Published online Sep 16, 2021. doi: 10.12998/wjcc.v9.i26.7870
Peer-review started: March 29, 2021
First decision: June 24, 2021
Revised: July 6, 2021
Accepted: August 13, 2021
Article in press: August 13, 2021
Published online: September 16, 2021
Processing time: 164 Days and 14.7 Hours
Mediastinal mature teratoma is the most common histological type of primary extragonadal germ cell tumor. In this report, we describe a rare case of giant mature teratoma located primarily in the anterior mediastinum and causing partial atelectasis of the upper and middle lobes of the right lung, as well as extrinsic compression of the right atrium.
A 31-year-old male with a giant mediastinal mature teratoma presented with progressive exertional dyspnea and chest pain for 1 mo. Computed tomography of the chest indicated the diagnosis of anterior mediastinal teratoma. The patient underwent right uniportal anterior approach video-assisted thoracoscopic surgery (VATS). En bloc resection of the giant teratoma, wedge resection of the upper and middle lobes of the right lung, resection of the thymus and partial excision of the pericardium were successfully performed. The pathological diagnosis revealed a mature cystic teratoma with foreign-body reaction that was closely related to the right lung, atrium dextrum, superior vena cava and ascending aorta. An atrophic thymic tissue was also discovered at the external teratoma surface. The patient was discharged on postoperative day 7.
This is the first report of the use of uniportal VATS for complete resection of a teratoma in combination with wedge resection of the right upper and middle lung lobes and partial resection of the pericardium.
Core Tip: Mediastinal mature teratoma accounts for the majority of primary germ cell tumors in the mediastinum, which can be resected by traditional surgery. We present a rare case of mediastinal mature teratoma with complex adhesions and infiltration resected using uniportal video-assisted thoracoscopic surgery (VATS) technology. The patient had no postoperative complications and was completely asymptomatic at the first-year postoperative follow-up. As VATS currently plays an increasingly significant role in the therapy of teratomas, our report indicated that uniportal VATS for resection of mediastinal teratomas with complex adhesions and infiltration can be successfully conducted.
- Citation: Hu XL, Zhang D, Zhu WY. Uniportal video-assisted thoracoscopic surgery for complex mediastinal mature teratoma: A case report. World J Clin Cases 2021; 9(26): 7870-7875
- URL: https://www.wjgnet.com/2307-8960/full/v9/i26/7870.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i26.7870
Germ cell tumors, frequently observed in the gonads, can also be found in the (anterior) mediastinum, which is the most predominant extragonadal site, and manifests as a mature teratoma accounting for the majority of primary germ cell tumors in the mediastinum[1]. Most mediastinal mature teratomas are insidious and therefore are generally discovered during abnormal medical examinations. Teratomas usually compress adjacent structures, predominantly altering the respiratory and circulatory systems[2]. Another typical feature of mediastinal mature teratoma is tumor bleeding or rupture into the bronchus, pleura, vessel, or pericardium[3]. Mediastinal mature teratoma can be definitively diagnosed by histopathological examination as the tumors are generally composed of ectodermal, mesodermal, and endodermal derivatives[4]. Video-assisted thoracoscopic surgery (VATS) technology has evolved from its multiport origins to even less invasive approaches due to its identified advantages compared with open surgery for a series of thoracic cavity tumors[5]. During the course of its evolution, Uniportal VATS (UniVATS) has emerged, which has proved to be superior to multiport VATS and has extended the surgical boundaries[6]. In the present case, we describe a giant mature teratoma in the anterior mediastinum of a 31-year-old male with complex rupture into the right lung and compression of the right atrium, as well as the superior vena cava and ascending aorta, which was completely resected using UniVATS.
A 31-year-old male patient was admitted to our hospital complaining of progressive chest pain, exertional dyspnea and cough, accompanied by recurrent hemoptysis, and a low-grade fever. The patient had been treated with antibiotics for 5 d, but this was unsuccessful in relieving his symptoms.
Chest pain and exertional dyspnea in this patient started 6 wk ago, and recurrent hemoptysis developed 10 d previously.
The patient had no previous medical history.
The patient had no disease-related personal or family history.
Physical examination on admission showed that the patient was normothermic and normotensive, without tachypnea, cyanosis or tachycardia. In addition, no abnormalities of features, thyroid, lung fields, abdomen, skin, arms and legs, lymph nodes, or testicles were observed during the examination. Neurological examination and routine stool as well as urine analysis were generally within normal limits. A 12-lead resting electrocardiogram demonstrated sinus rhythm.
Routine blood test showed a slightly higher C-reactive protein level of 12.98 mg/L, suggesting a mild inflammatory response. Tumor markers, such as CEA, AFP, CA-125, NSE, β-HCG, and CA 19-9, were within normal ranges, except for TK1 (5.60 pmol/L). In addition, no abnormalities were found following respiratory function tests. Transthoracic echocardiography in the parasternal view revealed a normal-sized heart with normal function and blood flow velocities.
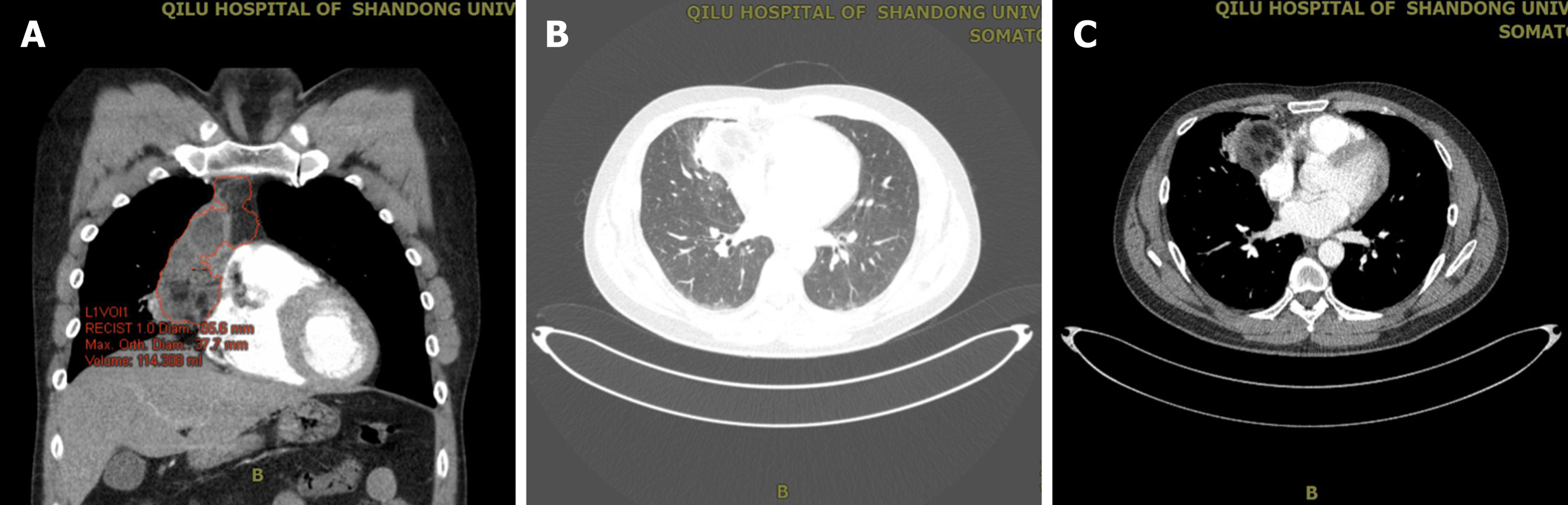
An earlier computed tomography (CT) report from a local hospital showed a large oval mass measuring approximately 9.0 cm × 6.0 cm × 5.0 cm in the anterior mediastinum. To further define the location, nature, composition, characteristics, and operability of the tumor, contrast-enhanced CT of the chest and soft tissue three-dimensional reconstruction were performed, which confirmed the presence of a right anterior mediastinal mass with extrinsic compression of the right atrium and right lung (Figure 1).
Moreover, contrast-enhanced CT further revealed an oval, polycystic, heterogeneous mass with fatty, liquid and calcified components in the right anterior mediastinum, measuring 8.3 cm × 4.4 cm × 4.8 cm in size. The mass was closely related to the surrounding tissues and organs, presenting as infiltration of the right upper and middle lobes with pneumonitis, and encased the origin or terminal of the superior vena cava as well as the ascending aorta. Heterogeneous enhancement of the mass was confirmed following administration of Ultravist 300.
The final diagnosis in the presented case was mediastinal mature teratoma.
The patient underwent VATS via a uniportal right-sided anterior approach with surgical resection via the 5th intercostal space on day 7 after admission. The extracorporeal circulation system was prepared in advance for possible intraoperative haemorrhage. Intraoperative thoracoscopic exploration revealed extensive adhesions around the thorax, including a large mass measuring approximately 9 cm × 6 cm × 5 cm, located in the right anterior mediastinum. The tumor was located above the superior border of the left brachiocephalic vein and was partially solid and cystic in nature. Moreover, the tumor was adjacent to the pericardium, the terminal superior vena cava and the left brachiocephalic vein, and infiltrated the right upper and middle lung lobes and the right phrenic nerve, and it was extremely difficult to separate the mass. We therefore performed en bloc resection of the giant teratoma, a wedge resection of the upper and middle lobes of the right lung, and partial pericardial resection in this patient. The tumor was resected with utmost care to preserve vital structures, such as the phrenic nerve, recurrent laryngeal nerve, aorta, superior vena cava, left brachiocephalic vein, pulmonary vessels, and subclavian vessels. In addition, the enlarged mediastinal lymph nodes and the right portion of the thymus were also resected to ensure that no tumor tissue remained. Basal thoracostomy tubes were placed.
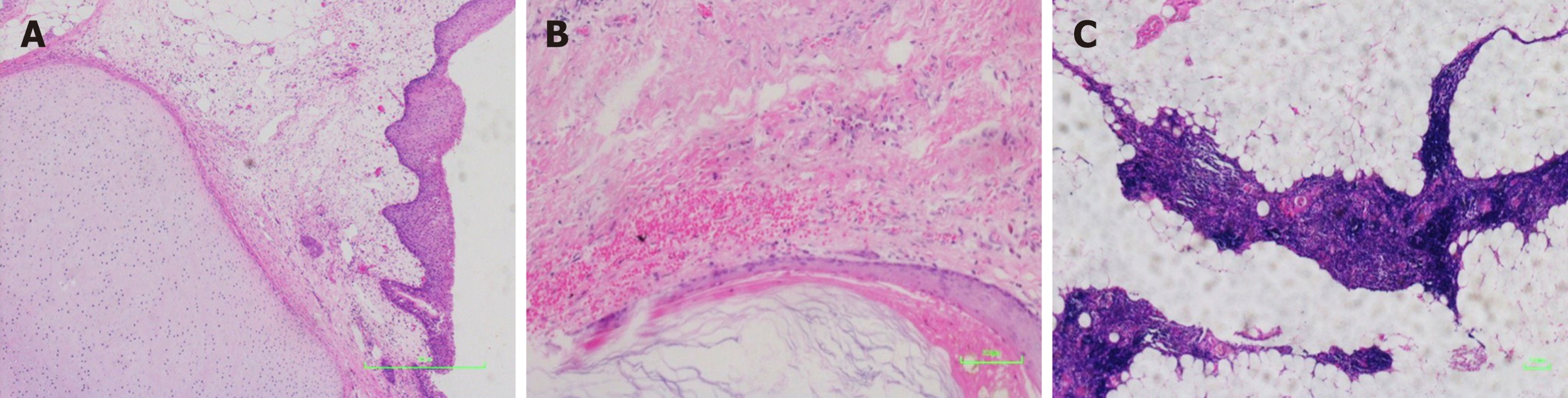
The gross pathological diagnosis revealed a predominantly mature cystic teratoma with a foreign-body reaction that measured 10 cm × 6 cm × 4.5 cm (Figure 2). The tumor infiltrated the lung, and the tissue was filled with sebaceous materials. An immunohistochemical diagnosis was conducted and showed positive markers of epithelial as well as T cells. However, neither mesenchymal nor neural elements were observed (data not shown). Moreover, there was no histological or morphological evidence of malignancy in the tumor (Figure 3). In addition, atrophic thymus and inflammatory lymph nodes were observed in the tissue surrounding the tumor.
The patient had no post-operative complications, and was discharged on the 7th post-operative day. Moreover, he was completely asymptomatic at the first-year post-operative follow-up.
Mature teratomas comprise the vast majority of all histological types of germ cell tumors, which predominantly originate from the gonads. Extragonadal germ cell tumors are found in the mediastinum, peritoneum, sacral pineal gland, thyroid, and gastrointestinal tract, of which the anterior mediastinum is the most frequent extragonadal site and these tumors are named mediastinal teratomas[7]. Mediastinal teratoma should be differentiated from a series of thoracic tumors, including mediastinal lymphomas, thymomas, esophageal cysts, bronchogenic cysts, pericardial tumors, lymphangiomas, neurogenic tumors, and mesenchymal tumors[8].
The majority of mediastinal teratomas are benign, which means the tumors grow quite slowly and are almost asymptomatic in the early stages. Few cases of rapidly growing mediastinal mature teratomas have been published. Thus, most of these tumors were diagnosed incidentally during medical examination[9]. However, the specific mechanism of action of mediastinal mature teratoma development is unclear. It is documented that tumors which proliferated and grew to a certain extent could induce extrinsic compression of adjacent vital structures, which results in representative clinical symptoms including chest congestion, bronchial cough, blood-streaked phlegm, hemoptysis, as well as dyspnea[10]. Moreover, the tumors can also rupture into adjacent structures, such as the pericardium, bronchus, and pleural space, where sebaceous materials or hair can be observed by electric bronchoscope or fine needle aspiration biopsy. As an extreme example, a case report illustrated a mature mediastinal teratoma with complex rupture into the skin with a cysto-cutaneous fistula, which produced sebum and hair[7]. Some teratomas contain malignant components, indicating that radiotherapy and chemotherapy may be acceptable management options[11].
In clinical practice, the most effective diagnostic modality for mediastinal teratomas is CT, which provides unambiguous signs of tumor rupture as well as infiltration of adjacent structures, crucial for early diagnosis and surgical decisions[12].
Surgical resection is the mainstay of teratoma treatment, particularly for mature teratomas. The choice of surgical approach for mediastinal teratomas depends to a large extent on the size, location, invasiveness, histological classification, metastases, the relationship of the tumor to the relevant vital structures, as well as the experience of the surgeon. Traditionally, a lateral, anterolateral or median sternotomy is the primary approach for resecting teratomas[11]. Moreover, robotic surgery and VATS-assisted surgery are increasingly used in the surgical excision of mediastinal tumors[13]. In recent years, the application of VATS has played an important role in thymectomy, which also provides the rational for teratoma resection[6,14]. However, there are few reports on the application of VATS to resect mediastinal teratomas. There are always extensive and widespread adhesions between mediastinal teratomas and adjacent vital organs and tissues. In addition, some teratomas are also inflamed, infiltrated, and ruptured. Therefore, great care must be taken during resection of the tumor. Serious cardiopulmonary complications, such as hemorrhage, cardiac arrest, and diaphragmatic paralysis, may occur when adjacent vital structures are damaged[15]. In addition, some anesthesia-related problems may occur during mediastinal tumor excision due to adjacent structures such as the superior vena cava. For example, Kumar et al[16] reported a case of intraoperative catastrophe during benign medi
Mediastinal mature teratomas are uncommon, asymptomatic benign tumors that are often diagnosed on CT scans obtained for unrelated reasons. Complete surgical excision is the best treatment for mediastinal teratomas. Currently, VATS plays an increasingly significant role in the treatment of teratomas. Our report revealed that UniVATS for the resection of mediastinal teratomas with complex adhesions and infiltration can be successfully conducted.
| 1. | Zheng R, Devin CL, O'Malley T, Palazzo F, Evans NR 3rd. Surgical management of growing teratoma syndrome: robotic-assisted thoracoscopic resection of mediastinal teratoma. Surg Endosc. 2020;34:1019-1023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Tian Z, Liu H, Li S, Chen Y, Ma D, Han Z, Huang C. Surgical treatment of benign mediastinal teratoma: summary of experience of 108 cases. J Cardiothorac Surg. 2020;15:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Vieira RD, Grimberg H, Uezumi KK, Demarchi LM, Tsutsui JM, Lopes NH, Hueb W. Teratoma of the mediastinum: a case report. J Med Case Rep. 2011;5:193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Ghritlaharey RK. Mature Teratoma at Left Lumbar Region in an Infant: A Case Report. J Clin Diagn Res. 2016;10:PD22-PD23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Xie D, Deng J, Gonzalez-Rivas D, Zhu Y, Jiang L, Jiang G, Chen C. Comparison of video-assisted thoracoscopic surgery with thoracotomy in bronchial sleeve lobectomy for centrally located non-small cell lung cancer. J Thorac Cardiovasc Surg. 2021;161:403-413.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Bulgarelli Maqueda L, García-Pérez A, Minasyan A, Gonzalez-Rivas D. Uniportal VATS for non-small cell lung cancer. Gen Thorac Cardiovasc Surg. 2020;68:707-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Serraj M, Lakranbi M, Ghalimi J, Ouadnouni Y, Smahi M. Mediastinal mature teratoma with complex rupture into the lung, bronchus and skin: a case report. World J Surg Oncol. 2013;11:125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Zhao H, Zhu D, Zhou Q. Complete resection of a giant mediastinal teratoma occupying the entire right hemithorax in a 14-year-old boy. BMC Surg. 2014;14:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Koçinaj D, Krasniqi X, Bakalli A. Immature teratoma mimicking pulmonary stenosis: a case report. J Med Case Rep. 2018;12:125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Ahmed MA, Fouda R, Ammar H, Amin SM. Massive pericardial effusion and multiple pericardial masses due to an anterior mediastinal teratoma rupturing in pericardial sac. BMJ Case Rep. 2012;2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Lin C, Du Y, Li Y, Wang H, Chang J. Superior mediastinal mature cystic teratoma with gastrointestinal adenocarcinoma transformation: Report of a case. Oncotarget. 2016;7:38392-38397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Yalagachin GH. Anterior mediastinal teratoma- a case report with review of literature. Indian J Surg. 2013;75:182-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Kermenli T, Azar C. Evaluation of surgical procedures in primary mediastinal cysts and tumors: single-center experience. Kardiochir Torakochirurgia Pol. 2019;16:109-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Gross DJ, Zangbar B, Muthu N, Chang EH, Badami A, Stein L, Gruessner R, Poston R. Saving the split: the benefits of VATS thymectomy. J Thorac Dis. 2019;11:1428-1432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Stella F, Davoli F. Giant mediastinal mature teratoma with increased exocrine pancreatic activity presenting in a young woman: a case report. J Med Case Rep. 2011;5:238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Kumar A, Persuad P, Shiwalkar N. Intraoperative Catastrophe during Benign Mediastinal Tumor Mass Excision: A Case Report. Cureus. 2019;11:e4941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kermenli T, Kumar A, Yalçinkaya İ S-Editor: Gao CC L-Editor: A P-Editor: Zhang YL