Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8820
Peer-review started: May 17, 2021
First decision: June 25, 2021
Revised: June 28, 2021
Accepted: August 23, 2021
Article in press: August 23, 2021
Published online: October 16, 2021
Processing time: 150 Days and 19.2 Hours
Implanted intravenous infusion port (IVAP) is indicated for patients undergoing chemotherapy, total parenteral nutrition and long-term antibiotic treatment. Among their complications, the rupture and migration of the catheter of an IVAP via internal jugular vein represents a very rare but potentially severe condition.
A 43-year-old woman was identified with a spontaneous fracture and migration of catheter of an IVAP via right internal jugular vein after adjuvant chemotherapy for left breast cancer. A computed tomography showed the fractured catheter of the IVAP in the pulmonary artery. Therefore, we conducted an emergency procedure to remove the catheter fragment by a pigtail catheter combined with a gooseneck trap.
When the fractured catheter of an IVAP was detected, the special shape of the pigtail catheter in combination with the gooseneck trap successfully facilitated the removal of the dislodged catheter.
Core Tip: Implanted intravenous infusion port (IVAP) is indicated for patients undergoing chemotherapy, total parenteral nutrition and long-term antibiotic treatment. Among their complications, the rupture and migration of the catheter of a IVAP via internal jugular vein represents a very rare but potentially severe condition. We report a case of a 43-year-old woman who was identified with a spontaneous fracture and migration of catheter of an IVAP via right internal jugular vein after adjuvant chemotherapy for left breast cancer. Computed tomography showed the fractured catheter of the IVAP in the pulmonary artery. Therefore, we conducted an emergency procedure to remove the catheter fragment by a pigtail catheter combined with the gooseneck trap.
- Citation: Chen GQ, Wu Y, Zhao KF, Shi RS. Removal of "ruptured" pulmonary artery infusion port catheter by pigtail catheter combined with gooseneck trap: A case report. World J Clin Cases 2021; 9(29): 8820-8824
- URL: https://www.wjgnet.com/2307-8960/full/v9/i29/8820.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i29.8820
Implanted intravenous infusion port (IVAP) is a subcutaneous intravenous infusion device that can be retained in the body for a long time and is widely used in many countries[1]. Because tumor patients need repeated chemotherapy and long-term infusion of high concentration nutrients, the traditional method of intravenous infusion is unsuitable, and IVAP is a common catheterization method for these patients, which can provide a good access to chemotherapy, reduce the pain of multiple punctures and improve clinical work efficiency. The puncture site is mainly subclavian vein, but due to individual differences, the catheter can be easily placed too deep or too shallow when there is no monitoring by imaging equipment. Moreover, complications, such as blockage, infection, pneumothorax, hemothorax, arterial injury, thrombus, catheter rupture, spondylolisthesis, etc., may occur due to improper nursing[2-4]. Catheter rupture is one of the most serious complications after implantation, with a reported incidence rate of 1.5%-2.6%[5,6]. Although very rare, it poses a serious threat to patients' life and needs to be actively resolved. In the case of damage, the IVAP must be removed. Ectopic embolism occurs in a very small number of patients with IVAP shedding, which causes serious complications and eventually leads to medical disputes. Herein, we have described a case with broken catheter that could not be removed by conventional technique. Hence, we finally used the special shape of pigtail catheter to remove the blocked IVAP exfoliated catheter, which has not been previously reported.
The patient was a 43-year-old woman with a single, progressive, increment mass in the upper inner quadrant of the left breast. After the eighth chemotherapy, the patient's IVAP catheter was dislodged, with wheezing, coughing, chest tightness, shortness of breath and dysphasia following exercise.
Breast cancer after chemotherapy.
On October 9, 2017, the patient underwent breast-conserving surgery, sentinel lymph node biopsy and a modified radical mastectomy for left breast cancer. After the operation, IVAP was implanted into the right internal jugular vein for eight courses of chemotherapy, consisting of 5-fluorouracil, epirubicin, cyclophosphamide and docetaxel, were administered.
The patient denied any other specific personal or family history of other diseases.
The patient presented with the following vital signs: Body temperature, 36.1 °C; blood pressure, 111/75 mmHg; pulse rate, 78 beats/min; and respiratory rate, 19 breaths/min. She was conscious and cooperative during physical examination. She had clear breathing sounds in both lungs. Her heart rate was 78 bpm with a normal rhythm, and no other abnormalities were noted.
The patient did not have a laboratory examination.
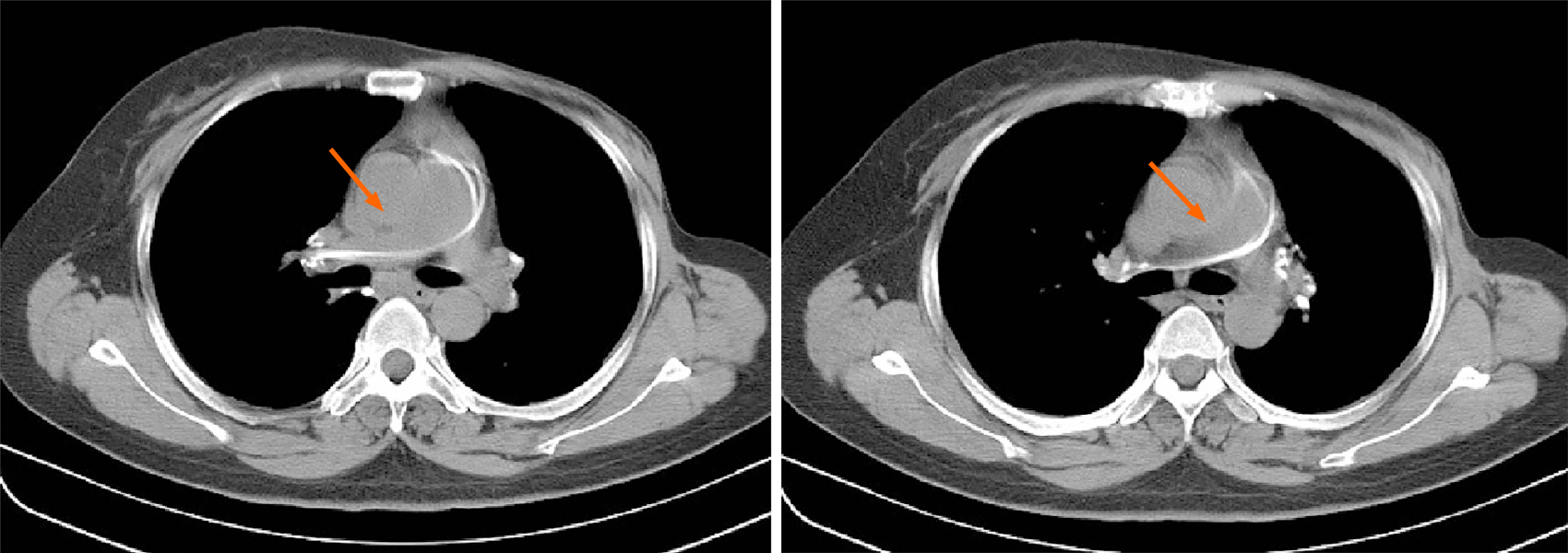
An emergency computed tomography (CT) performed on March 21, 2018 identified a strip high density shadow in the main pulmonary artery-right pulmonary artery-hilar area (Figure 1).
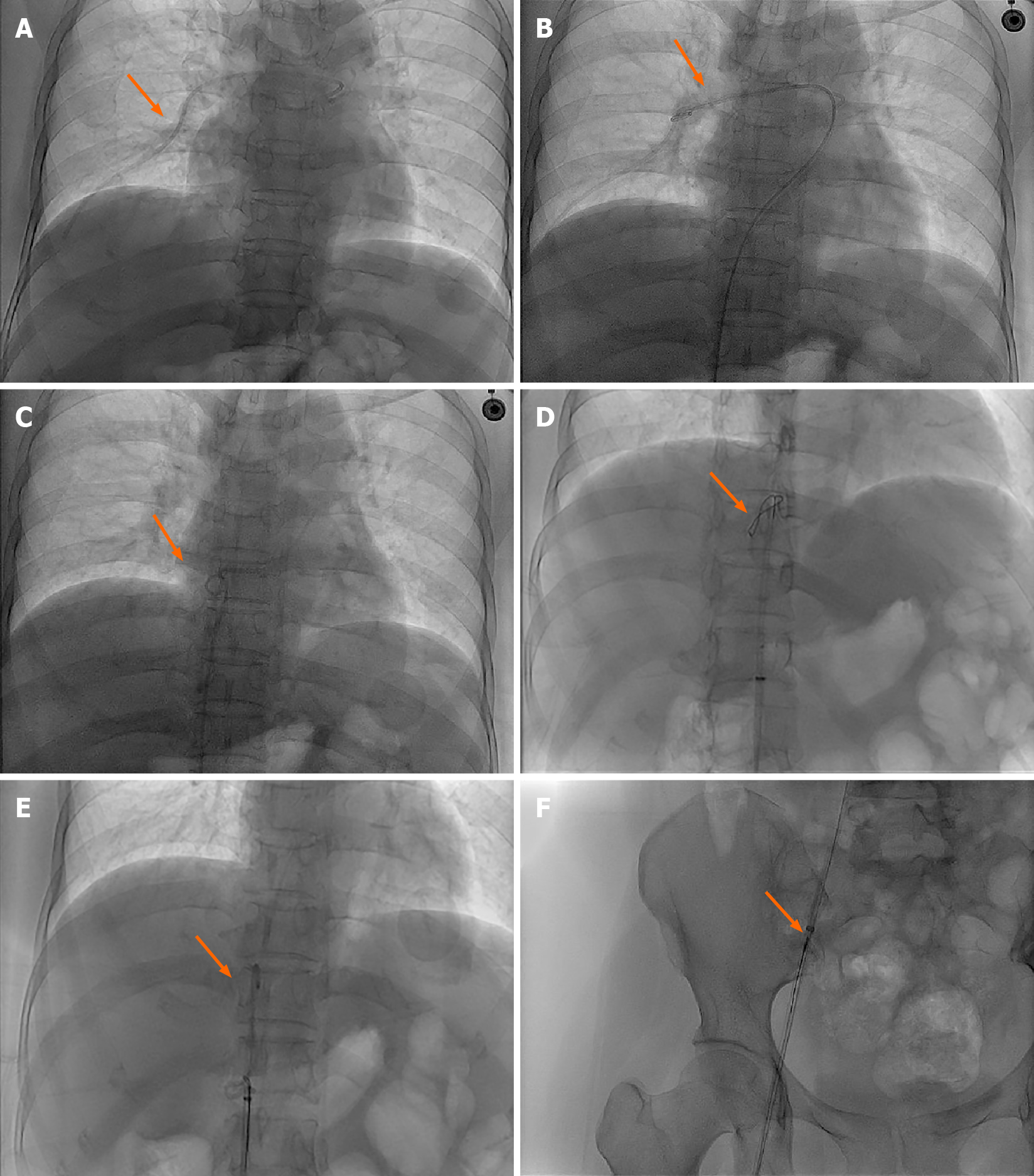
Under digital subtraction angiography fluoroscopy, the main pulmonary artery and right pulmonary artery showed tubular shadow (Figure 2A).
The final diagnosis of the presented case is exfoliated catheter.
We prepared to extract the IVAP by interventional method after consultation with relevant departments. During the operation, the patient was supine on the digital subtraction angiography examination bed. After local anesthesia of the right inguinal region, a 12F arterial sheath (model SFPQ12F) was introduced. A 5F gooseneck trap (model WXSK-20) was introduced along the arterial sheath to attempt to remove the exfoliated catheter from the main pulmonary artery and right pulmonary artery, but several attempts were unsuccessful. To analyze the location of the dislodged catheter and the effect on cardiopulmonary activity, a 5F pigtail catheter (model 45150-503H5) was selected, and the dislodged catheter was towed to the inferior vena cava after the two catheters were crossed by rotating the catheter outside the body according to the natural bending at the front end of the catheter. The IVAP catheter was then successfully removed using a 5F gooseneck trap (Figure 2B-F).
Post-operation, the patient had no chest stuffiness, and her shortness of breath symptom improved. She was discharged 2 d later.
IVAP chemotherapy can provide permanent venous access for patients and prevent the injury of peripheral blood vessels caused by irritant drugs[7]. It has the advantages of one-time puncture, convenient infusion, long-term indwelling in vivo and less pain for patients. With the increasing application of IVAP in tumor chemotherapy, the incidence of adverse events such as catheter thrombosis, obstruction and exfoliation is also increasing. Catheter rupture and shedding is one of the most serious complications. If the shedding catheter dislocates to the heart or pulmonary artery with blood flow, it will lead to arrhythmia, pericardial tamponade, pulmonary embolism, cardiac rupture, pulmonary artery rupture and other life-threatening complications[8,9]. Catheter fracture and slippage may be caused by the following: (1) Non-standard operation; (2) Inappropriate selection of the tube parts; (3) Patients have poor protection consciousness; and (4) Long-term implantation, repeated wear and oxidation of catheter. The catheter retention time should not exceed 1 year in general, and the longer the retention time, the higher the risk of complications[10]. The catheter fracture in our patient may have been due to long-term implantation, repeated wear, oxidation and folding of the catheter, as well as the poor comprehension of catheter protection, which finally led to the fracture and slippage of the catheter. The reason why it was difficult to extract the common ferrule for catheter in this case might be that the main pulmonary artery was wide, and the blood flow rate was high. In addition, cardiopulmonary activities increased the operation difficulty. The head end of the pigtail catheter is naturally bent, the surface is smooth and the stimulation to blood vessels is mild. We used the special curved shape of the head end of the pigtail catheter to cross and twist the IVAP catheter and traction the IVAP catheter to the inferior vena cava, and then used the gooseneck trap to successfully remove it through the 12F sheath.
In conclusion, conventional extraction techniques may be unable to remove the dislodged catheter. The special shape of the pigtail catheter in combination with the gooseneck trap successfully facilitated the removal of the dislodged catheter from the pulmonary artery infusion port without any complications. Hence, this is a safe and reliable method that could be clinically applied in the future.
We are thankful to the patient who agreed to participate in this study.
| 1. | Ma L, Xia C, Sun X, Zuo Y, Zhao L. The effects of oral acetylsalicylic acid on blood fluidity and infusion speed in the cancer patients with PICC. Clin Hemorheol Microcirc. 2017;65:11-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Miao J, Ji L, Lu J, Chen J. Randomized clinical trial comparing ultrasound-guided procedure with the Seldinger's technique for placement of implantable venous ports. Cell Biochem Biophys. 2014;70:559-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Ribeiro RC, Abib SC, Aguiar AS, Schettini ST. Long-term complications in totally implantable venous access devices: randomized study comparing subclavian and internal jugular vein puncture. Pediatr Blood Cancer. 2012;58:274-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Machat S, Eisenhuber E, Pfarl G, Stübler J, Koelblinger C, Zacherl J, Schima W. Complications of central venous port systems: a pictorial review. Insights Imaging. 2019;10:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 5. | Gallieni M, Pittiruti M, Biffi R. Vascular access in oncology patients. CA Cancer J Clin. 2008;58:323-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 186] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 6. | Xu L, Qin W, Zheng W, Sun X. Ultrasound-guided totally implantable venous access ports via the right innominate vein: a new approach for patients with breast cancer. World J Surg Oncol. 2019;17:196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Li G, Zhang Y, Ma H, Zheng J. Arm port vs chest port: a systematic review and meta-analysis. Cancer Manag Res. 2019;11:6099-6112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Ben Kridis W, Sahnoun M, Maraoui H, Amari N, Frikha M. Fracture at catheter of totally implantable venous access port with migration into the right pulmonary artery: A serious complication. Acta Clin Belg. 2016;71:349-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Letachowicz K, Gołębiowski T, Miś M, Wolańczyk M, Zmonarski S, Krajewska M. Partial breakage of a tunneled dialysis catheter: An uncommon finding. Hemodial Int. 2021;25:E15-E17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Busch JD, Herrmann J, Heller F, Derlin T, Koops A, Adam G, Habermann CR. Follow-up of radiologically totally implanted central venous access ports of the upper arm: long-term complications in 127,750 catheter-days. AJR Am J Roentgenol. 2012;199:447-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Deshwal H S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Guo X