resistance, pro-coagulation, endothelial dysfunction, and inflammation). These risk factors place pre-diabetics at a heightened risk of vascular complications[5-7]. Additionally, limited research has been conducted to explore the connection between prediabetes and concrete outcomes, specifically the mortality risk associated with each subtype of vascular disease.
Understanding the association between pre-diabetes and mortality following acute IS (AIS) is crucial for better prognostication and patient management. Several individual studies have investigated the relationship between pre-diabetes and post-AIS mortality, with varying and sometimes conflicting results. According to the findings of Kamouchi et al[8], glycemic control status (assessed by HbA1c levels) before a stroke has been linked to unfavorable outcomes within the first 24 hours of hospitalization for AIS.
A systematic review and meta-analysis of the available evidence can offer a more comprehensive assessment of this association by combining data from multiple studies, increasing statistical power, and reducing biases. In this research publication, we present a meta-analysis of relevant prospective and observational studies investigating the potential link between pre-diabetes and mortality in patients who have experienced AIS to understand the association between the two better.
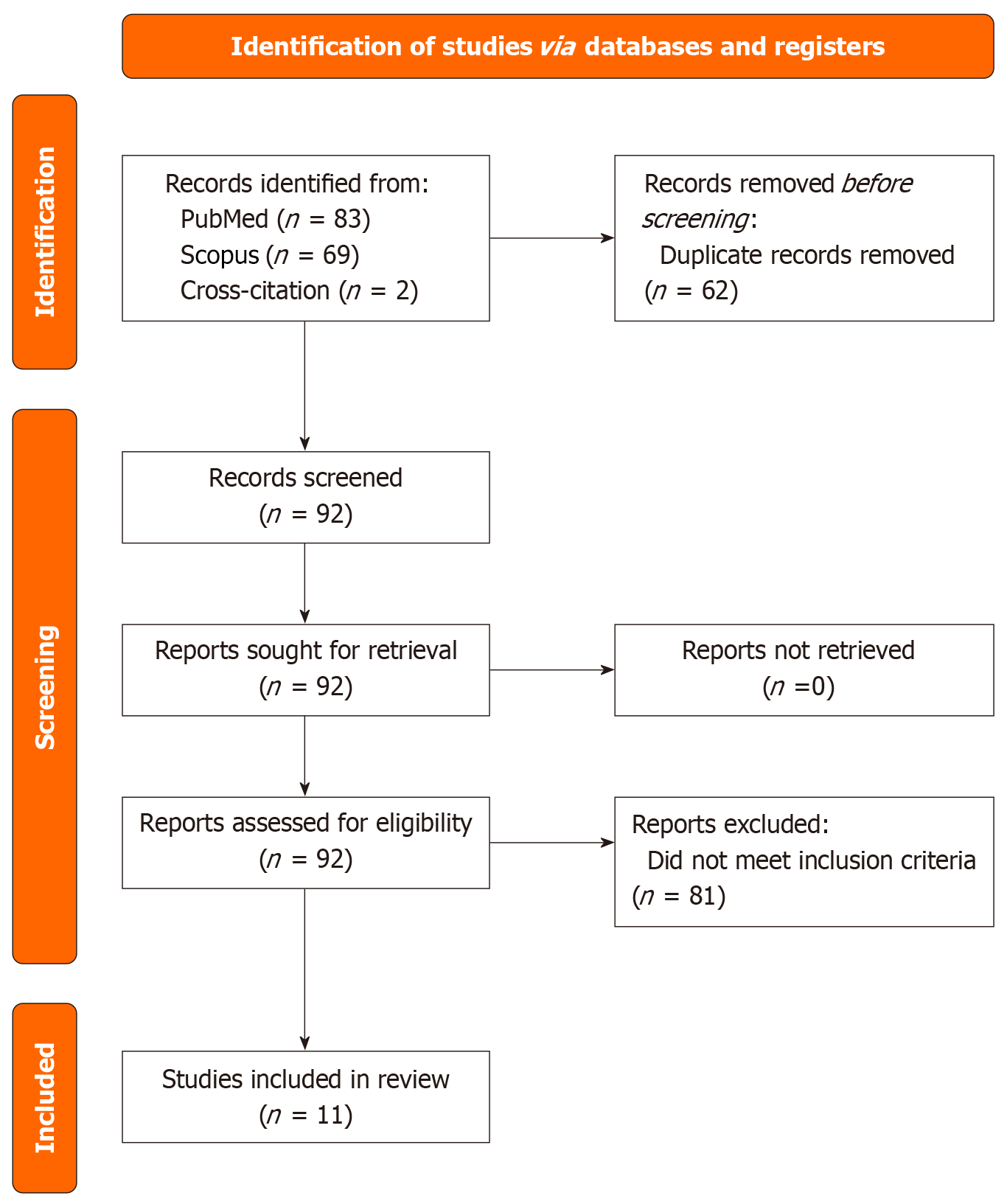
This meta-analysis was conducted per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (Figure 1). A search was performed using PubMed, Scopus, and Google Scholar from 2013 to 2023 using the following keywords, including “impaired fasting glucose”, “impaired glucose tolerance”, “elevated blood sugar”, “prediabetes”, “insulin resistance”, “elevated HbA1c”, “ischemic stroke”, “cerebral infarction”, “ischemic brain injury”, “ischemic cerebrovascular accident”, and “mortality”. Reference lists of relevant studies were also manually searched. Studies were included if they involved patients with prediabetes diagnosed with an IS and reported clinical outcomes, including mortality. Systematic reviews, meta-analyses, editorials, comments, news, guidelines, case reports, and non-English publications were excluded. Studies reporting incomplete or insufficient data on demographics or clinical outcomes were also excluded. In cases where multiple studies reported on the same cohort of patients, only the study with the most comprehensive data set was included.
Two independent reviewers screened the studies for eligibility, and a third reviewer was consulted in cases of uncertainty. The following data were extracted from studies that met the inclusion criteria: (1) First author name; (2) Publication year; (3) Country of study; (4) Study design; (5) Number of participants in each group; (6) Participant age and sex; (7) Racial demographics; (8) Assessed primary and secondary outcomes; (9) Median follow-up duration; and (10) Unadjusted and adjusted risk for mortality with adjusted variables. Any discrepancies between the two reviewers were resolved through discussion and consensus.
The JBI tool was used to assess the quality of the included studies. This tool evaluates the risk of bias in each study based on standardized criteria. Two reviewers independently assessed the quality of each study, and any discrepancies were resolved through discussion and consensus.
The primary outcome was the mortality risk in prediabetic AIS patients. A binary random-effects model was used to combine the effect sizes of the included studies, and the results were presented as forest plots. I2 statistics assessed the effect size heterogeneity across the different studies. Leave-one-out sensitivity analyses were conducted to explore the influence of individual studies on the overall effect size estimate. P < 0.05 was used to define statistical significance.
In our meta-analysis, we synthesized data from 11 primary studies to evaluate the impact of prediabetes on mortality in stroke patients (Table 1)[2,3,9-17]. A comprehensive search across PubMed, Scopus, Google Scholar, and cross-citation from 2013 to 2023 yielded 154 studies. After removing duplicates (n = 62), 92 studies were assessed in total, culminating in including four case-control and seven cohort studies. These studies encompassed 84833 prediabetic patients with an average follow-up period of 20.9 months. The average age of the patients was 67, drawn from diverse countries, including Korea, Italy, Japan, China, Spain, and the Netherlands. Notably, the study by Kim et al[13] contributed to the majority of patients, totaling 81875.
| Ref. | Type of study | Total sample size (n) | Sample size (n): Prediabetics with ischemic stroke | Age (years) (mean ± SD) | Male sex | Median follow-up (months) | Definition of prediabetes | |
| n | % | |||||||
| Tanaka et al[3], 2013, Japan | Cohort | 116 | 52 | 67.8 ± 11.7 | 36 | 69.2 | 1 | FPG ≤ 126 mg/dL; oral glucose tolerance test: 140-199 mg/dL |
| Jia et al[11], 2014, China | Cohort | 926 | 439 | 63.2 ± 12.6 | 290 | 66.1 | 12 | FPG: 6.1-7.0 mmol/L and 2-hour post-prandial glucose: 7.8-11.1 mmol/L |
| Roquer et al[15], 2014, Spain | Case-control | 1088 | 273 | 771 | 135 | 49.5 | 3 | PG: 5.7-6.4 mmol/L |
| Wu et al[16], 2014, China | Case-control | 1810 | 507 | 63 ± 12 | 331 | 65.3 | 12 | HBA1c < 5.5% and 5.5%-6.1% |
| Ernaga Lorea et al[2], 2017, Spain | Cohort | 255 | 72 | 73.91 | 148 | 58 | 30 | HBA1c: 5.7%-6.4% |
| Kim et al[13], 2017, South Korea | Cohort | 499239 | 81875 | 49.7 ± 11.92 51.3 ± 12.23 | - | 60.72 64.93 | 132 | PG: 100-125 mg/dL |
| Osei et al[14], 2017, Netherlands | Case-control | 1007 | 176 | 65 ± 14 | - | - | - | PG: 5.6-6.9 mmol/L |
| Zhu et al[17], 2017, China | Cohort | 3882 | 412 | 63.1 ± 10.8 | 270 | 65.5 | 3 | PG: 6.1-7.0 mmol/L |
| Ago et al[9], 2018, Japan | Case-control | 4655 | 4655 | 70.3 ± 12.4 | 2962 | 63.5 | 3 | - |
| Forti et al[10], 2020, Italy | Cohort | 2662 | 830 | 79 (71-85)1 | 360 | 43.4 | 1 | HBA1c: 5.7%-6.4% |
| Kim et al[12], 2021, South Korea | Cohort | 661 | 197 | 68.7 ± 12.6 | 115 | 58.4 | 12 | HBA1c: 5.7%-6.4% |
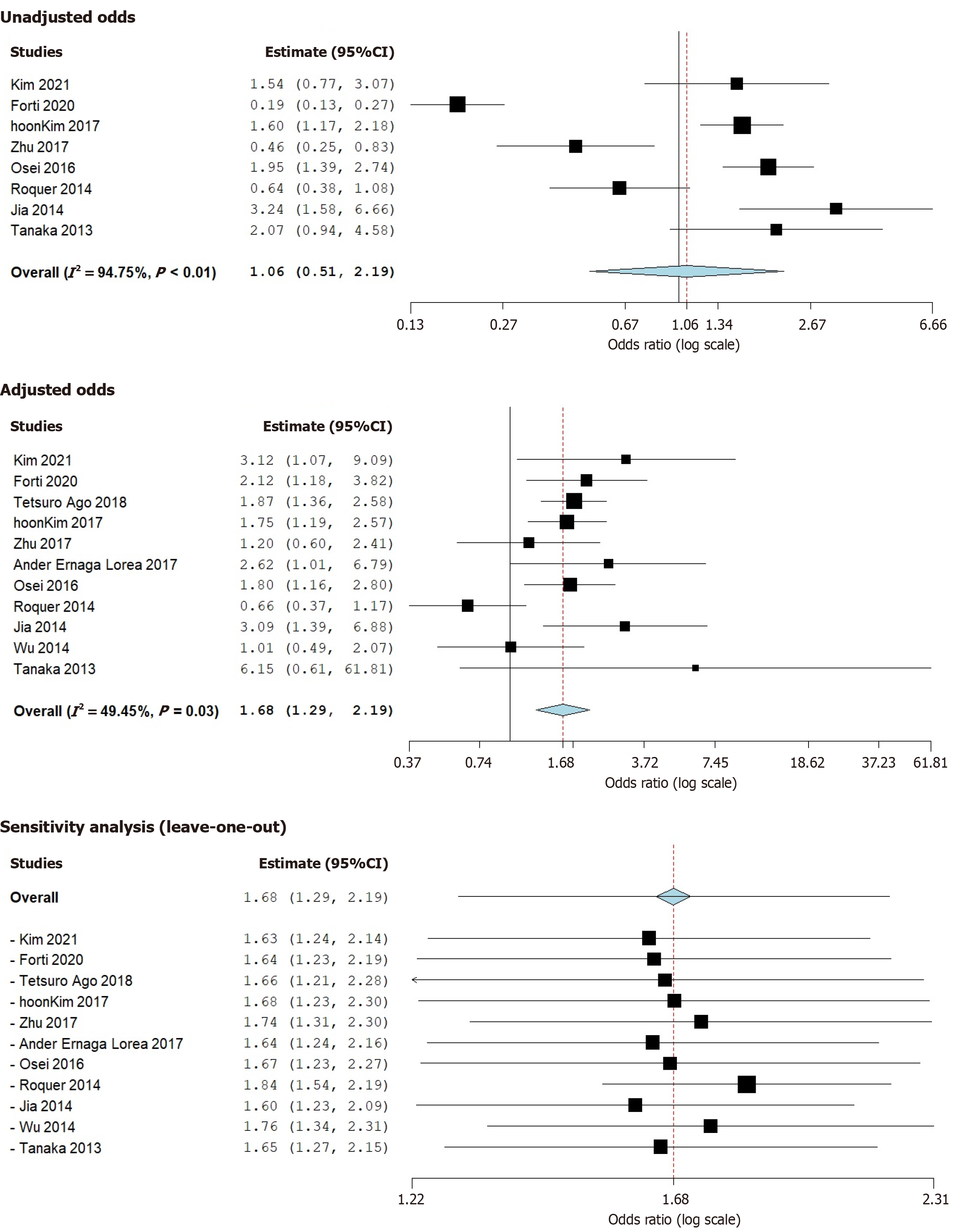
Our analysis focused on the all-cause mortality risk associated with prediabetes in stroke patients. We observed a minor elevation in unadjusted risk from the eight studies incorporating 84254 patients[3,10-15,17]. This increase, however, was not statistically significant [odds ratio (OR) = 1.06, 95%CI: 0.51-2.19, P = 0.88] but exhibited high heterogeneity (I2 = 94.75%, P < 0.01). The weights of the studies were relatively consistent, with values between 11.63% and 13.18%.
When we adjusted for baseline characteristics and comorbidities across all eleven studies (n = 84833)[2,3,9-17], prediabetic stroke patients displayed a considerably increased post-stroke mortality risk (adjusted OR = 1.68, 95%CI: 1.29-2.19, P < 0.01). This adjusted analysis showed moderate heterogeneity (I2 = 49.45%, P = 0.03). Among the studies, weights varied, with the smallest being 1.23% (Tanaka et al[3]) and the largest being 16.01% (Ago et al[9]). The findings were also validated with a leave-one-out sensitivity analysis (Figure 2)[2,3,9-17].
The close relationship between prediabetes and post-AIS mortality necessitates careful attention due to its implications on patient care and clinical prognosis. With hyperglycemia frequently presenting in individuals with cerebrovascular disease, regardless of their diabetic status, the significance of this relationship cannot be understated[18]. Moreover, the high incidence of prediabetes in stroke patients further emphasizes its role as a considerable risk factor for cerebrovascular mortality[12,15,19]. Recent literature suggests a correlation between prediabetes and an elevated risk of stroke recurrence[20], as well as detrimental functional outcomes associated with hyperglycemia during the acute phase of stroke[21].
Our meta-analysis underscores prediabetes as a significant precursor to increased mortality risk post-stroke, revealing a heightened risk of 68% during an average follow-up span of 20.9 months. These results align with prior studies, reinforcing that prediabetes significantly influences post-stroke mortality risk. Including data from multiple countries in our research bolsters its external validity.
It is imperative to recognize prediabetes as a pivotal risk factor. This acknowledgment empowers healthcare practitioners to tailor their therapeutic strategies more effectively, aiming to diminish the fatal outcomes that follow a stroke. Notably, while the Stroke Hyperglycemia Insulin Network Effort had demonstrated that intensive glucose management during acute stroke did not affect outcomes at 90 days[22], it's essential to emphasize that the enduring risk posed by prediabetes, mainly its association with long-term mortality, remains substantial, as underscored by our findings. A contemporary study also identified prediabetes as a determinant for high on-treatment platelet reactivity, impacting the efficacy of antiplatelet agents such as Jia et al[23]. Thereby highlighting the potential for precise changes to post-stroke management for prediabetic patients.
Moreover, our results underscore the urgency for proactive lifestyle interventions and preventive initiatives regarding prediabetes. Achieving ideal glycemic control and stringent preventive actions form a holistic approach to improving clinical outcomes. Such strategies also have the potential to curtail the economic strain on healthcare infrastructures, especially concerning stroke interventions in vulnerable groups. Additionally, identifying prediabetes after AIS may help flag patients for closer followup and rigorous secondary prevention. While intensive inpatient glucose-lowering has not improved short-term functional outcomes, targeted riskfactor management and pragmatic trials focused on prediabetic subgroups could clarify whether tailored interventions improve survival.
This meta-analysis presents notable strengths. It comprehensively evaluates the link between prediabetes and post-stroke mortality by drawing from a large sample size across diverse studies, enhancing statistical power and overall generalizability. Moreover, including studies from various geographical regions ensures the findings' applicability across healthcare contexts. The use of the leave-one-out sensitivity analysis further confirms the robustness of our conclusions.
However, this study is not without limitations. There is evident heterogeneity among the included studies, which may impact the collective results. Definitions of prediabetes varied across included studies (FPG, oral glucose tolerance, and/or HbA1c thresholds). Such variability likely contributed to between-study heterogeneity, particularly in the unadjusted analyses. Differences in study design, case mix, geography/ethnicity, and followup may further explain dispersion. By contrast, adjusted estimates – accounting for baseline imbalances – showed a more consistent association with mortality, supporting their greater clinical interpretability.
One study contributed a disproportionately large portion of participants, which may influence pooled estimates despite the leave-one-out sensitivity analysis. This dominance highlights the need for additional large, well-adjusted cohorts to validate the observed association. Key data elements were unavailable or inconsistently reported across studies, including stroke severity (e.g., National Institutes of Health Stroke Scale scores), acute treatments, and adherence to secondary prevention. Study designs were predominantly observational, leaving room for residual confounding and selection biases despite adjusted analyses. These factors should temper causal inference. Furthermore, the analysis does not explore the specific mechanisms connecting prediabetes with increased post-stroke mortality, highlighting an area for future research.
Our meta-analysis establishes a significant association between prediabetes and heightened post-AIS mortality risk, with prediabetic patients exhibiting a 68% increased mortality risk during an average follow-up of 20.9 months. These findings accentuate the critical role of prediabetes as a determinant in post-stroke outcomes, emphasizing the need for clinicians to tailor their therapeutic strategies and engage in proactive preventive measures. Recognizing and addressing prediabetes could enhance patient prognosis and reduce healthcare burdens. While a diverse and extensive data set reinforces the study, it underscores the necessity for further research to elucidate the specific mechanisms driving this association.
| 1. | Bansal N. Prediabetes diagnosis and treatment: A review. World J Diabetes. 2015;6:296-303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 276] [Cited by in RCA: 344] [Article Influence: 31.3] [Reference Citation Analysis (13)] |
| 2. | Ernaga Lorea A, Hernández Morhain MC, Ollero García-Agulló MD, Martínez de Esteban JP, Iriarte Beroiz A, Gállego Culleré J. Prognostic value of blood glucose in emergency room and glycosylated hemoglobin in patients who have suffered an acute cerebro-vascular event. Med Clin (Barc). 2017;149:17-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Tanaka R, Ueno Y, Miyamoto N, Yamashiro K, Tanaka Y, Shimura H, Hattori N, Urabe T. Impact of diabetes and prediabetes on the short-term prognosis in patients with acute ischemic stroke. J Neurol Sci. 2013;332:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Osei E, den Hertog HM, Berkhemer OA, Fransen PS, Roos YB, Beumer D, van Oostenbrugge RJ, Schonewille WJ, Boiten J, Zandbergen AA, Koudstaal PJ, Dippel DW; MR CLEAN pretrial investigators. Increased admission and fasting glucose are associated with unfavorable short-term outcome after intra-arterial treatment of ischemic stroke in the MR CLEAN pretrial cohort. J Neurol Sci. 2016;371:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Kim HK, Kim CH, Kim EH, Bae SJ, Choe J, Park JY, Park SW, Yun YD, Baek SJ, Mok Y, Jee SH. Impaired fasting glucose and risk of cardiovascular disease in Korean men and women: the Korean Heart Study. Diabetes Care. 2013;36:328-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Oizumi T, Daimon M, Jimbu Y, Wada K, Kameda W, Susa S, Yamaguchi H, Ohnuma H, Tominaga M, Kato T. Impaired glucose tolerance is a risk factor for stroke in a Japanese sample--the Funagata study. Metabolism. 2008;57:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Sung J, Song YM, Ebrahim S, Lawlor DA. Fasting blood glucose and the risk of stroke and myocardial infarction. Circulation. 2009;119:812-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Kamouchi M, Matsuki T, Hata J, Kuwashiro T, Ago T, Sambongi Y, Fukushima Y, Sugimori H, Kitazono T; FSR Investigators. Prestroke glycemic control is associated with the functional outcome in acute ischemic stroke: the Fukuoka Stroke Registry. Stroke. 2011;42:2788-2794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 121] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 9. | Ago T, Matsuo R, Hata J, Wakisaka Y, Kuroda J, Kitazono T, Kamouchi M; Fukuoka Stroke Registry Investigators. Insulin resistance and clinical outcomes after acute ischemic stroke. Neurology. 2018;90:e1470-e1477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 94] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 10. | Forti P, Maioli F, Nativio V, Maestri L, Coveri M, Zoli M. Association of prestroke glycemic status with stroke mortality. BMJ Open Diabetes Res Care. 2020;8:e000957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Jia Q, Liu G, Zheng H, Zhao X, Wang C, Wang Y, Liu L, Wang Y; Investigators for the Survey on Abnormal Glucose Regulation in Patients With Acute Stroke Across China. Impaired glucose regulation predicted 1-year mortality of Chinese patients with ischemic stroke: data from abnormal glucose regulation in patients with acute stroke across China. Stroke. 2014;45:1498-1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Kim BG, Kim GY, Cha JK. Pre-diabetes is a predictor of short-term poor outcomes after acute ischemic stroke using IV thrombolysis. BMC Neurol. 2021;21:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Kim NH, Kwon TY, Yu S, Kim NH, Choi KM, Baik SH, Park Y, Kim SG. Increased Vascular Disease Mortality Risk in Prediabetic Korean Adults Is Mainly Attributable to Ischemic Stroke. Stroke. 2017;48:840-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Osei E, Fonville S, Zandbergen AA, Koudstaal PJ, Dippel DW, den Hertog HM. Glucose in prediabetic and diabetic range and outcome after stroke. Acta Neurol Scand. 2017;135:170-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Roquer J, Rodríguez-Campello A, Cuadrado-Godia E, Giralt-Steinhauer E, Jiménez-Conde J, Dégano IR, Ois A. Ischemic stroke in prediabetic patients. J Neurol. 2014;261:1866-1870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Wu S, Wang C, Jia Q, Liu G, Hoff K, Wang X, Wang A, Wang C, Zhao X, Wang Y, Liu L, Wang Y. HbA1c is associated with increased all-cause mortality in the first year after acute ischemic stroke. Neurol Res. 2014;36:444-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Zhu Z, Yang J, Zhong C, Xu T, Wang A, Bu X, Peng Y, Peng H, Xu T, Chen CS, Sun Y, Chen J, Zhang Y, He J; CATIS Investigation Groups. Abnormal glucose regulation, hypoglycemic treatment during hospitalization and prognosis of acute ischemic stroke. J Neurol Sci. 2017;379:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Luitse MJ, Biessels GJ, Rutten GE, Kappelle LJ. Diabetes, hyperglycaemia, and acute ischaemic stroke. Lancet Neurol. 2012;11:261-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 343] [Article Influence: 24.5] [Reference Citation Analysis (1)] |
| 19. | Abilleira S, Ribera A, Sánchez E, Roquer J, Duarte E, Tresserras R, Gallofré M. [In-hospital stroke care in Catalonia [Spain]. Results of the "First Clinical Audit of Stroke. Catalonia, 2005/2006"]. Gac Sanit. 2008;22:565-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Pan Y, Chen W, Wang Y. Prediabetes and Outcome of Ischemic Stroke or Transient Ischemic Attack: A Systematic Review and Meta-analysis. J Stroke Cerebrovasc Dis. 2019;28:683-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 21. | Yao M, Ni J, Zhou L, Peng B, Zhu Y, Cui L; SMART investigators. Elevated Fasting Blood Glucose Is Predictive of Poor Outcome in Non-Diabetic Stroke Patients: A Sub-Group Analysis of SMART. PLoS One. 2016;11:e0160674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Johnston KC, Bruno A, Pauls Q, Hall CE, Barrett KM, Barsan W, Fansler A, Van de Bruinhorst K, Janis S, Durkalski-Mauldin VL; Neurological Emergencies Treatment Trials Network and the SHINE Trial Investigators. Intensive vs Standard Treatment of Hyperglycemia and Functional Outcome in Patients With Acute Ischemic Stroke: The SHINE Randomized Clinical Trial. JAMA. 2019;322:326-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 303] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 23. | Jia W, Jia Q, Zhang Y, Zhao X, Wang Y. Effect of prediabetes on asprin or clopidogrel resistance in patients with recent ischemic stroke/TIA. Neurol Sci. 2021;42:2829-2835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/