Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7022
Peer-review started: March 11, 2021
First decision: April 4, 2021
Revised: May 13, 2021
Accepted: July 5, 2021
Article in press: July 5, 2021
Published online: August 26, 2021
Processing time: 165 Days and 16.8 Hours
Distal radius fractures accompanied by the volar margin of the lunate fossa (VMLF) lesions are often overlooked or inadequately reduced in clinical practice.
To investigate the impact of VMLF fragment in distal radius fractures on the stability and function of the wrist joint.
This was a retrospective study of patients with distal radius fractures who underwent surgical treatment between January 2013 and December 2017. The patients were divided into two groups according to whether the VMLF fragments were fixed or not. X-rays and computed tomography were performed before surgery, immediately postoperatively, and at 1, 3, and 6 mo to measure the scapholunate angle, radiolunate angle, capitolunate angle, and effective radiolunate flexion (ERLF). The Mayo wrist score and disabilities of the arm, shoulder, and hand (DASH) score were determined at 1 year.
Thirty-five patients were included. There were 15 males and 20 females. Their mean age was 52.5 ± 14.3 (range: 19-70) years. There were 38 wrists (17 on the left side, 15 on the right, and three bilateral; 16 in the fixed group, and 22 in the unfixed group). The interval between trauma and surgery was from 1 h to 1 mo. The incidence of postoperative wrist instability in the unfixed group (86.4%) was higher than in the fixed group (25.0%) (P ≤ 0.001). Ten patients had ERLF > 25° in the unfixed group and none in the fixed group (P = 0.019). The Mayo wrist score was 94 ± 5.7 in the fixed group and 68 ± 15.1 in the unfixed group (P < 0.001). The DASH score was 4.6 ± 2.5 in the fixed group and 28.5 ± 19.5 in the unfixed group (P < 0.001).
Injuries of VMLF, even small fractures, might damage the radial-lunar ligament, leading to postoperative wrist instability, sagittal force line imbalance, and poor recovery of wrist joint function.
Core Tip: This study aimed to examine the impact of volar margin of the lunate fossa fragment in distal radius fractures on the stability and function of the wrist joint. The results suggested that the number of patients with pathological carpal malalignment in the unfixed group was significantly higher than that in the fixed group. All cases in the fixed group had an excellent/good functional outcome. In the unfixed group, six of 22 cases had an excellent/good outcome, and 16 of 22 cases had a fair-poor functional outcome.
- Citation: Meng H, Yan JZ, Wang B, Ma ZB, Kang WB, Liu BG. Influence of volar margin of the lunate fossa fragment fixation on distal radius fracture outcomes: A retrospective series. World J Clin Cases 2021; 9(24): 7022-7031
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7022.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7022
Distal radius fractures are common and represent 25%-50% of all bone fractures[1,2]. Distal radius fractures have a bimodal peak in incidence; it classically occurs in young male patients with high-energy injuries and predominantly in elderly female patients sustaining low-energy, osteoporotic fractures[3,4]. Most patients can be managed as outpatients after reduction and immobilization. The decision for operative repair is multifactorial (age of the patient, baseline functional mobility, hand dominance, instability of fracture, disruption of the radiocarpal and radioulnar ligaments, and comorbidities). Fractures associated with neurovascular injuries need emergent reductions[3,5-7].
Nevertheless, even with the development of modern implants that allow early mobilization, the long-term outcomes have not significantly improved[3,8,9]. Associated lesions in the ligaments or cartilage might contribute to this problem[3,8-11]. Although fracture reduction and fixation of some cases show good image findings, the long-term follow-up of patients with distal radius fractures suggests that poor wrist function is accompanied by instability and sagittal malalignment[3,8,9]. In clinical practice, the adaptive response of the carpus to the loss of the normal architecture due to distal ulnar and radius fractures results in lunate deformity[12,13].
Distal radius fracture accompanied by a fracture of the volar margin of the lunate fossa (VMLF) is uncommon in clinical practice[14]. The definition of the injury mechanism and fixation method for the treatment of VMLF fracture still has no consensus. When the VMLF fragment is large, the carpus always subluxates with a part of the distal radius articular surface, and it is conspicuous and easy to diagnose, but when it is sufficiently small, the carpus position and distal radius articular surface may appear to be normal in the initial X-ray[15,16]. Distal radius fractures accompanied by VMLF lesions are often overlooked or inadequately reduced in clinical practice. The short radiolunate ligament (SRL) originates from the VMLF of the distal radius and attaches to the palmar aspect of the lunate, maintaining the stability of the radiolunate joint and the sagittal alignment of the wrist joint. Distal radius fractures with VMLF fragments can damage the attachment of the SRL or even injure it directly[16-18].
This study aimed to report a series of cases in which the postoperative stability, function, and sagittal alignment of the wrist joint were measured after distal radius fractures accompanied by VMLF lesions. Our hypothesis was that effective reduction and fixation of the VMLF are important to maintain the stability of the wrist joint and sagittal alignment and that repair of the SRL should be considered.
This was a retrospective study of patients with distal radius fractures who underwent surgical treatment at the Department of Orthopedics of Beijing Tiantan Hospital between January 2013 and December 2017. The study was performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The requirement for informed consent was waived due to the retrospective nature of the study.
The inclusion criteria were: (1) Distal radius fracture in a skeletally mature patient (i.e., > 18 years of age); (2) distal radius fracture accompanied by VMLF fracture fragments (i.e., the pieces were detached from the VMLF) according to computed tomography (CT); (3) operative treatment (regardless of the type of fixation method used); and (4) radiological films available (before and after the operation and at 1-, 3-, and 6-mo follow-ups). The exclusion criteria were: (1) Open fracture; (2) multiple fractures of the ipsilateral upper arm; or (3) preexisting functional impairment of the involved upper extremity.
From 2013 to 2017, a total of 216 patients with distal radius fractures underwent surgical treatment. Among them, there were 37 patients with VMLF fractures. Two patients were lost to follow-up. Therefore, 35 patients (38 wrists) were included in the study.
The patients were divided into two groups according to whether the VMLF fragments were fixed or not. The fractures were classified according to the Association for Osteosynthesis/Association for the Study of Internal Fixation classification[19].
The operations were performed by the department’s chief surgeon and deputy chief surgeon, who have both worked for more than 18 years in the hospital. The indication for operative treatment was a comminuted fracture zone combined with a tilting of ≥ 20° and radial shortening of ≥ 5 mm on the initial X-ray, according to the guidelines of the German Society for Trauma for distal radius fractures[20].
For volar fixation, a volar incision of about 6 cm in length was made between the radial artery and the flexor carpi radialis tendon. The pronator muscle was cut to expose the fracture, which was then reduced and fixed with a volar plate. According to the degree of fracture comminution, auxiliary screws or Kirschner wire internal fixation could be used. After reduction and fixation were satisfying, the pronator muscle was repaired, and the incision was sutured. If the fracture was severely comminuted, external fixation with plaster or brace was provided after the operation.
In dorsal fixation surgery, a dorsal incision, about 4 cm in length, was made to enter between the extensor wrist and extensor digitorum muscles, reveal the fracture, reduce it, and fix it with a dorsal plate. After reduction and fixation were confirmed, the incision was sutured.
During postoperative care, the patients were instructed to raise the affected limb for 1 wk, start passive functional exercises of the metacarpophalangeal and interphalangeal joints after recovery from anesthesia, and after 2-3 d, gradually perform active functional exercises of the metacarpophalangeal and interphalangeal joints. Patients with external fixation were asked to gradually perform active wrist exercises starting 3 d after surgery. The length of operation was about 1 h for only volar or dorsal fixation. Fixing the VMLF took about 30 min.
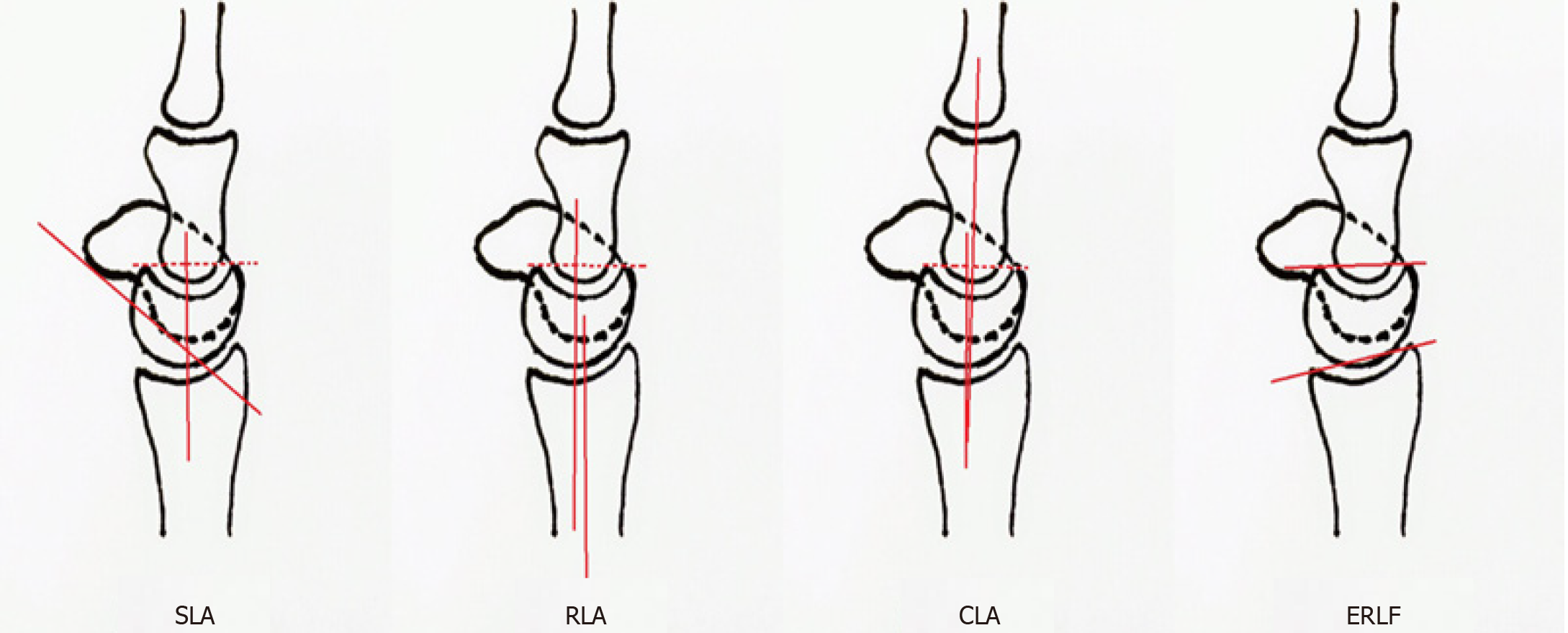
Pain, functional status, range of motion (ROM), grip strength, daily life status, and X-ray and CT data (preoperative, immediately postoperative, 1 mo, 3 mo, and 6 mo) were retrieved from the patient charts. All films were taken in the standard position with the forearm in neutral rotation. The measured radiological parameters were: (1) Scapholunate angle (SLA) (an average of 47° with a range of 30° to 60°); (2) radiolunate angle (RLA) (an average of 0° with a range of -15° to +15°); and (3) capitolunate angle (CLA) (an averages of 0° with a range of -15° to +15°)[14]. According to the diagnostic criteria for wrist instability, SLA, RLA, and CLA outside the range indicated wrist instability (dorsal intercalated segment instability or volar intercalated segmental instability)[21] (Figure 1).
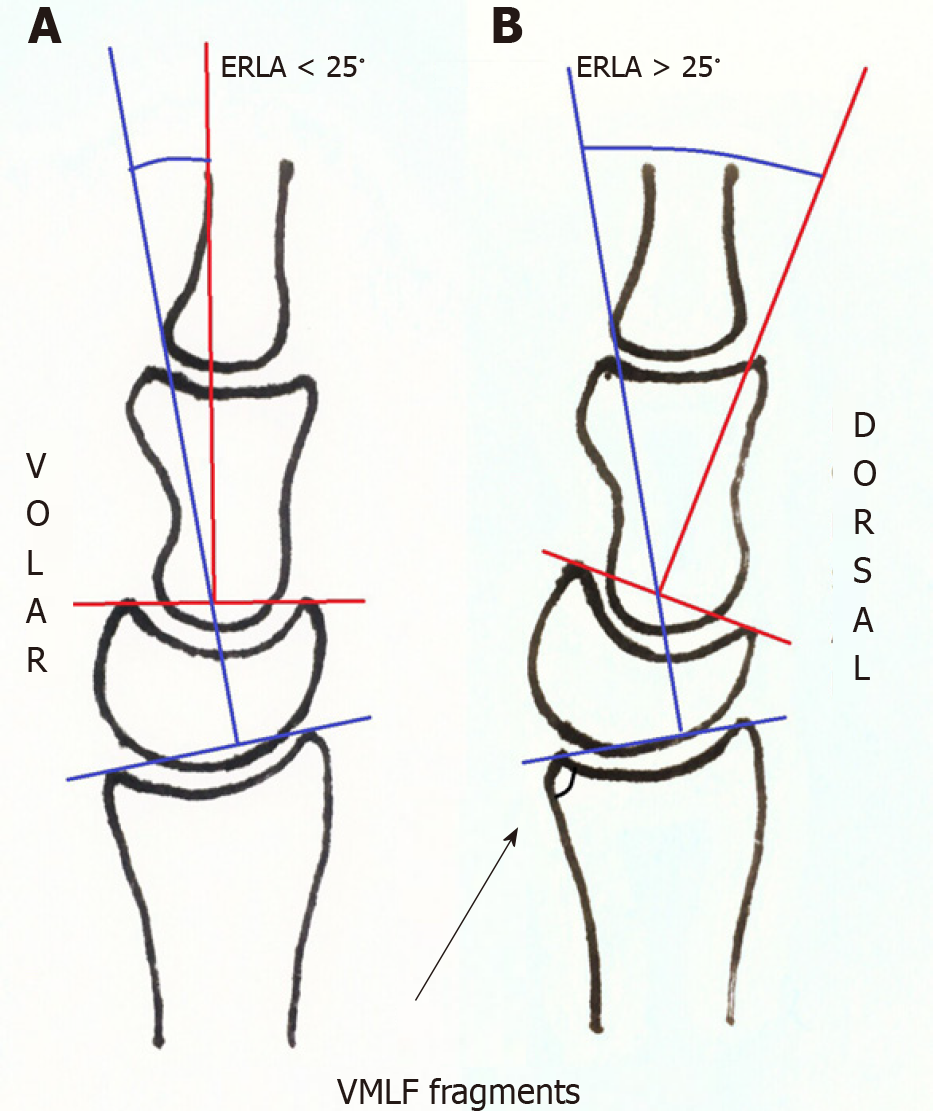
The effective radiolunate flexion (ERLF) denotes the relative flexion of the lunate [22] (Figure 1). Multiple measurements of ERLF during follow-up enabled the identification of pathologic carpal malalignment[22-24]. Distal radius fractures with ERLF < 25° were considered to have an "adaptive" sagittal malalignment. Neither the radiocarpal capsule nor the carpal ligaments were injured, and the malalignment reflects only the adaptation to the lesions[22]. Fractures showing ERLF > 25° were with sagittal malalignment beyond the physiological range, producing dorsal subluxation of the radiolunate joint and resulting in pathologic radiocarpal malalignment[22-24] (Figure 2).
One year after surgery, the Mayo wrist score and the disabilities of the arm, shoulder, and hand (DASH) score were used to evaluate the disability of the wrist. The Mayo wrist score includes not only subjective criteria (pain, restriction of activity, and grip strength) but also objective data (loss of ROM). A score of 90-100 represents an excellent outcome, 80-90 represents a good outcome, 60-80 represents a fair outcome, and < 60 represents a poor outcome. The main part of the DASH is a 30-item disability/symptom score concerning the patient's health status during the preceding week[25]. The items evaluate the degree of difficulty in performing different physical activities because of the arm, shoulder, or hand problems (21 items), the severity of each of the symptoms of pain, activity-related pain, tingling, weakness, and stiffness (five items), and the impact of these problems on social activities, work, sleep, and self-image (four items). Each item has five response options. The scores for all items are then used to calculate a scale score ranging from 0 (no disability) to 100 (the most severe disability)[26].
The data were analyzed using SPSS 17.0 for Windows (IBM, Armonk, NY, United States) and Minitab 15 (Minitab, Inc., State College, PA, United States). Continuous data were tested for normal distribution using the Shapiro-Wilk test and for homogeneity of variance using Levene’s test. All continuous data were found to be normally distributed and have homogeneous variance. They are presented as the means ± SD, minimum, and maximum and were analyzed using Student’s t-test. Categorical data are presented as n (%) and were analyzed using Fisher’s exact test. Two-sided P < 0.05 were considered statistically significant.
The sample size is small and from a single center. According to the authors’ experience, the difference of Mayo or DASH between two non-paired groups was expected to be 20-25[27]. Considering an SD of 20 in each group and a power of 0.8, the sample size was calculated to be 11-18/group using the R software (https://www.R-project.org/). Since the two groups included 16 and 22 patients, respectively, it can be considered that the power reached 0.8.
Table 1 shows the characteristics of the patients. There were 15 males and 20 females. Their mean age was 52.5 ± 14.3 (range: 19-70) years. The interval between the trauma and surgery was from 1 h to 1 mo. There were 38 wrists involved (17 on the left side, 15 on the right, and three bilateral). There were no differences in patient characteristics between the two groups (P > 0.05). The patients were divided into two groups according to whether the VMLF fragments were fixed (n = 16) or not (n = 22). There were no significant differences between the two groups for any of the characteristics. The average duration of follow-up was 12 mo (11-15 mo, 13.1 ± 1.6 mo). All included patients showed no complications such as infection, nonunion of fracture, loosening of internal fixation, or rupture.
| Group | Fixed, n = 16 | Unfixed, n = 22 | P value |
| Sex, n (%) | 0.052 | ||
| Male | 4 (25) | 13 (59.1) | |
| Female | 12 (75) | 9 (40.9) | |
| Age (yr) | 54.0 ± 16.0 | 51.4 ± 13.2 | 0.59 |
| Radius fracture, n (%) | 0.19 | ||
| B1 | 1 (6.3) | 2 (9.1) | |
| B3 | 4 (25) | 8 (36.4) | |
| C1 | 3 (18.7) | 0 (0) | |
| C2 | 0 (0) | 2 (9.1) | |
| C3 | 8 (50) | 10 (45.5) | |
| Imaging features | AO classification | AO classification | |
| Reduction and fixation of the VMLF fragments, n (%) | Fix with screws or sutures | Fracture is small and not fixed | |
| Fixed with AO distal radius volar locking plates | 14 (87.5) | 18 (81.8) | 0.582 |
| Volar and dorsal locking plates | 2 (12.5) | 1 (4.5) | 0.582 |
| Dorsal locking plate | 0 (0) | 1 (4.5) | 1.0 |
| Locking plates and ancillary fixation with Kirschner wires or screws | 0 (0) | 2 (9.1) | 0.4993 |
| External fixation with plaster | 6 (37.5) | 11 (50) | 0.6638 |
In the fixed group, four (25.0%) of 16 patients developed instability; none were in the radiolunate joint. In the unfixed group, 19 (86.4%) of 22 patients developed instability, and all were in the radiolunate joint (Table 2). The difference in instability occurrence was significant (P < 0.001). In the fixed group, none showed ERLF > 25°. In the unfixed group, 10 (45.5%) of 22 patients showed ERLF > 25° (P = 0.019) (Table 2). The number of patients with pathological carpal malalignment in the unfixed group was significantly higher than that in the fixed group.
| Group | Fixed, n = 16 | Unfixed, n = 22 | P value |
| Wrist instability at 1, 3, and 6 mo | < 0.001 | ||
| Instability, n (%) | 4 (25) | 19 (86.4) | |
| DISI | 4 | 19 | |
| VISI | 0 | 0 | |
| Stability, n (%) | 12 (75) | 3 (13.6) | |
| ERLF, n (%) | 0.019 | ||
| > 25° | 0 (0) | 10 (45.5) | |
| ≤ 25° | 16 (100) | 12 (54.5) | |
| Disability of the wrist at 1 year | |||
| Mayo, mean ± SD | 94.0 ± 5.7 | 68.0 ± 15.1 | < 0.001 |
| DASH, mean ± SD | 4.6 ± 2.5 | 28.5 ± 19.5 | < 0.001 |
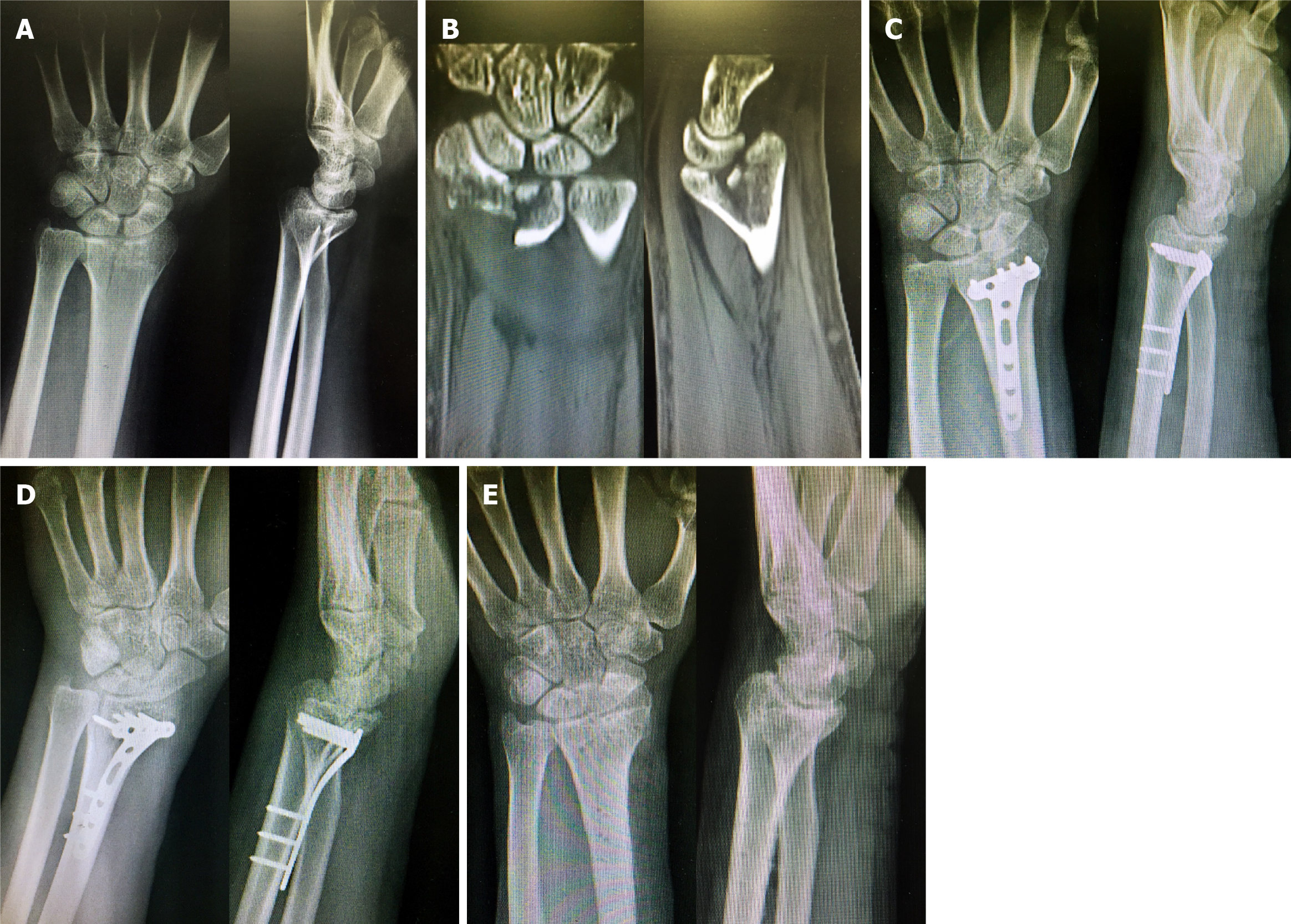
Postoperative evaluation at 1 year showed an average Mayo wrist score of 94 ± 5.7 in the fixed group and 68 ± 15.1 in the unfixed group (P < 0.001) (Table 2). All cases (16/16) in the fixed group had an excellent-good functional outcome. In the unfixed group, six (27.3%) of 22 cases had an excellent-good outcome, and 16 (72.7%) of 22 cases had a fair-poor functional outcome. Among the 16 patients in the fixed group, the DASH score was 4.6 ± 2.5; among the 22 patients in the unfixed group, the DASH score was 28.5 ± 19.5 (P < 0.001) (Table 2 and Figure 3).
Figure 3 presents a representative case. It was a 39-year-old man from the unfixed group, who had a distal radius fracture with VMLF fragment due to a traffic accident.
The purpose of this study was to investigate whether the distal radius fractures with lesions involving the VMLF have an important effect on the postoperative sagittal alignment and stability and function of the wrist joint. The results suggest that injuries to the VMLF, even small fractures, might damage the radial-lunar ligament, leading to postoperative wrist instability, sagittal force line imbalance, and poor recovery of wrist joint function.
This study emphasizes the significance of the reduction of small VMLF fragments when managing distal radius fractures. The VMLF is critical because the SRL is attached to this location. The SRL is important for maintaining the stability of the radiocarpal joint and bears more load than the ligaments attached in the scaphoid fossa. A quantitative three-dimensional CT study has shown that 16% of the lunate facet projects anteriorly from the flat surface of the radius[28]. This bony projection has a mean thickness of 5 mm and width of 19 mm, which is susceptible to fracture but difficult to control with plates and screws alone.
The axes of the radius, lunate, capitate, and 3rd metacarpal should be in a straight line or parallel to each other in the neutral position, which is the normal carpal sagittal alignment[21]. The RLA, CLA, and ERLF are important angles for the carpal sagittal alignment. This alignment is maintained not only by the normal structure of the distal radius and carpal bones but also by the intrinsic and extrinsic carpal ligaments. The movement of the wrist is mainly determined by the radiolunate joint. Stabilization is mainly maintained by the articular capsule and volar and dorsal ligaments[29]. The volar ligaments are tougher than the dorsal ligaments, strengthening the stability of the wrist joint[30]. The SRL originates from the VMLF of the distal radius and attaches to the palmar aspect of the lunate. Distal radius fractures accompanied by VMLF fracture could damage the attachment of the SRL or even injure the SRL directly, which can lead to instability of the wrist joint. In turn, this condition might result in a global radiocarpal volar derangement, even resulting in a volar subluxation of the radiolunate joint. Fractures with SRL partial tears or hematomas, in some cases, can be explored intraoperatively.
In this retrospective study, 19 cases of radiolunate joint instability were found among 22 cases with distal radius fractures accompanied by VMLF fracture in the unfixed group. The possible reason is that the VMLF fracture fragments were not reduced accurately or fixed effectively. Although postoperative X-ray showed that the volar tilt, ulnar tilt, radial height, and articular surface of the distal radius recovered satisfactorily, the small VMLF fragments were not effectively fixed. Three of the 22 patients in the unfixed group did not meet the diagnostic criteria for instability, but all had an ancillary external fixation with plaster for 3 wk after surgery. In contrast, in the fixed group, the VMLF fracture fragments were reduced and effectively fixed with Kirschner wires, ancillary screws, universal plates, or sutures. Four of 16 cases developed instability postoperatively, but none occurred in the radiolunate joint. Therefore, the effective fixation of the VMLF fragments is important to maintain the stability of the wrist joint. This study’s findings suggest that wrist instability and sagittal malalignment associated with outcomes of unfixed VMLF might lead to a worse wrist function than in patients with VMLF fixed effectively. One year after surgery, the Mayo and DASH scores indicate that the patients in the unfixed group had significantly greater disability than those in the fixed group.
This study has several limitations. The data are limited to those available from the patient charts. Data such as osteoporosis, body mass index, drugs, and comorbidities were not available from all patient charts and could not be analyzed. That is one of the shortcomings of retrospective analyses. The age distribution of distal radial fracture is bimodal, peaking in young men and older age women, with more than 50% of fractures belonging to type A3 or C2[31]. The estrogen levels decrease in women after menopause, and the bone loss is faster than in men. The degree of osteoporosis of the distal radius is more serious than in men[32]. Age and gender might be confounding factors for the results, but the number of patients was small, and further follow-up studies are needed. Multivariable analyses for the occurrence of wrist instability could not be performed. Since such cases are relatively rare, surgeons are likely to be less experienced with VMLF fracture fixation, extending the surgical time. Still, additional studies on VMLF repair and fixation are needed.
In patients with distal radius fracture, effective reduction and fixation of the VMLF fragment is important to maintain the stability of the wrist joint and sagittal alignment. Distal radius fractures involving VMLF fragments should be reduced and fixed with Kirschner wires, ancillary screws, universal plates, or sutures, regardless of the articular surface involved. An associated injury of the SRL should be considered when treating distal radius fractures. Examination and repairs should be performed in operative treatment plans for these fractures. If necessary, ancillary external fixation with plaster should be performed after surgery.
Distal radius fractures is common, while volar margin fractures of the lunate fossa (VMLF) is uncommon.
In clinical practice, distal radius fractures accompanied by VMLF lesions are often overlooked or inadequately reduced.
To investigate the effect of fixation of VMLF on the postoperative stability, function, and sagittal alignment of patients with distal fractures of the radius bone accompanied by VMLF lesions.
In the retrospective study, patients with VMLF factures were included and grouped according to whether the VMLF fragments were fixed or not. All patients received operative treatment following the guideline of the German Society for Trauma for distal radius fractures. Affected wrists were evaluated using radiological parameters at preoperative and series postoperative follow-up time points among 6 mo. One year after the operation, the Mayo wrist score and the arm, shoulder, and hand (DASH) score were used to assess wrist disability.
A total of 35 patients were included. There were 38 wrists (17 on the left side, 15 on the right, and three bilateral; 16 in the fixed group, and 22 in the unfixed group). The incidence of postoperative wrist instability in the unfixed group (86.4%) was higher than that in the fixed group (25.0%) (P ≤ 0.001). Both Mayo wrist score and DASH score supported better outcome of wrist instability at 1 year in the fixed group than that of the unfixed group (P ≤ 0.001).
In patients with distal radius fracture, effective reduction and fixation of the VMLF fragment is important to maintain the stability of the wrist joint and sagittal alignment.
An associated injury of the short radiolunate ligament should be considered when treating distal radius fractures.
| 1. | Ruch DS. Fractures of the distal radius and ulna. In: Bucholz RW, Heckman JD, Court-Brown C, editors. Rockwood and Green’s fractures of adults. 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2006. |
| 2. | Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908-915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 538] [Cited by in RCA: 580] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 3. | Chen NC, Jupiter JB. Management of distal radial fractures. J Bone Joint Surg Am. 2007;89:2051-2062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 98] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 4. | Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1916] [Cited by in RCA: 2332] [Article Influence: 116.6] [Reference Citation Analysis (0)] |
| 5. | Handoll HH, Madhok R. Conservative interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2003;CD000314. [PubMed] |
| 6. | Dayican A, Unal VS, Ozkurt B, Portakal S, Nuhoglu E, Tumoz MA. Conservative treatment in intra-articular fractures of the distal radius: a study on the functional and anatomic outcome in elderly patients. Yonsei Med J. 2003;44:836-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Lindau T. Treatment of injuries to the ulnar side of the wrist occurring with distal radial fractures. Hand Clin. 2005;21:417-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 452] [Cited by in RCA: 457] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 9. | Campbell DA. Open reduction and internal fixation of intra articular and unstable fractures of the distal radius using the AO distal radius plate. J Hand Surg Br. 2000;25:528-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 84] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Thomas BP, Sreekanth R. Distal radioulnar joint injuries. Indian J Orthop. 2012;46:493-504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Logan AJ, Lindau TR. The management of distal ulnar fractures in adults: a review of the literature and recommendations for treatment. Strategies Trauma Limb Reconstr. 2008;3:49-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Frane N, Goldenberg W. Perilunate Dislocation. StatPearls. Treasure Island (FL), 2020. |
| 13. | Lee S, Yu JH, Jeon SH. Fixed Lunate Flexion Deformity in Distal Radius Fractures. Clin Orthop Surg. 2016;8:228-231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | O'Shaughnessy MA, Shin AY, Kakar S. Stabilization of Volar Ulnar Rim Fractures of the Distal Radius: Current Techniques and Review of the Literature. J Wrist Surg. 2016;5:113-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Zhang J, Ji XR, Peng Y, Li JT, Zhang LH, Tang PF. New classification of lunate fossa fractures of the distal radius. J Orthop Surg Res. 2016;11:124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Obata H, Baba T, Futamura K, Obayashi O, Mogami A, Tsuji H, Kurata Y, Kaneko K. Difficulty in Fixation of the Volar Lunate Facet Fragment in Distal Radius Fracture. Case Rep Orthop. 2017;2017:6269081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Harness NG. Fixation Options for the Volar Lunate Facet Fracture: Thinking Outside the Box. J Wrist Surg. 2016;5:9-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Harness NG, Jupiter JB, Orbay JL, Raskin KB, Fernandez DL. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg Am. 2004;86:1900-1908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 159] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 19. | Lill CA, Goldhahn J, Albrecht A, Eckstein F, Gatzka C, Schneider E. Impact of bone density on distal radius fracture patterns and comparison between five different fracture classifications. J Orthop Trauma. 2003;17:271-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Polytrauma Guideline Update Group. Level 3 guideline on the treatment of patients with severe/multiple injuries: AWMF Register-Nr. 012/019. Eur J Trauma Emerg Surg. 2018;44:3-271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 21. | Garcia-Elias M. Carpal Instability. In: Wolfe SW, Hotchkiss RN, Pederson WC, editors. Green’s operative hand surgery. 6th ed. Philadelphia: Elsevier/Churchill Livingstone, 2011. |
| 22. | Gupta A, Batra S, Jain P, Sharma SK. Carpal alignment in distal radial fractures. BMC Musculoskelet Disord. 2002;3:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Berger RA. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res. 2001;32-40. [PubMed] |
| 24. | Taleisnik J, Watson HK. Midcarpal instability caused by malunited fractures of the distal radius. J Hand Surg Am. 1984;9:350-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 192] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 25. | Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 634] [Cited by in RCA: 766] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 26. | Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand. 2000;71:613-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 292] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 27. | Egund L, Önnby K, Mcguigan F, Åkesson K. Disability and Pain are the Best Predictors of Sick Leave After a Distal Radius Fracture in Men. J Occup Rehabil. 2020;30:656-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Andermahr J, Lozano-Calderon S, Trafton T, Crisco JJ, Ring D. The volar extension of the lunate facet of the distal radius: a quantitative anatomic study. J Hand Surg Am. 2006;31:892-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Brahin B, Allieu Y. [Compensatory carpal malalignments]. Ann Chir Main. 1984;3:357-363. [PubMed] |
| 30. | Dzwierzynski WW, Matloub HS, Yan JG, Deng S, Sanger JR, Yousif NJ. Anatomy of the intermetacarpal ligaments of the carpometacarpal joints of the fingers. J Hand Surg Am. 1997;22:931-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Ng CY, McQueen MM. What are the radiological predictors of functional outcome following fractures of the distal radius? J Bone Joint Surg Br. 2011;93:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 105] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 32. | Mackenney PJ, McQueen MM, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88:1944-1951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 138] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Welter J S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Wang LYT