Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8782
Peer-review started: June 7, 2021
First decision: June 25, 2021
Revised: July 5, 2021
Accepted: August 2, 2021
Article in press: August 2, 2021
Published online: October 16, 2021
Processing time: 130 Days and 2.2 Hours
Acute appendicitis is one of the most common acute abdominal emergencies around the world, which is always associated with infection. Infection with Salmonella typhi, an enteric pathogen, is a rare cause of acute appendicitis. We here report a patient with acute appendicitis associated with Samonella typhi infection, accompanied with spleen and kidney infarction, providing a rare example for a common surgical emergency.
A 25-year-old Pakistani man presented to the hospital with a 3-d history of fevers, vomiting, and abdominal pain. Computed tomography (CT) revealed a thickened intestinal wall of the ileocecal junction with multiple enlarged lymph nodes nearby. He was diagnosed with acute appendicitis and received laparoscopic appendectomy, which showed mild inflammation of the appendix. After the surgery, the patient presented again with a high fever (> 39 °C) and diarrhea. A CT angiography scan indicated spleen and kidney infarction. According to the blood culture, the diagnosis was finally clear to be Samonella typhi infection. The pyrexia and enteric symptoms were relieved after the application of intravenous levofloxacin.
This case, characterized by the combination of Salmonella typhi infection, acute appendicitis, and renal and splenic infraction, serves as a rare example for a common surgical emergency.
Core Tip: Acute appendicitis is one of the most common acute abdominal emergencies around the world, which is always associated with infection. Infection with Salmonella typhi, an enteric pathogen, is a rare cause of acute appendicitis. We here report a patient with acute appendicitis associated with Samonella typhi infection, accompanied by spleen and kidney infarction, providing a rare example for a common surgical emergency. This case might remind emergency doctors that the etiology of appendicitis needs to be clarified to give appropriate treatment to patients with appendicitis.
- Citation: Zheng BH, Hao WM, Lin HC, Shang GG, Liu H, Ni XJ. Samonella typhi infection-related appendicitis: A case report. World J Clin Cases 2021; 9(29): 8782-8788
- URL: https://www.wjgnet.com/2307-8960/full/v9/i29/8782.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i29.8782
Acute appendicitis is one of the most common acute abdominal emergencies around the world, with a lifetime risk of approximately 7%-8%[1]. Although infection has been considered as an important cause and trigger factor of acute appendicitis, the pathogenic mechanism and the full range of the infectious agents remain poorly understood[2,3]. As an enteric pathogen, Samonella typhi can be associated with some non-specific gastrointestinal symptoms like diarrhea, vomiting, and abdominal pain and is the main cause of typhoid fever[4]. In some rare cases, Samonella typhi infection could cause acute appendicitis[5,6]. Moreover, splenic and renal infarction is rarely reported in typhoid fever[7,8]. We here report a patient with acute appendicitis associated with Samonella typhi infection, accompanied with spleen and kidney infarction, serving as a rare example for a common surgical emergency.
A 25-year-old Pakistani man presented to the hospital with a 3-d history of subjective fevers, vomiting, and abdominal pain.
Within a month, the patient experienced several days of diarrhea. His symptoms worsened over the last 3 d and presented to the hospital with subjective fevers, vomiting, and abdominal pain.
The patient had no significant medical or surgical history, and he did not take any regular medications.
The patient did not have a history of smoking or drinking.
On presentation to the Emergency Department, the physical examination revealed a body temperature of 39.7 °C, blood pressure of 105/85 mmHg, and pulse of 108 beats per minute (slight tachycardia). Right lower abdominal pain with mild whole abdominal tenderness was found on abdominal palpation. No rashes were found.
Initial laboratory tests showed a normal white blood cell (WBC) level at 7.45 × 109/L with neutrophils at 6.5 × 109/L, zero eosinophils, and increased procalcitonin, alkaline phosphatase, and C-recreative protein.
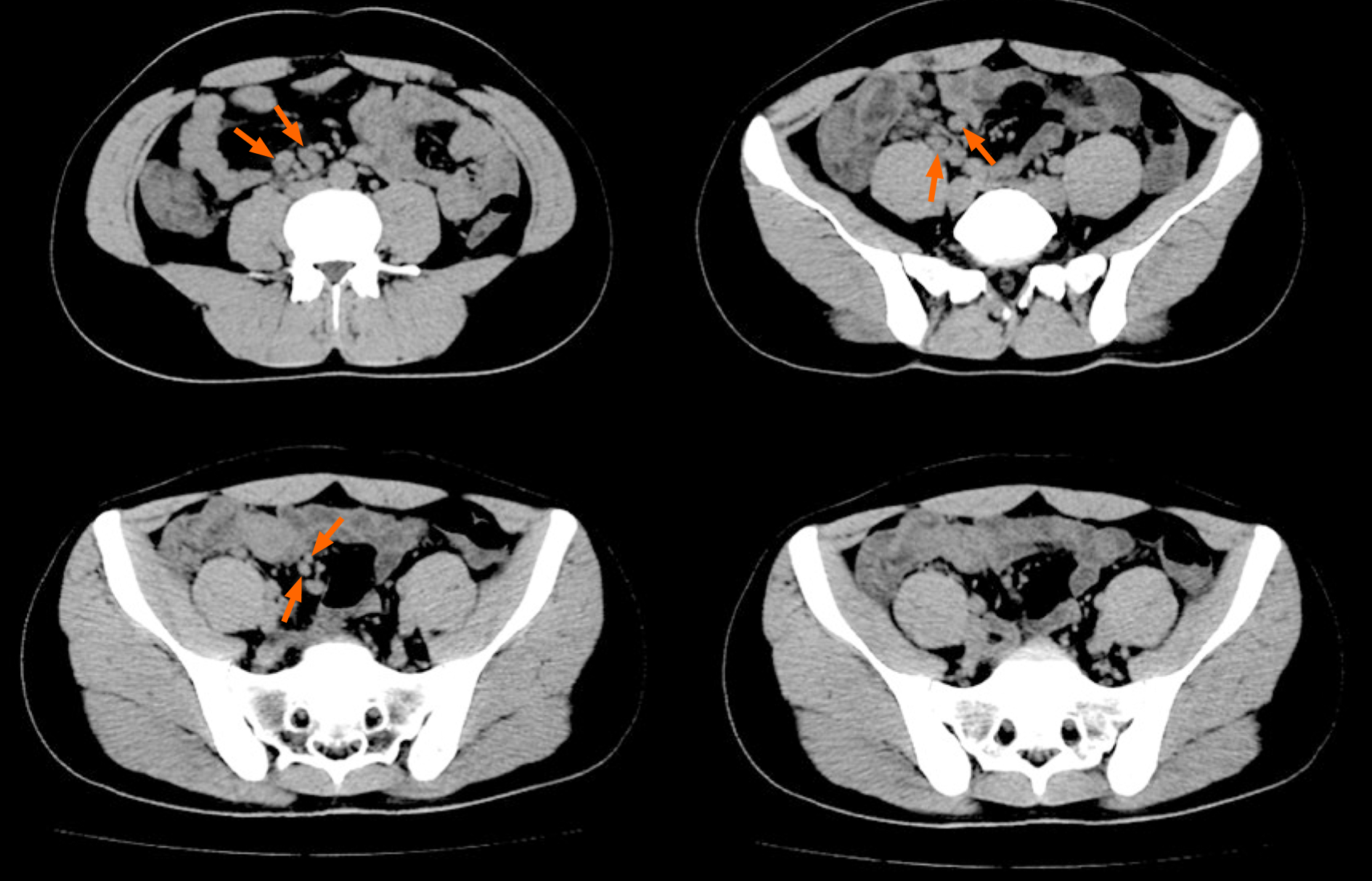
Abdominal computerized tomography (CT) was performed, which revealed a fatty liver and a thickened intestinal wall of the ileocecal junction with multiple enlarged lymph nodes nearby, indicating appendicitis (Figure 1).
Final pathology supported the diagnosis of acute appendicitis. Meanwhile, the blood culture later reported Gram-negative bacillus, which was later tested to be Salmonella species, confirming the diagnosis of Samonella typhi infection.
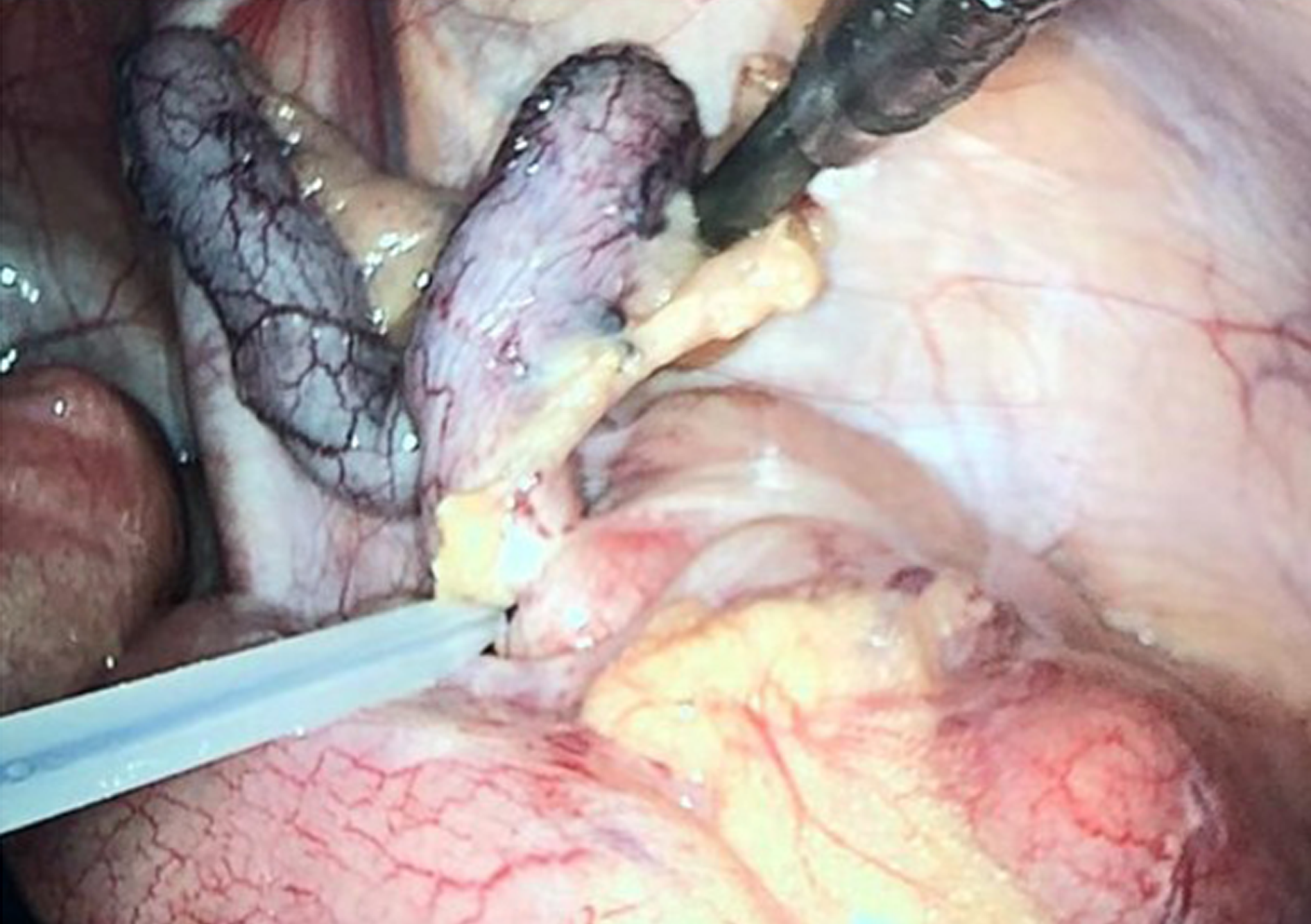
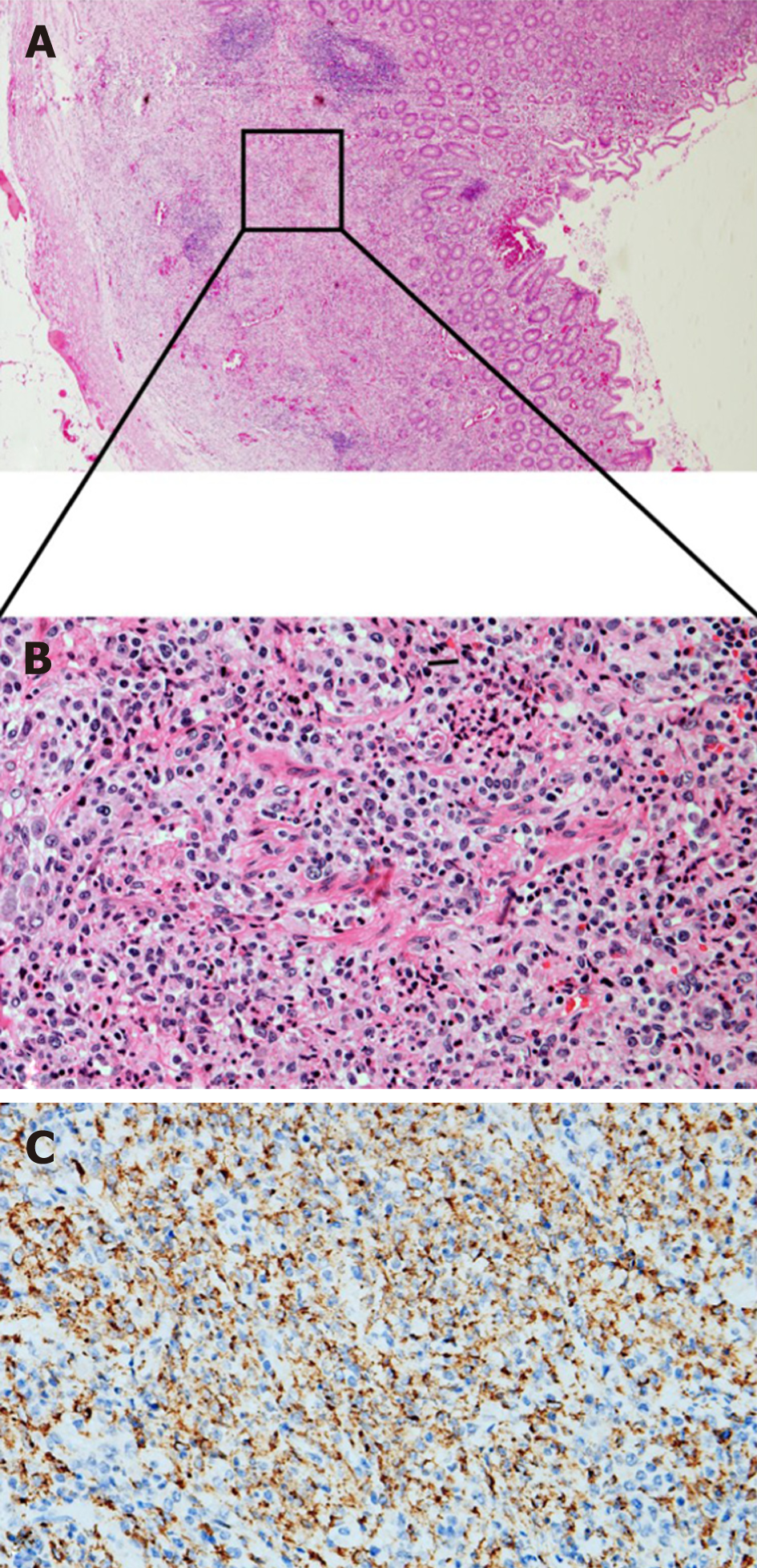
The admission diagnosis that we first considered was acute appendicitis. Therefore, after a general discussion and family agreement, the patient was taken for laparoscopic appendectomy. During the operation, we found a congested, 7 cm long non-perforated appendix with a little exudate (Figure 2). Pathology reported lamina propria hyperplasia and macrophage reactive hyperplasia in the submucosa, and the normal lymphoid follicular structure disappeared in the lamina propria massive macrophage reactive hyperplasia with a small amount of neutrophil and lymphocyte infiltration, and partial mucosal ulcers (Figure 3). Affected tissue was restricted in the lamina propria, while the submucosal and muscle layers were normal. Focal deposition of collagen fibers and neutrophilic invasion were found in the serosal layer, which supported the diagnosis of acute appendicitis.
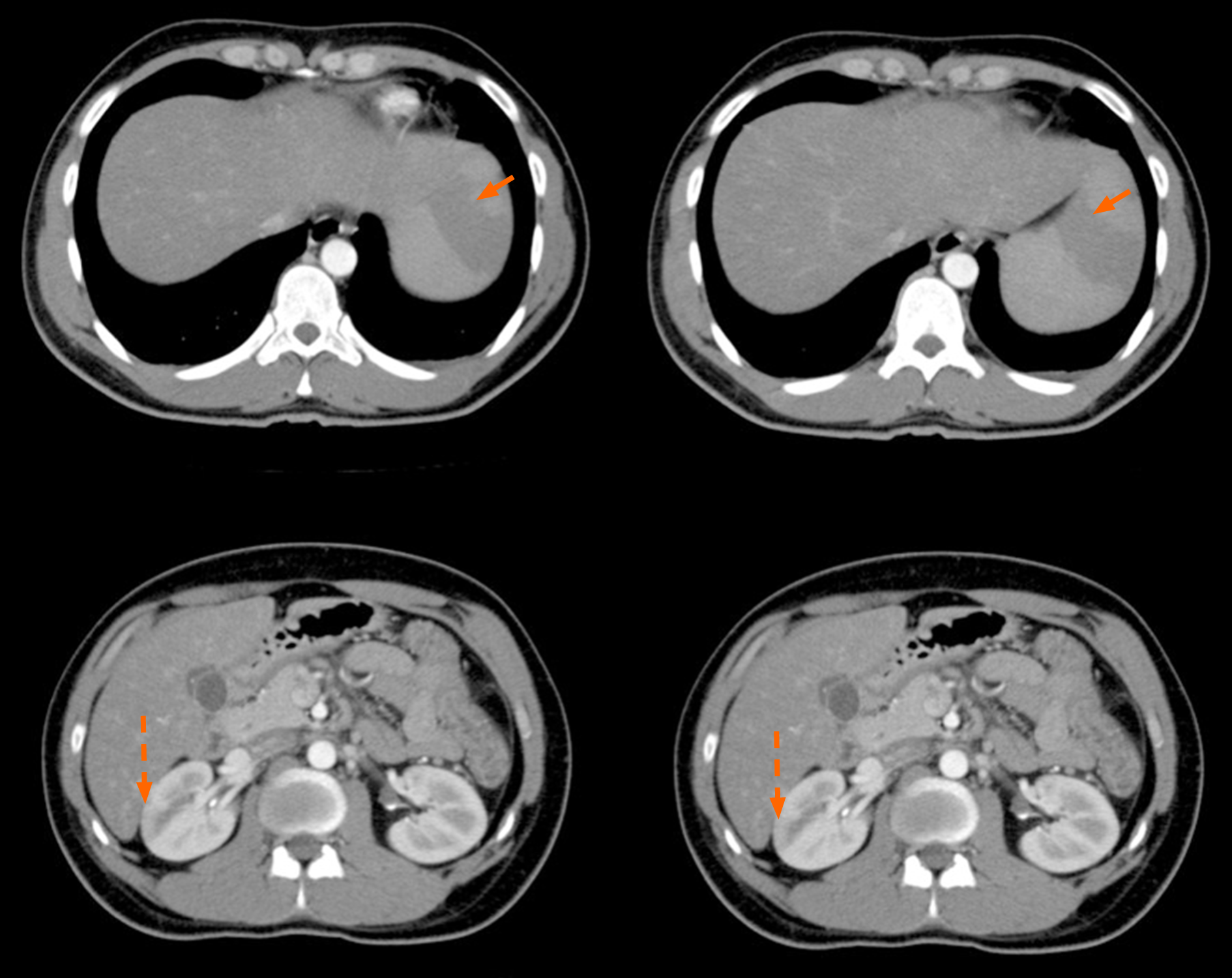
However, on the second post-surgery day, the patient presented again with a high fever of more than 39 °C and diarrhea with loose yellow-green stools. Urine and stool routine tests were performed at once and the fecal occult blood test was positive. Routine blood test showed that WBC was 4.1 × 109 with zero eosinophils, platelet count was 77 × 109/L, and D-dimer was higher than 40 mg/L. Cefoperazone and sulbactam plus metronidazole were used immediately. A CT scan showed swelling of the cecal and ascending colonic wall, with multiple enlarged celiacs and retroperitoneal lymph nodes. A multi-disciplinary consultation was called on differential diagnoses: Secondary abdominal infections, leak of the appendiceal stump, and lymphoma. Considering the inflammation appearance and foreigner identity of the patients, unclear infectious agent from the epidemic area was suspected and the chance of thrombosis was concerned. A CT angiography scan was performed and showed multiple spleen infarctions and right renal infarction (Figure 4). Blood culture later reported Gram-negative bacillus, which turned out to be Salmonella species sensitive to ciprofloxacin, levofloxacin, ceftazidime, and cefaloridine. Levofloxacin and low-molecular-weight heparin were then used intravenously.
The temperature decreased to 37-38 °C within 3 d. This patient's enteric symptoms were also relieved much. He was then transferred to the Shanghai Public Health Clinical Center for further treatment of typhoid fever according to the epidemic prevention provisions. At the 1-mo follow-up, the patient had recovered well.
In this case report, we present a patient with acute appendicitis associated with Samonella typhi infection, thus serving as a rare example of a common surgical emergency.
In general, appendicitis is an infection-related disease, and the infectious agents include viruses, bacteria, fungi, and parasites[9]. In bacterial infections causing appendicitis, Samonella typhi infection-related acute appendicitis has been rarely reported, and clinical presentation and histologic findings are identical to those of acute nonspecific appendicitis[2]. In one case reported by Sartori et al[10], the pathology demonstrated early acute appendicitis as appendiceal lymphoid follicle hyperplasia, neutrophilic invasion in the mucosa, and crypt abscesses. Besides, Boyd reported[11] histologic changes of the appendixes in nine patients dying of typhoid fever, and the main histological change of one case was mucosal hyperplasia and epithelial granuloma formation. Previously, it has been reported that Samonella typhi might invade the intestinal mucosa of the ileocecal junction through M cells gathering at follicle-associated epithelium (FAE)[12], which leads to leucocytes infiltrating into the lamina propria. Some bacteria even went inside intestinal lymphoid tissue and then drained into mesenteric nodes[4]. All these studies might explain the pathological feature of Samonella typhi-related acute appendicitis. Consistent with these previous reports, appendix involvements of typhoid fever in our case presented with milder unspecific inflammation such as lamina propria hyperplasia and neutrophilic invasion, and typical histopathological changes were consistent with intestinal typhoid as partial mucosal ulcers and enlarged lymph nodes. Enlarged lymph nodes and an appendix with mucosal hyperplasia and ulcers were found at the same time in our patient. This might indicate involvements of typhoid inflammation in both the appendix and lymph node system, possibly associated with FAE and lymphoid follicles.
Of note, the appendicitis symptoms in some cases related to typhoid fever can be mimics of mesenteric lymphadenitis[13,14]. In this condition, a normal appendix may be found during laparoscopic exploration. Therefore, careful examinations should be carried out to differentiate mesenteric lymphadenitis from appendicitis in typhoid fever patients.
In a case without early immediate surgery, the patient developed gangrenous appendicitis[15]. Moreover, it has been reported that patients with Salmonella infection-related appendicitis often remain febrile postoperatively, and need antibiotic treatment following appendectomy[2,10]. All these reports supported that Salmonella infection-related appendicitis requires immediate appendectomy and postoperative antibiotic treatment.
Splenic and renal infarction is usually caused by hematological and rheumatological diseases, as well as human immunodeficiency virus (HIV) infection[16]. In our case, rheumatoid factor, antinuclear acid antibody, and HIV tests all showed negative results, which ruled out hematological and rheumatological diseases, and HIV infection. There are few reported cases of splenic infarction and typhoid fever[7,8,17]. However, the possible mechanisms of solid organ infarction in typhoid fever have not been clarified. An animal study has indicated inflammation related to thrombosis via C type lectin-like receptor-2 on platelets in Samonella infections, and the bacteria may colonize solid organs, thus triggering inflammations and thrombosis responses[18].
Epidemic focus and normal WBC also provided significant clues in this case. Southern Asia is a high-risk region for typhoid fever, where our patient came from. Pre- and post-operation routine blood tests all showed normal WBC with zero eosinophils. CT scan gives some hints for pre-surgery differential diagnosis, but not enough to preclude the surgery, especially in cases with suppurative appendicitis.
In conclusion, we here report a rare case of Samonella typhi infection-related acute appendicitis. This case might remind emergency doctors that the etiology of appendicitis needs to be clarified to give appropriate treatment to patients with appendicitis. Besides, some improvements would have been needed in our clinical practice in this case: First of all, enough attention on the patient's epidemic focus history was not paid until the late course of the diagnosis. Second, we only performed a routine stool test without sending a stool sample for bacterial cultivation.
This case, characterized by the association of Salmonella typhi infection with acute appendicitis and renal and splenic infarction, serves as a rare example for a common surgical emergency.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research, and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee KG S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Zhang YL
| 1. | Stewart B, Khanduri P, McCord C, Ohene-Yeboah M, Uranues S, Vega Rivera F, Mock C. Global disease burden of conditions requiring emergency surgery. Br J Surg. 2014;101:e9-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 356] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 2. | Lamps LW. Infectious causes of appendicitis. Infect Dis Clin North Am. 2010;24:995-1018, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Snyder MJ, Guthrie M, Cagle S. Acute Appendicitis: Efficient Diagnosis and Management. Am Fam Physician. 2018;98:25-33. [PubMed] |
| 4. | Bhan, M. K., R. Bahl, and S. Bhatnagar, Typhoid and paratyphoid fever. Lancet. 2005;366:749-762. [RCA] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 321] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 5. | Golakai VK, Makunike R. Perforation of terminal ileum and appendix in typhoid enteritis: report of two cases. East Afr Med J. 1997;74:796-799. [PubMed] |
| 6. | Kazlow PG, Freed J, Rosh JR, Reiner M, Dische R, Benkov K, LeLeiko NS. Salmonella typhimurium appendicitis. J Pediatr Gastroenterol Nutr. 1991;13:101-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Gautier-Benoit C, Pontac MO, Hochedez G, Houcke M. [Splenic infarct revealing paratyphoid fever in a child]. Lille Med. 1975;20:630-631. [PubMed] |
| 8. | Küpeli S, Alehan D, Akpinar E. Isolated splenic infarction owing to group B Salmonella: case report. Ann Trop Paediatr. 2002;22:380-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 535] [Cited by in RCA: 744] [Article Influence: 67.6] [Reference Citation Analysis (1)] |
| 10. | Sartori DJ, Sun K, Hopkins MA, Sloane MF. Typhoid Fever and Acute Appendicitis: A Rare Association Not Yet Fully Formed. Case Rep Gastroenterol. 2017;11:446-451. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Boyd JF. Pathology of the alimentary tract in Salmonella typhimurium food poisoning. Gut. 1985;26:935-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 53] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Pier GB, Grout M, Zaidi T, Meluleni G, Mueschenborn SS, Banting G, Ratcliff R, Evans MJ, Colledge WH. Salmonella typhi uses CFTR to enter intestinal epithelial cells. Nature. 1998;393:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 222] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 13. | Likitnukul S, Wongsawat J, Nunthapisud P. Appendicitis-like syndrome owing to mesenteric adenitis caused by Salmonella typhi. Ann Trop Paediatr. 2002;22:97-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Martin HC, Goon HK. Salmonella ileocecal lymphadenitis masquerading as appendicitis. J Pediatr Surg. 1986;21:377-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Stewart-Parker EP, Atta M, Doddi S. A curious cause of appendicitis. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Nores M, Phillips EH, Morgenstern L, Hiatt JR. The clinical spectrum of splenic infarction. Am Surg. 1998;64:182-188. [PubMed] |
| 17. | Mehta LK, Arya SC, Mathai G. Infarction of the spleen in typhoid fever. Saudi Med J. 2007;28:271-272. [PubMed] |
| 18. | Hitchcock JR, Cook CN, Bobat S, Ross EA, Flores-Langarica A, Lowe KL, Khan M, Dominguez-Medina CC, Lax S, Carvalho-Gaspar M, Hubscher S, Rainger GE, Cobbold M, Buckley CD, Mitchell TJ, Mitchell A, Jones ND, Van Rooijen N, Kirchhofer D, Henderson IR, Adams DH, Watson SP, Cunningham AF. Inflammation drives thrombosis after Salmonella infection via CLEC-2 on platelets. J Clin Invest. 2015;125:4429-4446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 138] [Article Influence: 12.5] [Reference Citation Analysis (0)] |