Published online Sep 15, 2025. doi: 10.4251/wjgo.v17.i9.109060
Revised: June 7, 2025
Accepted: July 21, 2025
Published online: September 15, 2025
Processing time: 140 Days and 1.9 Hours
Hepatocellular carcinoma (HCC) remains a significant public health concern in South Korea even though the incidence rates are declining. While medical travel for cancer treatment is common, its patterns and influencing factors for patients with HCC are unknown.
To assess medical travel patterns and determinants and their policy implications among patients with newly diagnosed HCC in South Korea.
This retrospective cohort study used the National Health Insurance Service database to identify patients with newly diagnosed HCC from 2013 to 2021. Medical travel was defined as receiving initial treatment outside one’s residential region. Patient characteristics and regional trends were analyzed, and factors influencing medical travel were identified using logistic regression analysis.
Among 64808 patients 52.4% received treatment in the capital. This proportion increased to 67.4% when including the surrounding metropolitan area. Medical travel was significantly more common among younger and wealthier patients. Patients with greater comorbidity burden or liver cirrhosis were less likely to travel. While geographic distance influenced travel patterns, high-volume academic centers in the capital attracted patients nationwide regardless of proximity.
This nationwide study highlighted the centralization of HCC care in the capital. This observation indicates that regional cancer hubs should be strengthened and promoted for equitable healthcare access.
Core Tip: This nationwide retrospective cohort study examined domestic medical travel patterns among patients newly diagnosed with hepatocellular carcinoma in South Korea. Despite universal health insurance and open provider access, over half of the patients with hepatocellular carcinoma traveled to the capital for initial treatment. Younger age, higher income, and residence in non-capital regions were key drivers of medical travel. These findings highlighted the persistent regional disparities and indicate that policy efforts to strengthen regional cancer centers should be made to ensure geographically equitable access to specialized care.
- Citation: Kim S, Kim N, Lee HS, Kim M, Kim H, Choi Y. Medical travel patterns for hepatocellular carcinoma treatment in South Korea: National Health Insurance data from 2013 to 2021. World J Gastrointest Oncol 2025; 17(9): 109060
- URL: https://www.wjgnet.com/1948-5204/full/v17/i9/109060.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i9.109060
The incidence of primary liver cancer in South Korea has been declining since 1999, with an annual reduction of 1.2% from 1999 to 2010 and followed by a more pronounced decrease of 4.0%. Despite this downward trend primary liver cancer remained the seventh most common cancer and the second-leading cause of cancer-related mortality in 2021, surpassed only by lung cancer[1]. Given its high incidence and mortality rates, liver cancer represents a substantial public health burden in South Korea. Although regional disparities in incidence and treatment have been reported, few studies have thoroughly examined inter-regional access to care[2].
Hepatocellular carcinoma (HCC) accounts for approximately 90% of primary liver cancers[3,4] and is the focus of this study. Globally, HCC represents a major oncological burden, particularly in East Asia where it accounts for a high proportion of liver cancer cases[3]. Its complex etiology and diverse treatment options, ranging from resection and locoregional therapy to transplantation and systemic therapy, require multidisciplinary management and highly specialized care settings[4]. Since the implementation of mandatory social health insurance in 1989, the National Health Insurance Service (NHIS) has provided coverage to nearly the entire South Korean population[5]. This system allows patients to freely select healthcare providers regardless of geographic location. Consequently, many cancer patients seek treatment outside their residential areas, particularly in Seoul[6-8]. During travel for medical purposes, patients typically pay additional costs for transportation and lodging, endure additional physical and mental fatigue, and must allow extra time. The expenses for medical travel are challenging for patients as well as the national health care system[9,10].
Currently, no large-scale studies have examined the trends of medical travel among South Korean patients with HCC. Although a prior investigation analyzing patients with prostate cancer revealed a mobility pattern concentrated in the capital region[8], HCC care is generally more complex and requires chronic disease management and multiple treatment phases. Therefore, evaluating travel patterns in this population may offer meaningful insights into access disparities and system-level inefficiencies. The aim of this study was to evaluate the extent of medical travel among patients with HCC across different regions from 2013 to 2021. We identified demographic and regional factors influencing medical travel behavior and assessed implications for healthcare policy in South Korea. Our observations can potentially inform other countries with centralized cancer care systems of their citizens’ medical travel patterns.
Koreans are universally enrolled in the NHIS, a government-operated single-payer program. The Korean National Health Information Database combines information obtained from the NHIS collected for claims and reimbursement of health care services and general health examination results[11,12]. Accordingly, health care information on HCC was retrieved from the National Health Information Database.
This retrospective cohort included patients newly diagnosed with HCC between 2013 and 2021. They were identified by the International Classification of Diseases, 10th Revision (ICD-10) code C22.0. Initial treatment was defined as the first recorded procedure code for HCC-related therapy, including hepatic resection (Q7221, Q7222, Q7223), liver trans
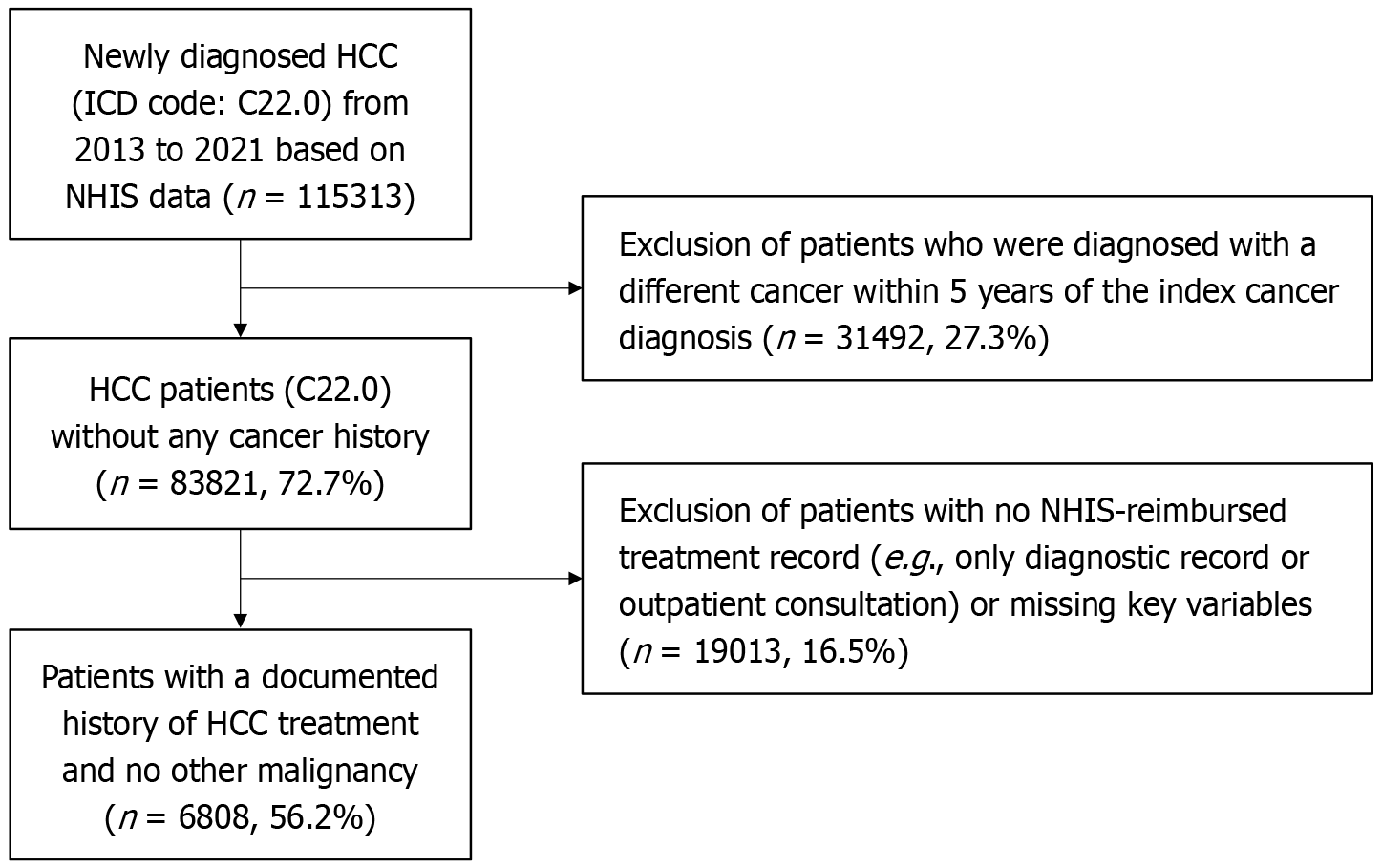
Individuals with a prior diagnosis of any malignancy within the preceding 5 years were excluded to minimize confounding. To ensure accurate assessment of medical travel, patients without records of initial treatment were excluded. Patients who had only a single outpatient consultation without any procedural or therapeutic claims were assumed to have declined treatment and were therefore excluded. Cases with incomplete eligibility or missing core sociodemographic data were excluded. Figure 1 outlines the cohort selection process.
HCC management typically involves multiple treatment modalities and requires regular follow-up to evaluate treatment response and plan subsequent care. Because of this complexity, patients often prefer continuity of care at a single institution. The treatment region was determined by the administrative location of the facility where the initial treatment was provided. Medical travel was defined as receiving this initial treatment in a region other than the patient’s region of residence.
South Korea is administratively divided into 17 regions. Chungcheong Province was consolidated to include both the southern and northern provinces as well as Sejong City to improve regional homogeneity. Similarly, the South and North Provinces of Jeolla and of Gyeongsang were merged into single regions. Therefore, the study population was categorized into 13 consolidated regions. The residential region and the region of the initial treatment facility were compared to identify interregional medical travel. Additionally, regional patterns of patient inflow and outflow were quantified.
Factors influencing medical travel consisted of age, sex, Charlson comorbidity index (CCI), year of diagnosis, income level, residential region, liver cirrhosis, and extrahepatic metastasis. The NHIS premium is principally based on household income, and the medical aid group (Medicare), which accounts for approximately 3% of the population, is exempt from this premium[12]. Income level was derived from NHIS premium data, which ranges from 0 to 20. Medicare beneficiaries correspond to level 0, while the remaining values were grouped into four income quintiles as follows: 1-5 (low income); 6-10 (low-middle income); 11-15 (middle-high income); and 16-20 (high income). CCI, a standardized measure of comorbidity severity designed to predict patient outcomes following critical illness, was calculated based on ICD-10 codes in the year prior to diagnosis (including liver cancer), resulting in no patients with a score of 0. Scores were categorized as 2, 3-4, and ≥ 5. Patients with missing values in key covariates such as income, region, or treatment status were excluded from the final cohort.
The trend of medical travel was deduced from the number of patients diagnosed and treated in a region. Net migration was calculated from the difference between the number of treated and diagnosed patients in each region and was analyzed using a t-test. The Cochran-Armitage trend test was employed to compare differences in trends in medical travel by year. Characteristics of patients treated either in or outside residential regions were analyzed using a t-test for continuous variables and the χ2 test for categorical variables. A multivariable logistic regression model was used to calculate adjusted odds ratios (aORs) and 95% confidence intervals for receiving initial treatment at an out-of-region hospital. Variables with P < 0.05 in univariate analysis were included in the multivariate model. All analyses were performed using SAS statistical software, version 9.4 (SAS Institute Inc., Cary, NC, United States). Statistical significance was set at P < 0.05.
From 2013 to 2021, a total of 64808 patients were newly diagnosed and treated for HCC in South Korea. Table 1 presents the demographic and clinical characteristics stratified by treatment in the patients’ residential region or another region. The mean age of patients with HCC was 61.3 years, with 50988 (78.6%) males and 13820 (21.3%) females. The largest patient cohort comprised the 50-59 years age group, followed by the 60-69 years and 70-79 years age groups. Patients receiving treatment outside their residential region had a significantly lower mean age (60.3 years vs 62.4 years, P < 0.0001).
| Characteristics | Different region | Residential region | P value | ||
| n/N | % | n/N | % | ||
| Age in years | |||||
| 0-39 | 1258/1938 | 64.9 | 680/1938 | 35.1 | < 0.0001a |
| 40-49 | 5033/8745 | 57.6 | 3712/8745 | 42.4 | |
| 50-59 | 11491/21062 | 54.6 | 9571/21062 | 45.4 | |
| 60-69 | 9759/18575 | 52.5 | 8816/18575 | 47.5 | |
| 70-79 | 5563/11775 | 47.2 | 6212/11775 | 52.8 | |
| ≥ 80 | 1053/2713 | 38.8 | 1660/2713 | 61.2 | |
| Sex | |||||
| Male | 26852/50988 | 52.7 | 24136/50988 | 47.3 | 0.6841 |
| Female | 7305/13820 | 52.9 | 6515/13820 | 47.1 | |
| Residential region | |||||
| Seoul | 401/9879 | 4.1 | 9478/9879 | 95.9 | < 0.0001b |
| Busan | 1923/4777 | 40.3 | 2854/4777 | 59.7 | |
| Daegu | 758/2780 | 27.3 | 2022/2780 | 72.7 | |
| Incheon | 1392/3185 | 43.7 | 1793/3185 | 56.3 | |
| Gwangju | 915/1194 | 76.6 | 279/1194 | 23.4 | |
| Daejeon | 529/1212 | 43.6 | 683/1212 | 56.4 | |
| Ulsan | 509/999 | 51.0 | 490/999 | 49.0 | |
| Chungcheong | 4159/5122 | 81.2 | 963/5122 | 18.8 | |
| Gyeonggi | 8909/15978 | 55.8 | 7069/15978 | 44.2 | |
| Gangwon | 1552/2299 | 67.5 | 747/2299 | 32.5 | |
| Jeolla | 4097/6194 | 66.1 | 2097/6194 | 33.9 | |
| Gyeongsang | 8279/10042 | 82.4 | 1763/10042 | 17.6 | |
| Jeju | 726/1147 | 63.3 | 421/1147 | 36.7 | |
| Year of diagnosis | |||||
| 2013 | 4008/7552 | 53.1 | 3544/7552 | 46.9 | 0.0045b |
| 2014 | 3986/7382 | 54.0 | 3396/7382 | 46.0 | |
| 2015 | 4047/7501 | 54.0 | 3454/7501 | 46.0 | |
| 2016 | 3933/7436 | 52.9 | 3503/7436 | 47.1 | |
| 2017 | 3894/7404 | 52.6 | 3510/7404 | 47.4 | |
| 2018 | 3817/7204 | 53.0 | 3387/7204 | 47.0 | |
| 2019 | 3775/7294 | 51.8 | 3519/7294 | 48.2 | |
| 2020 | 3530/6872 | 51.4 | 3342/6872 | 48.6 | |
| 2021 | 3167/6163 | 51.4 | 2996/6163 | 48.6 | |
| CCI | |||||
| 2 | 4063/7285 | 55.8 | 3222/7285 | 44.2 | < 0.0001b |
| 3-4 | 14207/26245 | 54.1 | 12038/26245 | 45.9 | |
| ≥ 5 | 15887/31278 | 50.8 | 15391/31278 | 49.2 | |
| Income level, quintiles | |||||
| Medicare | 1450/3847 | 37.7 | 2397/3847 | 62.3 | < 0.0001b |
| 1 (low income) | 5716/11297 | 50.6 | 5581/11297 | 49.4 | |
| 2 | 4747/9474 | 50.1 | 4727/9474 | 49.9 | |
| 3 | 5885/11406 | 51.6 | 5521/11406 | 48.4 | |
| 4 | 7155/13047 | 54.8 | 5892/13047 | 45.2 | |
| 5 (high income) | 9204/15737 | 58.5 | 6533/15737 | 41.5 | |
| Liver cirrhosis | |||||
| Yes | 5611/11054 | 50.8 | 5443/11054 | 49.2 | < 0.0001b |
| No | 28546/53754 | 53.1 | 25208/53754 | 46.9 | |
| Extrahepatic metastasis | |||||
| Yes | 3912/7458 | 52.5 | 3546/7458 | 47.5 | 0.6442 |
| No | 30245/57350 | 52.7 | 27105/57350 | 47.3 | |
Seoul exhibited the highest in-region treatment rate at 95.9%, followed by Daegu and Busan. Patients receiving medical aid were the only socioeconomic group more likely to be treated in their residential region. Higher CCI scores were more prevalent among patients treated in their residential region. Treatment region was significantly associated with age, residential area, CCI, income level, and liver cirrhosis status (all P < 0.0001) and with the year of diagnosis (P = 0.0045).
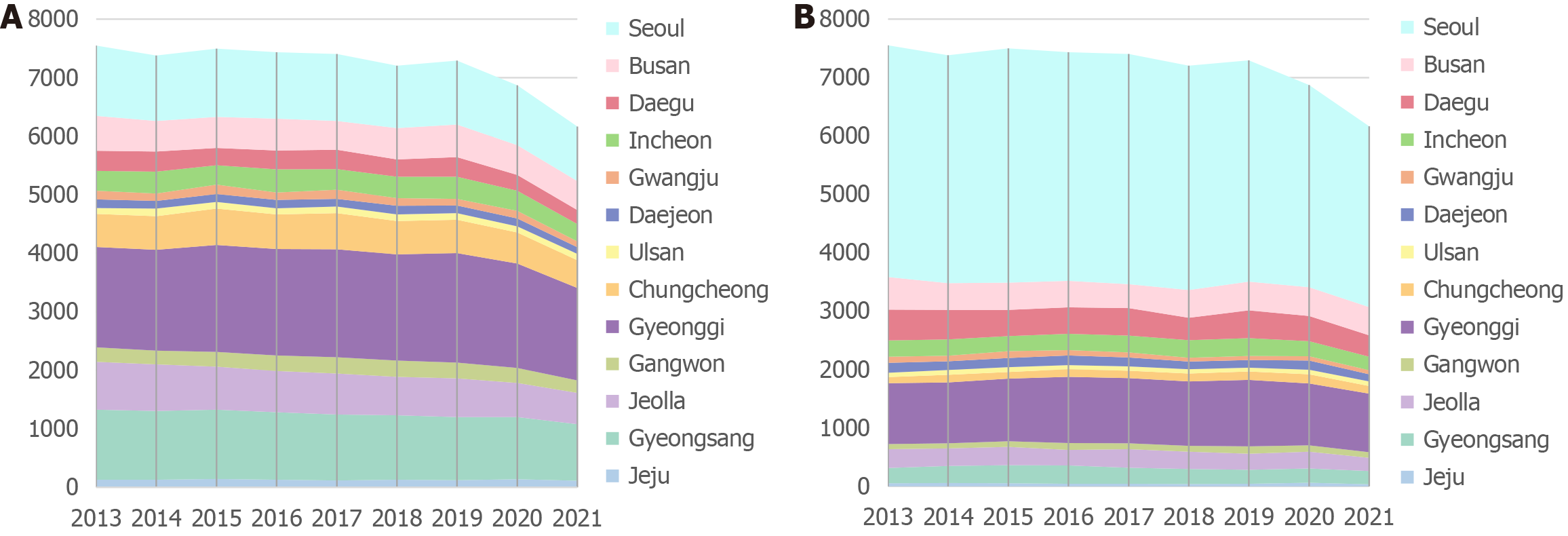
Gyeonggi Province had the largest number of newly diagnosed patients, followed by the Gyeongsang Province and Seoul. This trend was consistent throughout the study period (Figure 2). When analyzing patients outside of Seoul and the Gyeonggi Province (which surrounds Seoul on three sides, to the north, east, and south), more than half of these patients traveled to Seoul for initial treatment. This proportion increased to 67.4% when including the Gyeonggi Province. This observation highlighted the significant concentration of treatment in the capital region. Among patients who received treatment outside their residential region, 71.6% selected Seoul as their treatment destination. When expanded to include the Gyeonggi Province, 79.4% of patients received treatment in Seoul, indicating a strong preference for this region. The Cochran-Armitage trend test indicated a statistically significant upward trend in medical travel over time (Z = 2.006, P = 0.0448).
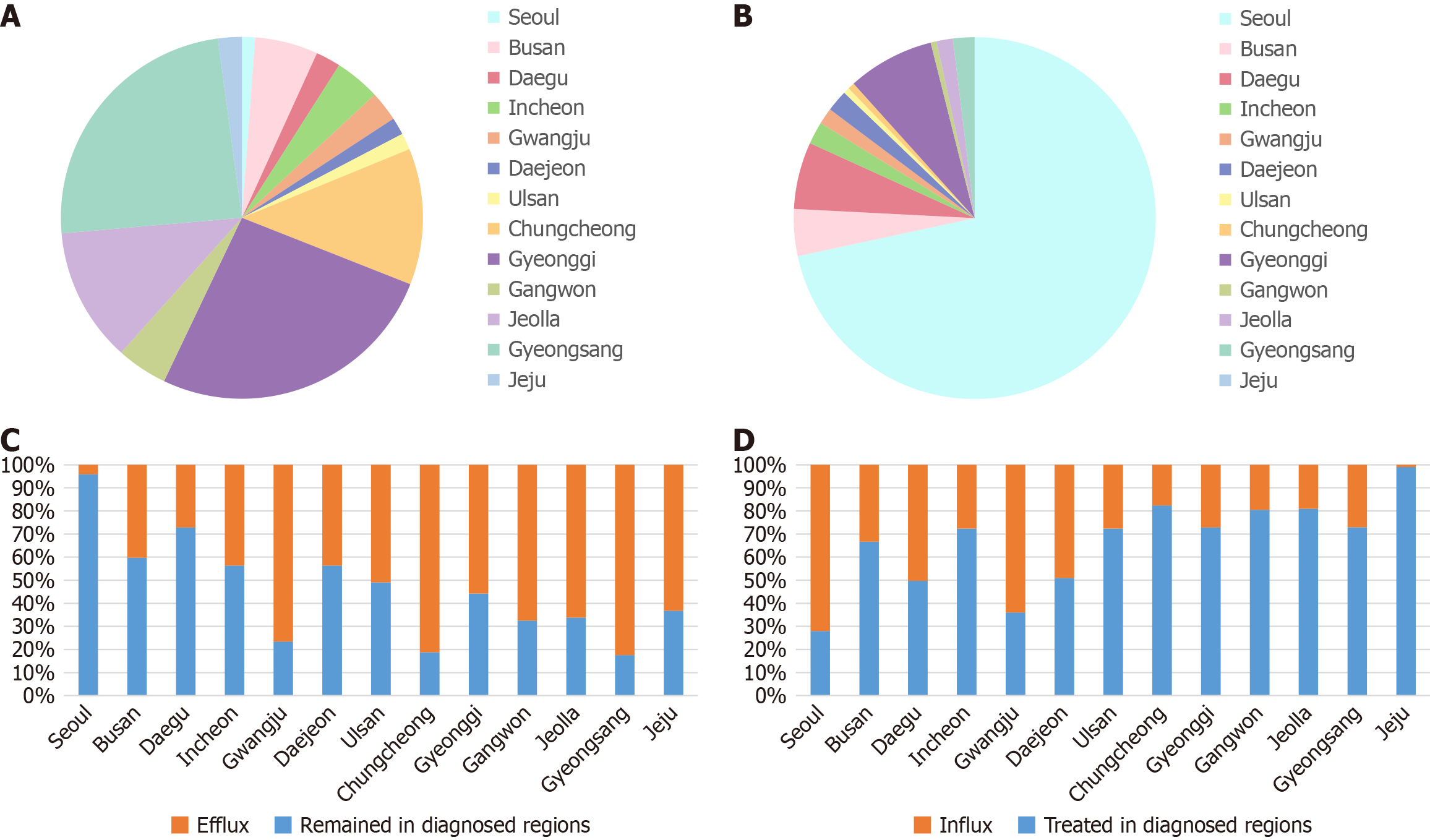
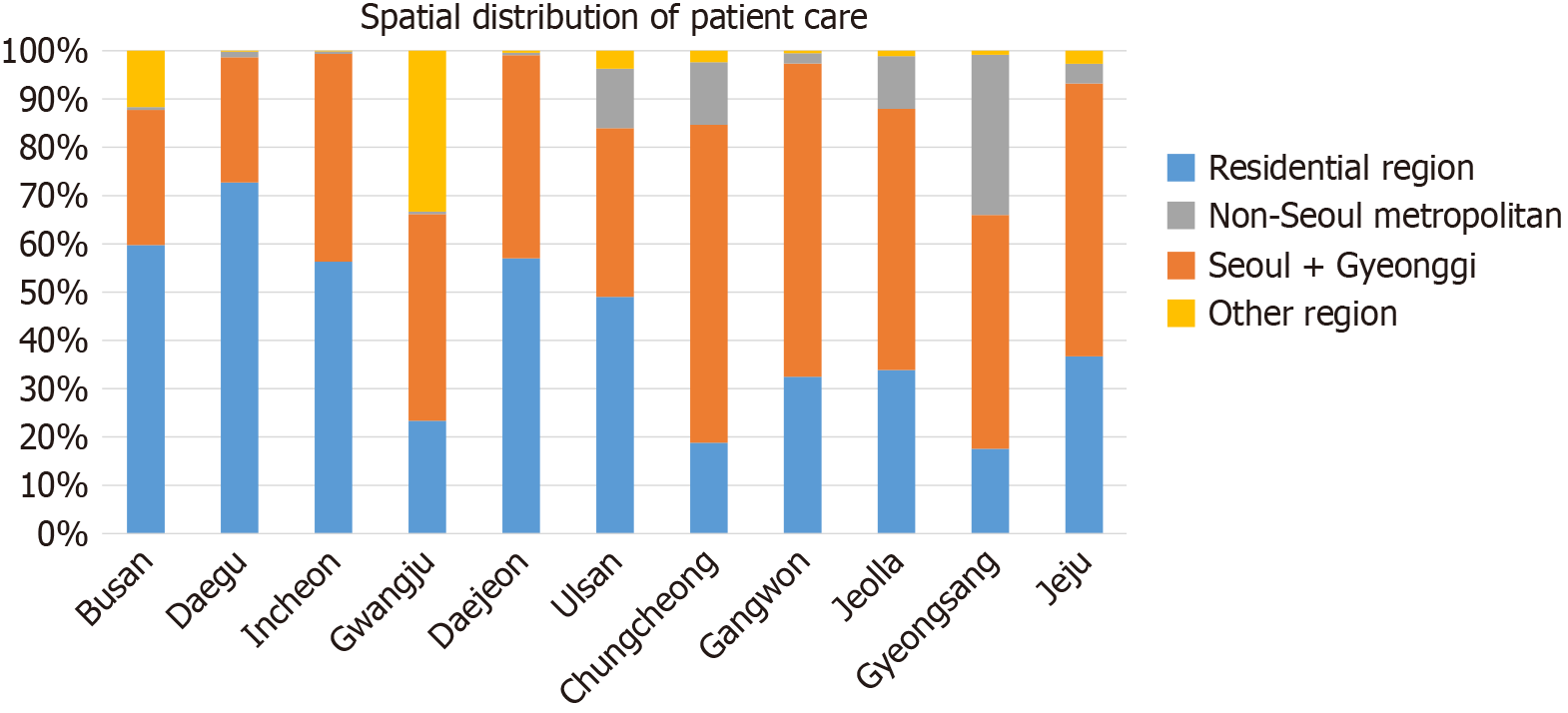
Patients from the Gyeonggi, Gyeongsang, Chungcheong, and Jeolla Provinces were the most likely to leave their residential regions for medical treatment. Seoul showed the highest treatment inflow, receiving 24451 patients from other regions, accounting for 72.1% of all patients treated in the capital. Other regions with notable patient inflows included Gyeonggi, Daegu, and Busan. When we excluded Seoul from the analysis of patient inflow, Gwangju, Daegu, Daejeon, and Busan exhibited the highest proportions of out-of-region patients. A graphical representation of medical travel is shown in Figure 3. Figure 4 presents the treatment destinations of patients by their region of residence. Although the majority of medical travel was concentrated in Seoul, Gyeongsang Province had the highest proportion of patients who sought treatment outside of Seoul. Gwangju and Chungcheong Provinces also had high proportions of patients who traveled to regions other than Seoul for treatment.
This study examined factors influencing the likelihood of receiving initial treatment for HCC at a facility outside a patient’s residential region (Table 2). Multivariate logistic regression analysis revealed that the aOR of medical travel decreased with increasing age. It was significantly more likely that the 40-49 years and 50-59 years age groups traveled outside their residential region compared with the older cohorts. Compared with patients residing in Seoul (reference group), patients in all other regions had significantly higher aORs for receiving treatment outside their residential area. The highest aORs were observed in Gyeongsang Province, Chungcheong Province, and Gwangju. Higher income levels were associated with an increased likelihood of medical travel, whereas patients with liver cirrhosis or higher CCI were significantly less likely to travel for treatment.
| Factors | aOR | 95%CI | |
| Low | High | ||
| Age in years | |||
| 00-39 | Reference | ||
| 40-49 | 0.733 | 0.661 | 0.812 |
| 50-59 | 0.649 | 0.589 | 0.715 |
| 60-69 | 0.598 | 0.542 | 0.659 |
| 70-79 | 0.484 | 0.438 | 0.535 |
| ≥ 80 | 0.343 | 0.304 | 0.387 |
| Sex | |||
| Male | Reference | ||
| Female | 1.008 | 0.971 | 1.047 |
| Residential regions | |||
| Seoul | Reference | ||
| Busan | 15.926 | 14.189 | 17.875 |
| Daegu | 8.861 | 7.779 | 10.093 |
| Incheon | 18.344 | 16.236 | 20.725 |
| Gwangju | 77.516 | 65.581 | 91.622 |
| Daejeon | 18.307 | 15.737 | 21.295 |
| Ulsan | 24.560 | 20.935 | 28.812 |
| Chungcheong | 102.079 | 90.350 | 115.330 |
| Gyeonggi | 29.790 | 26.829 | 33.078 |
| Gangwon | 49.107 | 43.005 | 56.074 |
| Jeolla | 46.179 | 41.247 | 51.700 |
| Gyeongsang | 110.994 | 99.196 | 124.194 |
| Jeju | 40.759 | 34.865 | 47.650 |
| Year of diagnosis | |||
| 2013 | Reference | ||
| 2014 | 1.038 | 0.973 | 1.107 |
| 2015 | 1.036 | 0.972 | 1.105 |
| 2016 | 0.993 | 0.931 | 1.059 |
| 2017 | 0.981 | 0.920 | 1.046 |
| 2018 | 0.996 | 0.934 | 1.063 |
| 2019 | 0.949 | 0.889 | 1.012 |
| 2020 | 0.934 | 0.875 | 0.997 |
| 2021 | 0.935 | 0.874 | 1.000 |
| CCI | |||
| 1-2 | Reference | ||
| 3-4 | 0.936 | 0.888 | 0.986 |
| ≥ 5 | 0.819 | 0.778 | 0.862 |
| Income level, quintiles | |||
| Medicare | Reference | ||
| 1 (low income) | 1.693 | 1.571 | 1.825 |
| 2 | 1.66 | 1.537 | 1.793 |
| 3 | 1.762 | 1.635 | 1.899 |
| 4 | 2.007 | 1.864 | 2.161 |
| 5 (high income) | 2.329 | 2.166 | 2.504 |
| Liver cirrhosis | |||
| Yes | Reference | ||
| No | 1.099 | 1.055 | 1.145 |
| Extrahepatic metastasis | |||
| Yes | Reference | ||
| No | 1.011 | 0.964 | 1.062 |
HCC remains the second-leading cause of cancer-related deaths in South Korea[1]. It is the primary cause of death among people in their 40s and 50s, highlighting the significant public health implications of this disease[13]. Although the clinical outcomes of HCC treatment have been studied extensively, there is a paucity of research on the determinants and implications of patients’ choices for treatment location. These types of investigations have been conducted for other cancer types[7,14], but this study represented the first focused analysis of domestic medical travel among patients with HCC in South Korea.
The most striking finding was the pronounced concentration of patients traveling to Seoul for medical treatment. A substantial 52.4% of patients with HCC sought treatment in Seoul, and this figure increased to 67.4% when considering the entire Seoul metropolitan area (which included the surrounding Gyeonggi Province). This geographic pattern remained relatively consistent from 2013 to 2021. Of note, however, the Cochran-Armitage trend test revealed a significant upward trend in medical travel over the years, indicating that the centralization of care in Seoul has become even more pronounced over time. A similar trend has been observed for other cancer types. One study analyzing the locations for diagnosis and treatment of patients with prostate cancer in South Korea revealed that 31% of patients were diagnosed in Seoul and 55% of patients received treatment there[14]. This disparity could be attributed to the number of hospitals and the population size of Seoul. Although only 15% of patients with HCC were initially diagnosed in Seoul, there are factors beyond hospital accessibility and population density that are influencing this geographic concentration of treatment.
A multitude of factors influence a patient’s choice of healthcare facility. Logistic regression analysis revealed that age, residential area, year of diagnosis, comorbidity burden, socioeconomic status, and liver cirrhosis significantly influenced the decision to seek treatment at a hospital in a different region. Other studies[9,15,16] have also found associations between younger age, higher socioeconomic status, fewer comorbidities, and higher education levels with a greater likelihood of traveling farther for medical care. The clinical complexity and relatively early age of onset of HCC[13] make access to specialized, continuous care even more critical[4].
Previous studies have consistently highlighted distance as a significant factor influencing medical travel[9,10,15]. For radiotherapy, which requires daily hospital visits, patients are less likely to choose distant facilities[10]. However, domestic medical travel in South Korea exhibited distinct patterns compared with other countries. A study on patients with prostate cancer in South Korea reported that distance was not a significant factor impacting medical travel to Seoul. In fact, the highest proportion of patients traveling to Seoul for surgery originated from Jeju Island, which is the most distant province from the capital[8]. Our study found that the highest aOR for medical travel was observed among patients residing in Gyeongsang Province, a region relatively far from Seoul.
These findings suggest that the Korean transportation infrastructure, which includes high-speed rail and domestic air travel, may mitigate geographic barriers and support greater patient mobility[17]. In addition, the tendency to seek treatment in Seoul reflects the perceptions of more medical expertise, access to advanced technology, and better treatment outcomes that are associated with high-volume academic hospitals[18]. The socialized health insurance policies in South Korea allow full coverage for patients regardless of their residential region and treatment region. This has likely reduced financial deterrents and facilitated medical centralization.
The concentration of patients seeking medical treatment in Seoul is also closely associated with structural and institutional dynamics of the healthcare system. It reflects systemic imbalances in healthcare infrastructure and workforce distribution. The majority of nationally designated cancer centers and liver disease specialists are located in Seoul[18]. Recent research highlighted that regional disparities in the availability of cancer clinical trials persist in South Korea with a vast majority being concentrated in the Seoul metropolitan area. This disparity limits access to innovative treatments for patients in regions outside the capital and reinforces the structural centralization of cancer care delivery[19]. Because HCC therapies rapidly evolve (e.g., the recent adoption of atezolizumab plus bevacizumab as a first-line systemic treat
The volume-outcome relationship suggests that high-volume centers have better outcomes, supporting centralization[20,21]. However, benefits may plateau or reverse beyond a certain threshold[22]. Nallamothu et al[23] found that high-volume hospitals generally had better outcomes for percutaneous coronary interventions. However, this advantage diminished after a certain volume threshold. Other studies argue that hospital resources, surgeon expertise, and care coordination are equally or more important than volume alone[24,25]. High-volume hospitals may face overcrowding, long wait times, and provider burnout, compromising the quality of care[26]. Moreover, centralization may weaken the role and viability of local hospitals, particularly in rural or underserved regions, exacerbating disparities and marginalizing healthcare access[18].
Our analysis of travel for medical treatment revealed an interesting pattern. While there was a significant outflow of patients from major metropolitan cities such as Busan and Daegu to Seoul, there was also a substantial inflow into these cities from surrounding regions. Gwangju exhibited the highest proportion of patients from other regions (64.0%), followed by Daegu (50.3%), Daejeon (49.1%), and Busan (33.4%). The primary inflow for Gwangju was from the Jeolla Province, while Daegu and Busan received most of their patients from the Gyeongsang Province and Daejeon from the Chungcheong Province. Regional hubs may serve as secondary centers of excellence and alleviate patient pressure on Seoul-based hospitals[7]. Policy initiatives including establishing regional liver cancer centers, implementing telemedicine-based tumor boards, and providing travel subsidies for underserved patients could serve as effective decentralization strategies[16].
This study has implications beyond South Korea. Other countries with centralized healthcare systems face similar challenges in balancing efficiency and equity[27-29]. Our Korean experience highlighted the need for proactive policy interventions that enhance regional capacity and promote spatial equity in healthcare delivery. Countries with universal health coverage may experience comparable trends of patients concentrating their medical care in capital or metropolitan areas[30]. The trade-offs between the pursuit of quality through centralization and the need to ensure geographically equitable access must be navigated by countries experiencing this trend[31]. Even with universal coverage and advanced transportation networks, regional disparities in access and care quality may persist, underscoring the need for targeted policy support[32]. The phenomenon of patients traveling for medical treatment remains prevalent and is influenced by a complex interplay of demographic, structural, and institutional factors. Policymakers must weigh the benefits of high-volume care against the potential to exacerbate regional disparities[22]. Further research should be carried out to develop a more sophisticated approach to guarantee high-quality care in all healthcare environments.
Several limitations of this study should be acknowledged. First, the health insurance data used in this study did not include detailed information such as patient stage or Child-Pugh score. This limited our ability to assess the impact of patient condition and severity on medical travel. Although liver cirrhosis was included as a covariate in the logistic regression analysis, it may not fully capture the heterogeneity in patient severity. With more granular data on patient conditions, further analysis on medical travel would have been possible. Second, the CCI was calculated using ICD-10 codes that included liver cancer, resulting in a minimum score of 2 for all patients. This approach will affect comparability with other studies that assess comorbidity independently of the index cancer. Third, this study used claims data limited to reimbursed care. This method excludes privately paid treatments or procedures performed outside the NHIS framework. Fourth, the dataset did not distinguish between a curative intent and a palliative intent of treatment. We hypothesize that this parameter would influence the choice of treatment location. Fifth, the lack of address-level data restricted our ability to assess precise spatial patterns, including urban–rural disparities. Sixth, model diagnostics such as the area under the curve or the Hosmer-Lemeshow test could not be performed due to analysis constraints. While some regional variables showed high aORs, we believe this reflects the strong centralization of care in Seoul rather than model overfitting.
This nationwide retrospective cohort study revealed a striking centralization of HCC treatment in the capital, Seoul where over half of all patients received care regardless of where they were diagnosed. Medical travel was more common among younger, wealthier patients, reflecting persistent regional disparities in healthcare access. To address this disparity, policymakers should implement decentralization strategies including strengthening regional cancer centers, redistributing healthcare resources, and improving care coordination across regions. Our observations offer valuable insights for South Korea as well as other countries with centralized healthcare systems where similar equity-efficiency tradeoffs may arise. Ensuring regionally balanced access to high-quality cancer care remains essential for sustainable and equitable health system performance.
| 1. | Kang MJ, Jung KW, Bang SH, Choi SH, Park EH, Yun EH, Kim HJ, Kong HJ, Im JS, Seo HG; Community of Population-Based Regional Cancer Registries*. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2020. Cancer Res Treat. 2023;55:385-399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 149] [Reference Citation Analysis (0)] |
| 2. | Park EH, Kang MJ, Jung KW, Park EH, Yun EH, Kim HJ, Kong HJ, Choi CK, Im JS, Seo HG. Regional disparities in major cancer incidence in Korea, 1999-2018. Epidemiol Health. 2023;45:e2023089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Oh JH, Jun DW. The latest global burden of liver cancer: A past and present threat. Clin Mol Hepatol. 2023;29:355-357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 85] [Reference Citation Analysis (0)] |
| 4. | Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, Lencioni R, Koike K, Zucman-Rossi J, Finn RS. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7:6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4432] [Cited by in RCA: 4462] [Article Influence: 892.4] [Reference Citation Analysis (4)] |
| 5. | Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009;24:63-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 309] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 6. | Park S, Park IK, Kim ER, Hwang Y, Lee HJ, Kang CH, Kim YT. Current Trends of Lung Cancer Surgery and Demographic and Social Factors Related to Changes in the Trends of Lung Cancer Surgery: An Analysis of the National Database from 2010 to 2014. Cancer Res Treat. 2017;49:330-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Jeong JH, Jung J, Kim HJ, Lee JW, Ko BS, Son BH, Jung KH, Chung IY. Domestic medical travel from non-Seoul regions to Seoul for initial breast cancer treatment: a nationwide cohort study. Ann Surg Treat Res. 2023;104:71-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 8. | Kim JH, Kim SY, Yun SJ, Chung JI, Choi H, Yu HS, Ha YS, Cho IC, Kim HJ, Chung HC, Koh JS, Kim WJ, Park JH, Lee JY. Medical Travel among Non-Seoul Residents to Seek Prostate Cancer Treatment in Medical Facilities of Seoul. Cancer Res Treat. 2019;51:53-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Lin CC, Bruinooge SS, Kirkwood MK, Hershman DL, Jemal A, Guadagnolo BA, Yu JB, Hopkins S, Goldstein M, Bajorin D, Giordano SH, Kosty M, Arnone A, Hanley A, Stevens S, Olsen C. Association Between Geographic Access to Cancer Care and Receipt of Radiation Therapy for Rectal Cancer. Int J Radiat Oncol Biol Phys. 2016;94:719-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 10. | Muralidhar V, Rose BS, Chen YW, Nezolosky MD, Nguyen PL. Association Between Travel Distance and Choice of Treatment for Prostate Cancer: Does Geography Reduce Patient Choice? Int J Radiat Oncol Biol Phys. 2016;96:313-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 11. | Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, Do CH, Song JS, Hyon Bang J, Ha S, Lee EJ, Ae Shin S. Data Resource Profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017;46:799-800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 660] [Article Influence: 82.5] [Reference Citation Analysis (0)] |
| 12. | Kim MK, Han K, Lee SH. Current Trends of Big Data Research Using the Korean National Health Information Database. Diabetes Metab J. 2022;46:552-563. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 114] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 13. | Gong YH, Yoon SJ, Jo MW, Kim A, Kim YA, Yoon J, Seo H, Kim D. The Burden of Cancer in Korea during 2012: Findings from a Prevalence-Based Approach. J Korean Med Sci. 2016;31 Suppl 2:S168-S177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Kim SC, Han S, Yoon JH, Park S, Moon KH, Cheon SH, Park GM, Kwon T. Analysis of trend in the role of national and regional hubs in prostatectomy after prostate cancer diagnosis in the past 5 years: A nationwide population-based study. Investig Clin Urol. 2024;65:124-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Lamont EB, Hayreh D, Pickett KE, Dignam JJ, List MA, Stenson KM, Haraf DJ, Brockstein BE, Sellergren SA, Vokes EE. Is patient travel distance associated with survival on phase II clinical trials in oncology? J Natl Cancer Inst. 2003;95:1370-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 123] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 16. | Kim D, Kang GW, Jang H, Cho JY, Yang B, Yang HC, Hwang J. Trend of lung cancer surgery, hospital selection, and survival between 2005 and 2016 in South Korea. Thorac Cancer. 2022;13:210-218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Hong NS, Lee KS, Kam S, Choi GS, Kwon OK, Ryu DH, Kim SW. A Survival Analysis of Gastric or Colorectal Cancer Patients Treated With Surgery: Comparison of Capital and a Non-capital City. J Prev Med Public Health. 2017;50:283-293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Kim W, Han KT, Kim S. Do Patients Residing in Provincial Areas Transport and Spend More on Cancer Treatment in Korea? Int J Environ Res Public Health. 2021;18:9247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Jang J, Choi W, Sim SH, Kang S. Regional disparities in the availability of cancer clinical trials in Korea. Epidemiol Health. 2024;46:e2024006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 20. | Uhlig J, Sellers CM, Khan SA, Cha C, Kim HS. Hepatocellular carcinoma: Impact of academic setting and hospital volume on patient survival. Surg Oncol. 2019;31:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Sato Y, Kaneko R, Yano Y, Kamada K, Kishimoto Y, Ikehara T, Sato Y, Matsuda T, Igarashi Y. Volume-Outcome Relationship in Cancer Survival Rates: Analysis of a Regional Population-Based Cancer Registry in Japan. Healthcare (Basel). 2022;11:16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 22. | Koh YX, Zhao Y, Tan IE, Tan HL, Chua DW, Loh WL, Tan EK, Teo JY, Au MKH, Goh BKP. The impact of hospital volume on liver resection: A systematic review and Bayesian network meta-analysis. Surgery. 2024;175:393-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (1)] |
| 23. | Nallamothu BK, Wang Y, Magid DJ, McNamara RL, Herrin J, Bradley EH, Bates ER, Pollack CV Jr, Krumholz HM; National Registry of Myocardial Infarction Investigators. Relation between hospital specialization with primary percutaneous coronary intervention and clinical outcomes in ST-segment elevation myocardial infarction: National Registry of Myocardial Infarction-4 analysis. Circulation. 2006;113:222-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 24. | Holt PJ, Poloniecki JD, Gerrard D, Loftus IM, Thompson MM. Meta-analysis and systematic review of the relationship between volume and outcome in abdominal aortic aneurysm surgery. Br J Surg. 2007;94:395-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 210] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 25. | Ross JS, Normand SL, Wang Y, Ko DT, Chen J, Drye EE, Keenan PS, Lichtman JH, Bueno H, Schreiner GC, Krumholz HM. Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med. 2010;362:1110-1118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 270] [Cited by in RCA: 264] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 26. | Royal College of Physicians. NHS reality check: Delivering care under pressure. June 2018. [cited 18 March 2025]. Available from: https://www.rcp.ac.uk/improving-care/resources/nhs-reality-check-2017-delivering-care-under-pressure. |
| 27. | Organization and financing of public health services in Europe: Country reports [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2018- . [PubMed] |
| 28. | GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459-1544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4683] [Cited by in RCA: 4356] [Article Influence: 435.6] [Reference Citation Analysis (1)] |
| 29. | GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736-1788. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5338] [Cited by in RCA: 4902] [Article Influence: 612.8] [Reference Citation Analysis (1)] |
| 30. | Doty MM, Tikkanen RS, FitzGerald M, Fields K, Williams RD 2nd. Income-Related Inequality In Affordability And Access To Primary Care In Eleven High-Income Countries. Health Aff (Millwood). 2021;40:113-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 31. | Hentschker C, Mennicken R, Reifferscheid A, Wasem J, Wübker A. Volume-outcome relationship and minimum volume regulations in the German hospital sector - evidence from nationwide administrative hospital data for the years 2005-2007. Health Econ Rev. 2018;8:25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 32. | Choi DW, Kim SJ, Kim S, Kim DW, Jeong W, Han KT. Cancer care patterns in South Korea: Types of hospital where patients receive care and outcomes using national health insurance claims data. Cancer Med. 2023;12:14707-14717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/