Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7032
Peer-review started: March 26, 2021
First decision: May 5, 2021
Revised: June 11, 2021
Accepted: July 5, 2021
Article in press: July 5, 2021
Published online: August 26, 2021
Processing time: 150 Days and 23 Hours
Coronavirus disease 2019 (COVID-19) is a serious infection caused by the new coronavirus severe acute respiratory syndrome coronavirus 2. The disease was first identified in December 2019 and has caused significant morbidity and mortality worldwide.
To explore the clinical characteristics and treatments for COVID-19 in the Qinghai-Tibetan Plateau Area in China.
We retrospectively analyzed the blood cell counts (neutrophils and lymphocytes), blood gas analysis, and thoracic computed tomography changes of patients from Qinghai Province before, during, and after treatment (January 23, 2020 to February 21, 2020). In addition, we summarized and analyzed the information of critical patients. All data were analyzed using SPSS 17.0 (SPSS Inc., Chicago, IL, United States). The quantitative and count variables are represented as the mean ± SD and n (%), respectively.
The main symptoms and signs of patients with COVID-19 were fever, dry cough, cough with phlegm, difficulty breathing, and respiratory distress with a respiration rate ≥ 30 times/min, finger oxygen saturation ≤ 93% in the resting state, and oxygenation index less than 200 but greater than 100 (after altitude correction). Eighteen patients with COVID-19, of whom three were critical, and the others were in a mild condition, were included. The main manifestations included fever, dry cough, and fatigue. Three patients developed difficulty breathing and had a fever. They were eventually cured and discharged. Adjuvant examinations showed one case with reduced white cell count (6%) (< 4 × 109/L), six with reduced count of lymphocytes (33%) (< 0.8 × 109/L), and one with abnormal blood glucose level. All 18 patients were discharged, and no death occurred.
Our findings provide critical insight into assessing the clinical diagnosis and treatment for COVID-19 in the Tibetan plateau area.
Core Tip: Eighteen patients with coronavirus disease 2019, of whom three were critical and the rest were in a mild condition were enrolled. The main manifestations included fever, dry cough, and fatigue. Three patients developed difficulty in breathing and had a fever and were eventually cured and discharged.
- Citation: Li JJ, Zhang HQ, Li PJ, Xin ZL, Xi AQ, Zhuo-Ma, Ding YH, Yang ZP, Ma SQ. Case series of COVID-19 patients from the Qinghai-Tibetan Plateau Area in China. World J Clin Cases 2021; 9(24): 7032-7042
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7032.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7032
The novel coronavirus (severe acute respiratory syndrome coronavirus 2, SARS-CoV-2) is an enveloped, non-segmented, positive-sense single-stranded RNA virus, causing a severe human and livestock coronavirus disease[1]. Since December 2019, the coronavirus disease 2019 (COVID-19) has swept the entire country of China. Clinical findings showed exuberant inflammatory responses, likely a leading cause of case fatality during SARS-CoV-2 infection, followed by other symptoms such as acute respiratory distress syndrome (ARDS) and immune dysfunction[2-4].
According to the statistics released by Johns Hopkins University on May 30, 2020, the number of confirmed cases in the world has reached 6003762, with 367356 deaths. Data shows that the United States is the country with the most serious epidemic, with 1764671 confirmed cases and 103605 deaths. Countries with more than 200000 confirmed cases are Brazil, Russia, the United Kingdom, Spain, and Italy. In addition, France, Germany, India, and Turkey have more than 150000 cumulative confirmed cases. Common symptoms include fever, fatigue, and dry cough and computed tomography (CT) shows that the lungs of most patients have a bilateral patchy shadow or ground-glass opacity[5-8]. Most patients receive anti-virus treatment (oseltamivir), many patients receive antibacterial treatment (moxifloxacin, ceftriaxone, and azithromycin), and glucocorticoid therapy[9]. Real-time reverse transcription-polymerase chain reaction (RT-PCR) is used for nucleic acid detection of the novel coronavirus[6,10]. It is suggested that the combination of repeated swab tests and CT scanning is helpful for the clinical diagnosis of COVID-19 when it is highly suspected of SARS-CoV-2 infection, but RT-PCR screening is negative[9,10]. The mechanisms of COVID-19 remain elusive, although respiratory virus-induced lung injuries are considered to be involved[11]. Toll-like receptors (TLRs) such as TLR3 and TLR9 are activated by viral RNA, leading to the activation of mesenchymal stem cells (MSCs) that are associated with lung injuries[12]. MSCs can induce innate antiviral defenses and provide therapeutic benefits in COVID-19 patients. Studies showed that SARS-CoV-2 exploits the angiotensin-converting enzyme 2 (ACE2) receptor to enter the cells, which causes neurological tissue damage[13]. By now, scientists have proposed a hypothesis for the pathobiology and treatment of COVID-19. ACE2 is the receptor of coronavirus SARS-CoV-2, and reducing ACE1/ACE2 imbalance may blunt the morbidity and mortality of COVID-19[14]. The good news is that ANG II receptor blockers and ACE1 inhibitors can be rapidly tested in patients with COVID-19. The prognosis of most patients is good. Only individuals with poor immune function, such as the elderly, pregnant women, or those with serious basic diseases such as diabetes, coronary heart disease, and liver and kidney dysfunction, have a relatively rapid progression and higher severity. Some of these patients may become critically ill or even die[15,16].
Although the mechanisms and treatments for COVID-19 have been explored, there is no report of the treatments and clinical characteristics of COVID-19 patients in the Tibetan plateau area. The plateau is geographically defined as an extensive, flat land area with an altitude above 500 m and gentle slopes in the terrain. It is confirmed that an altitude above 3000 m can induce a significant biological effect in people living in the plateau area, which has been the study focus for high altitude medical research[17,18]. This manuscript reports case series of COVID-19 patients from the Qinghai-Tibetan Plateau Area in China, which will improve the understanding of COVID-19.
This was a retrospective case series of patients confirmed with COVID-19 at Qinghai fourth People’s Hospital and Xining Third People’s Hospital, which were designated hospitals for COVID-19 in Qinghai Province. The diagnostic criteria were based on pathogenic or serological evidence: (1) Positive real-time PCR test for SARS-CoV-2; (2) Viral whole-genome sequencing showing high homogeneity to SARS-CoV-2; and (3) Positivity for the specific immunoglobulin M antibody and immunoglobulin G (IgG) antibody in the serum SARS-CoV-2 test, a change of the SARS-CoV-2-specific IgG antibody from negative to positive, or titer rising ≥ 4 times in the recovery phase above that in the acute phase.
The clinical research protocol was approved by the Institutional Review Board and the Ethical Committee of the Qinghai fourth People’s Hospital and Institute (No. 20200401), which were in accordance with the ethical standards of our Institutional Review Board and with the 1975 Helsinki declaration (revised in 2010) and its later amendments or comparable ethical standards.
The patients were treated in compliance with the fifth edition of the treatment and diagnosis plan for COVID-19 published by the National Health Commission, as summarized below.
General treatment: Rest in bed in the isolation area with sufficient energy supply was suggested. Enhanced supportive care was given to maintain the homeostasis of water and electrolyte. (1) Oxygen was given in a timely manner to keep the airway moist. Once admitted, the patients were given oxygen at 2-5 L/min intranasally or through a face mask to ensure that the figure oxygen saturation was around 95%. And (2) Antiviral medication: Atomization inhalation of α-2b interferon (Bioway Biomedical Co. Ltd, Tianjin) was provided at a dose of 5 million units per time for adults, three times per day. Lopinavir/ritonavir (Kaletra; 200 mg/50 mg per tablet; approval No. H20170213; manufactured by AbbVie Deutschland GmbH & Co.KG, Germany) was given two tablets each time, twice a day. Children were given three tablets per day in total, twice a day. Moxifloxacin (0.4 g; Bayer Pharmaceuticals) was given orally or intravenously once a day. The Chinese medicine Xue Bi Jing (Chase Sun Pharmaceutical Co. Ltd, Tianjin) for injection was given intravenously at 50-100 mL once a day. The Chinese medicine Tan Re Qing (Kai Bao Pharmaceutical Co. Ltd, Shanghai) for injection was given intravenously at 10-30 mL once a day. Ribavirin (Ya Tai Pharmaceutical Co. Ltd, Zhejiang Province) was given intravenously at a dose of 500 mg per time, three times a day for adults. Vitamin C (2 g; Hasen Modern Pharmaceutical Co. Ltd, Shanghai) was given intravenously once a day. Oseltamivir 75 mg (Yichang HEC Changjiang Pharmaceutical Co., Ltd, Hubei Province) capsules were given orally twice a day. Thymalfasin (1.6 mg; ShuangCheng Pharmaceutical Co., Ltd, Hainan Province) was given by subcutaneous injection twice per week.
Treatments for patients in critical condition: (1) Oxygen inhalation: The patients were provided with a non-invasive ventilator (Phillips V60) to facilitate respiration, with the following parameters: Inspiratory pressure 10-12 cmH2O, PEEP 4-8 cmH2O, FiO2 35%-45%, and SpO2 95%. Prone position ventilation was initially used. The V60 non-invasive ventilators from Philips were used, with 4-6 cm H2O pressure in the CPAP mode; (2) Steroid treatment: Methylprednisolone sodium succinate for injection (40-80 mg) (Haisco Pharmaceutical Co. Ltd, Liaoning Province) was given twice a day intravenously. The human immunoglobulin for injection (25 g) (Hualan Biological Engineering Inc., Shanghai) was given intravenously once a day for three successive days; (3) Fluid therapy: The daily fluid intake was kept below 800 mL to maintain a negative fluid balance; and (4) Plasma therapy: The three critical patients were given the plasma from cured patients intravenously twice, 50 mL each time.
Chinese medicine treatment: (1) Therapy 1: Astragalus 15 g, dried white Atractylodes rhizome 10 g, Saposhnikovia divaricata 10 g, Radix isatidis 15 g, honeysuckle 10 g, dried tangerine peel 8 g.m. and Eupatorium 10 g, one pack a day and decocted twice in water; (2) Therapy 2: Rhizoma Pinellinae Praeparata 9 g, dried tangerine peel 10 g, Codonopsis pilosula 15 g, Astragalus 30 g, Tuckahoe 15 g, Agastache rugosus 15 g, Fructusamomi 6 g, Cordatehouttuynia 30 g, Forsythia 20 g, Paeoniae Radix 15 g, Oyster 30 g, Fructus Aurantii 20 g, and Radix Isatidis 20 g, one pack a day and decocted twice in water. This therapy would help invigorate the circulation, reduce the disease-causing risks, and detoxify the body for recovery; and (3) Therapy 3: Rhizoma Pinellinae Praeparata 9 g, dried tangerine peel 10 g, Codonopsispilosula 15 g, Astragalus membranaceus 30 g, smilax glabra rhizome 15 g, Pogostemoncablin 15 g, Fructusamomi 6 g, Cordatehouttuynia 30 g, Forsythia 20 g, Fried Forsythia 20 g, Eupatorium 20 g, dried ginger 10 g, Paeoniae Radix 15 g, and Oyster 30 g.
Criteria for discharge: The patient’s body temperature had to remain normal for at least 3 d. The respiratory symptoms greatly improved. The patient tested negative for pathogenic nucleic acids in two successive tests (at least 24 h apart). If all criteria were met, the patient could be discharged or transferred to the corresponding department to treat other diseases.
Complete blood tests were performed before and after treatment, including blood cell count (including neutrophils and lymphocytes) and blood gas analysis. The equipment involved an Automated Erythrocyte Sedimentation Rate Analyzer (Monitor-100, Vital Diagnosis, Italy), Zybio-Q7 for determination of procalcitonin/C-reactive protein (ZybioInc, Chongqing), the blood gas analyzer ABL90 (Radiometer, Denmark), and Biochemical analyzer TBA-FX8 (TOSHIBA, Japan). Blood samples were drawn into ethylenediaminetetraacetic acid tubes and mixed well at venipuncture and again just before analysis. All measurements were commenced within 4 h after blood collection.
All data were analyzed using SPSS 17.0 (SPSS Inc., Chicago, IL, United States). The continuous and categorical variables are presented as the mean ± SD and n (%). Comparisons between two groups were examined using the two-sample t-test, and comparisons among multiple groups were examined using the F-test. The between-group comparisons of categorical variables were performed by Chi-square test. P < 0.05 was considered statistically significant.
Since the admission of the first confirmed case in Qinghai Province on January 23, 2020, 18 patients were confirmed with COVID-19, of whom three were in a critical condition, and the others were in a mild condition. Altogether 15 patients were admitted to Qinghai Fourth People’s Hospital, including the three in a critical condition, and three patients in mild condition were admitted to Xining Third People’s Hospital. All 18 patients were discharged. No death occurred. The main manifestations included fever, dry cough, and fatigue. Three patients developed difficulty breathing.
Regarding main symptoms and signs, 10 patients had a fever, 12 had a dry cough, five had cough with phlegm, three had difficulty breathing, three had respiratory distress with a respiration rate ≥ 30 times/min, three had finger oxygen saturation ≤ 93% in the resting state, and three had an oxygenation index less than 200 but greater than 100 (after altitude correction). Three (17%) out of the 18 patients developed difficulty breathing within an average of 11 d after disease onset, with oxygen saturation ≤ 93% and altitude-corrected oxygenation index less than 200 but greater than 100. These three cases were initially in a mild condition and were given intranasal oxygen inhalation and gradually progressed into critical or severe conditions.
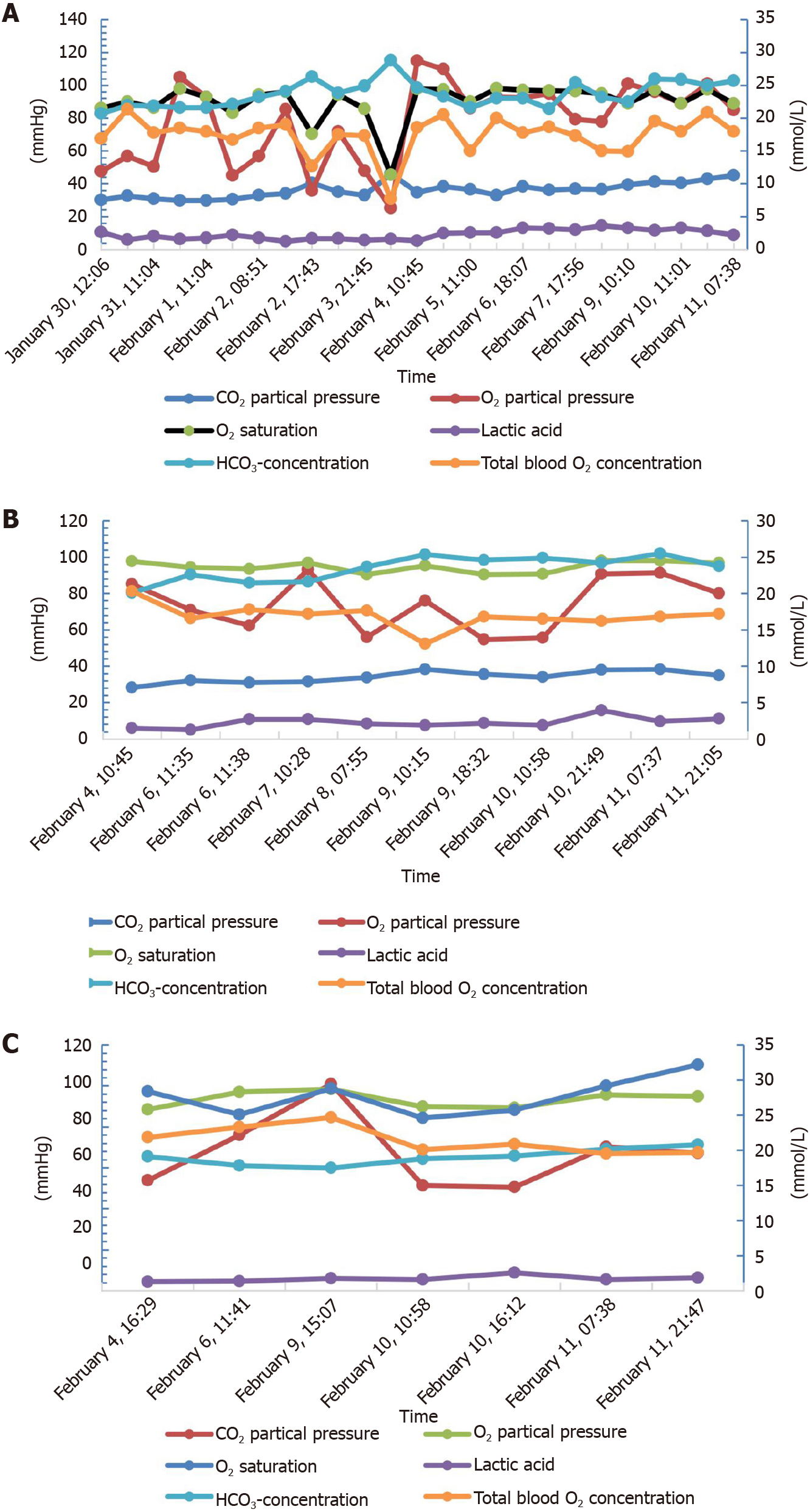
Adjuvant examinations showed one patient with a reduced white cell count (6%) (< 4 × 109/L), six with reduced counts of lymphocytes (33%) (< 0.8 × 109/L), and one with an abnormal blood glucose level (Figure 1).
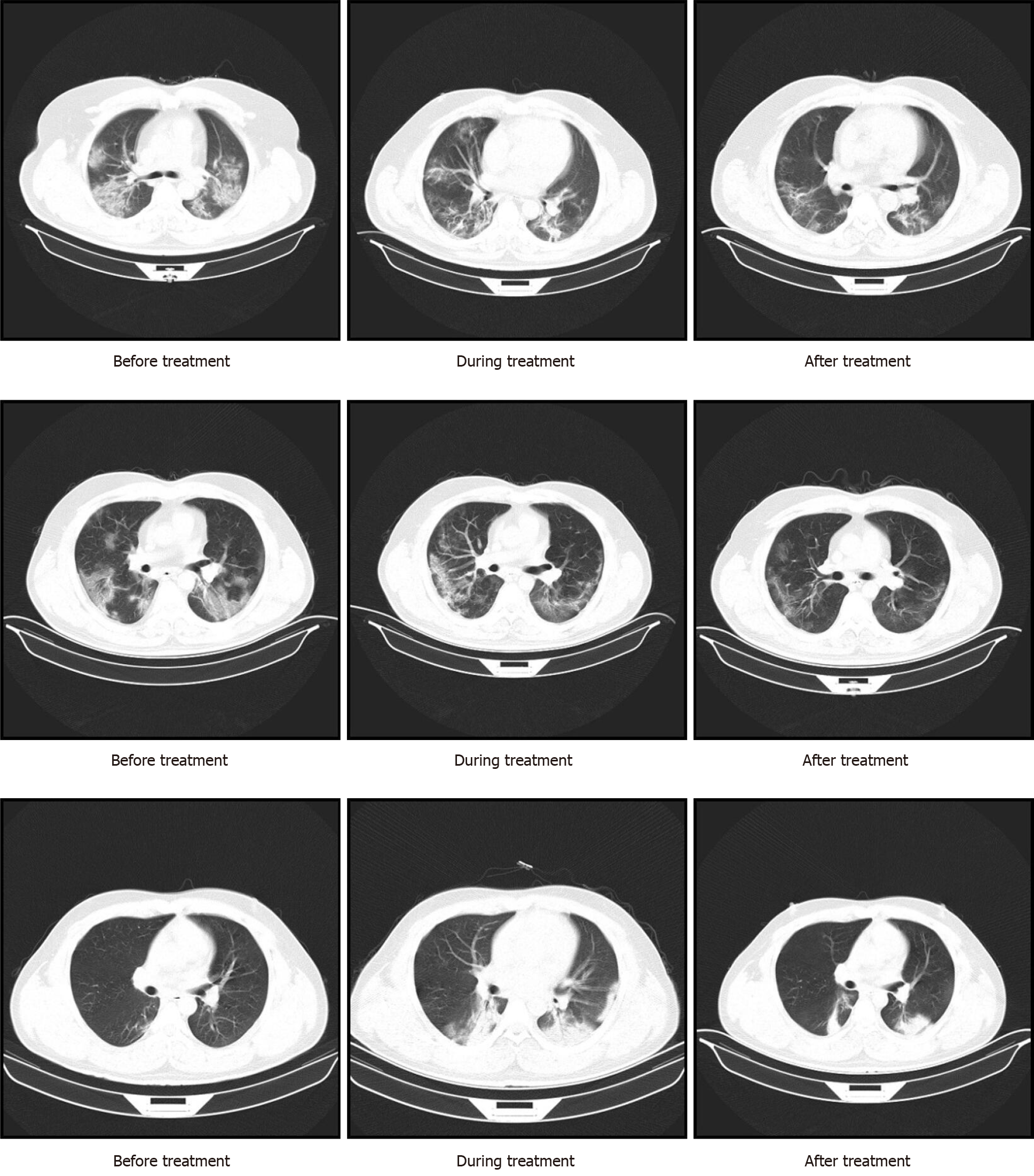
Thoracic CT revealed 13 cases with bilateral pneumonia, one with pneumonia in the left lung, three with pneumonia in the right lung, and one with no obvious pulmonary lesion.
A nasopharyngeal swab was collected when the patients did not have a fever or clinical symptoms for 3 d. A recheck was performed 24 h after the initial test. Sixteen cases turned out negative in the initial test, and two remained positive.
Sixteen out of the 18 cases were imported cases with a history of going to Wuhan for work, school, or family visits. Of all the imported cases, the first confirmed case in Qinghai worked for a company and developed symptoms 3 d after returning to Xining from Wuhan, and initially had a fever with a body temperature of 37.1 °C. On January 25, he was confirmed infected. A patient and his son lived in Wuhan and worked in the catering industry for a long time. They returned from Wuhan on January 16, 2020, and developed symptoms including cough, fever, and fatigue on that night. They attended a few events and were in contact with more than 300 people before their nasopharyngeal swab samples were tested positive in Qinghai Provincial Center for Disease Control and Prevention on January 28. Among those contact people, some cases were confirmed with COVID-19. Three were family cases, and five shared the same transportation. One of the two secondary infection cases was in close contact with a confirmed case, and the other case developed symptoms after being in contact with people returning from Wuhan. Among the 18 cases, 15 were from agricultural and pastoral areas (83%), and three were from urban areas (17%), including 12 males (67%) and six females (33%). The age ranged from 7 to 47 years old, with an average of 30.5 years old. Five cases were found to have underlying diseases: One with polymyositis (6%), two with hypertension (11%), two with tuberculosis (11%), and one with chronic hepatitis B (6%).
The white blood cell count after treatment was not statistically meaningful because of the steroid treatment. The lymphocyte counts returned to normal after treatment.
Patient 1: In a critical condition, was a 44-year-old man who used to work in the catering industry in Wuhan and was born in Qinghai province. He had hypertension. He had a fever with the highest body temperature of 39.5 °C when he returned from Wuhan and was eventually cured and discharged.
Patient 2: In a critical condition, was a 43-year-old man who was born and worked in Qinghai province. He had hypertension. He was the younger brother of patient 1 and was in close contact with him. He had a fever with the highest body temperature of 38.7 °C and was eventually cured and discharged.
Patient 3: In a critical condition, was a 26-year-old man who used to work in the catering industry in Wuhan and was born in Qinghai province. He had no underlying conditions. He had a fever with the highest body temperature of 37.8 °C when he came back from Wuhan and was eventually cured and discharged.
The dynamic blood gas analysis (Figure 1) and imaging manifestations of the critical patients before and after treatment (Figure 2) are shown.
Since December 2019, COVID-19 has spread widely across China and all over the world. The virus is highly contagious and can target multiple organs. Therefore, it is very difficult to treat the disease. The doctors in the isolation ward try their best to save the patients and fight the virus[19,20]. There has been no report of the treatments and clinical characteristics for COVID-19 patients in the Tibetan plateau area. We report a series of COVID-19 patients from the Qinghai-Tibetan Plateau Area in China, which will improve the understanding of COVID-19. Since the admission of the first confirmed case in Qinghai on January 23, 2020, there were 18 confirmed cases in total, of whom three were in critical condition. As of February 21, 2020, all patients were cured and discharged. No death was reported. There were only two secondary infection cases in Qinghai province, which could be due to its location in the east of the Qinghai-Tibet Plateau with high altitude, low atmospheric oxygen content, and high ultraviolet (UV) exposure.
In this study, we found that the most common symptoms of COVID-19 were fever, dry cough, and fatigue, consistent with the COVID-19 diagnostic criteria published by the National Health Commission of China[21-23]. Of all 18 COVID-19 patients in the plateau area, no death was reported. The fatality of patients in the plateau area is significantly lower than the whole national average level, which might be associated with characteristics of the plateau area[24]. The plateau area is a low-pressure environment. At the altitude of 5500 m, both atmospheric pressure and oxygen partial pressure are decreased by 50% compared with those at the sea level, resulting in decreased oxygen partial pressure of pulmonary gas exchange and arterial oxygen saturation[25-27]. In addition, for every 100 m increase in altitude, the temperature drops by about 0.6 °C. The cold makes the oxygen consumption and oxygen demand and the body load increase, and promotes the occurrence and development of tissue hypoxia[28-30]. The humidity at an altitude of 3000 m is only 34% of that in the plain; at an altitude of 6000 m, it is only 5% of that in the plain. Hence, water loss from the body surface and respiratory tract in plateau area is higher than that in the plain area, especially during exercise. At the same time, due to the influence of diuretic factors such as hypoxia and cold, the water content of the body is reduced, resulting in the abnormal dryness of the respiratory mucosa and the whole-body skin, and symptoms such as pharyngitis, dry cough, epistaxis, and dry split skin are easy to occur.
The plateau area has strong radiation and strong ultraviolet, more than 2.5 times that in the plain. When the incident and reflection rays are superposed, the amount and intensity of the ultraviolet light received by the human body increase significantly, causing damage to the skin and eyes[31,32] but possibly contributing to a low viral transmission. Therefore, the only two secondary infection cases could be due to high altitude, low atmospheric oxygen content, and high UV exposure. Indeed, ultraviolet light can be used to decontaminate protective equipment such as single-use filtering face respirators[33,34]. A previous study suggested that the maximal COVID-19 death rates were observed in areas with a maximal temperature of 10.1 °C, maximal humidity of 55%, and a null UV index[35]. Although the temperature is cold in the plateau, humidity is far lower than 55%, and the UV index is elevated. The characteristics of patients in critical condition include mild disease onset but sudden exacerbation in about 2 wk. The high fever was significantly correlated with respiratory difficulty. Hypoxia caused by COVID-19 has a smaller effect on the patients’ heart rate and respiratory rate than that caused by other ARDS, contrary to our expectations[36]. It can be proposed that it is critical to provide oxygen treatment in advance as the hypoxia in the patients with COVID-19 is silent and deceptive.
SARS-CoV-2 has a potential impact on the heart, especially in patients with cardiovascular diseases, and the potential complications and death risk increase. Reasonable preventive measures are recommended. In the COVID-19 diagnosis and treatment guidelines, the following definitions have been made for the patients with severe and critical respiratory infection: Severe cases have respiratory distress, hypoxemia, or shock, and require oxygen therapy, while critical cases require respiratory support and have hypoxic respiratory failure, ARDS, and septic shock. Severe and critical patients often have respiratory difficulties caused by the infection, which is the main clinical manifestation of myocardial injury[37]. While atmospheric pressure and oxygen partial pressure are decreased by 50% in the plateau area, more attention must be paid to hypoxemia.
There are some limitations to this study. The sample size was small, with only 18 patients included. The age of patients ranged between 7-47 years old, with an average of 30.5 years old, and there were no neonatal or elderly patients. Because of the epidemic, no further study of the similarities and differences of the mechanisms was performed. Last, because of the retrospective design of the study, some data might be missing.
In this study, we collectively illuminate the epidemiological characteristics and treatments for COVID-19 patients from the Qinghai-Tibetan Plateau Area in China. Our findings provide critical insight into assessing the clinical diagnosis and treatment of COVID-19 in the plateau area, which will further improve the understanding of COVID-19.
Coronavirus disease 2019 (COVID-19) is a serious infection caused by the new coronavirus severe acute respiratory syndrome coronavirus 2. The disease was identified in December 2019 and has caused significant morbidity and mortality worldwide.
Although the mechanisms and treatments for COVID-19 have been explored, there is no report of the treatments and clinical characteristics for COVID-19 patients in the Tibetan plateau area, which features a low temperature, low humidity, and high ultraviolet exposure.
To explore the clinical characteristics and treatments for COVID-19 in the Qinghai-Tibetan Plateau Area in China.
This study retrospectively analyzed the blood cell counts (neutrophils and lymphocytes), blood gas analysis, and thoracic computed tomography changes of patients from Qinghai Province before, during, and after treatment (January 23, 2020 to February 21, 2020). In addition, we summarized and analyzed the information of critical patients.
This study included 18 patients with COVID-19 in the Qinghai-Tibetan Plateau Area. The main manifestations included fever, dry cough, and fatigue. Three patients developed difficulty breathing and had a fever. They were eventually cured and discharged. Of the 18 cases, only two had secondary infections and three developed a critical condition but were cured and discharged. All 18 patients were discharged, and no death occurred.
This study collectively illuminates the epidemiological characteristics and treatments for COVID-19 patients from the Qinghai-Tibetan Plateau Area in China.
Our findings provide critical insight into assessing the clinical diagnosis and treatment of COVID-19 in the plateau area, which will further improve the understanding of COVID-19.
| 1. | Chen Y, Liu Q, Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol. 2020;92:418-423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1873] [Cited by in RCA: 1905] [Article Influence: 317.5] [Reference Citation Analysis (1)] |
| 2. | Li D, Chen Y, Liu H, Jia Y, Li F, Wang W, Wu J, Wan Z, Cao Y, Zeng R. Immune dysfunction leads to mortality and organ injury in patients with COVID-19 in China: insights from ERS-COVID-19 study. Signal Transduct Target Ther. 2020;5:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 3. | Molloy EJ, Bearer CF. COVID-19 in children and altered inflammatory responses. Pediatr Res. 2020;88:340-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 4. | Vittori A, Lerman J, Cascella M, Gomez-Morad AD, Marchetti G, Marinangeli F, Picardo SG. COVID-19 pandemic acute respiratory distress syndrome survivors: pain after the storm? Anesth Analg. 2020;131:117-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 13058] [Article Influence: 2176.3] [Reference Citation Analysis (4)] |
| 6. | Epidemiology Working Group for NCIP Emergency Response; Chinese Center for Disease Control and Prevention. Rapid investigation plan of clinical courses and key diagnosis and treatment equipment requirements for the patients of the 2019 Novel Coronavirus Pneumonia (COVID-19). Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | DU HZ, Hou XY, Miao YH, Huang BS, Liu DH. Traditional Chinese Medicine: an effective treatment for 2019 novel coronavirus pneumonia (NCP). Chin J Nat Med. 2020;18:206-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 8. | Wang Z, Chen X, Lu Y, Chen F, Zhang W. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci Trends. 2020;14:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 335] [Article Influence: 55.8] [Reference Citation Analysis (0)] |
| 9. | Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, Fang C, Huang D, Huang LQ, Huang Q, Han Y, Hu B, Hu F, Li BH, Li YR, Liang K, Lin LK, Luo LS, Ma J, Ma LL, Peng ZY, Pan YB, Pan ZY, Ren XQ, Sun HM, Wang Y, Wang YY, Weng H, Wei CJ, Wu DF, Xia J, Xiong Y, Xu HB, Yao XM, Yuan YF, Ye TS, Zhang XC, Zhang YW, Zhang YG, Zhang HM, Zhao Y, Zhao MJ, Zi H, Zeng XT, Wang XH; for the Zhongnan Hospital of Wuhan University Novel Coronavirus Management and Research Team, Evidence-Based Medicine Chapter of China International Exchange and Promotive Association for Medical and Health Care (CPAM). A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res. 2020;7:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 881] [Cited by in RCA: 1141] [Article Influence: 190.2] [Reference Citation Analysis (1)] |
| 10. | Zhang J, Wang S, Xue Y. Fecal specimen diagnosis 2019 novel coronavirus-infected pneumonia. J Med Virol. 2020;92:680-682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 278] [Cited by in RCA: 301] [Article Influence: 50.2] [Reference Citation Analysis (0)] |
| 11. | Khoury M, Cuenca J, Cruz FF, Figueroa FE, Rocco PRM, Weiss DJ. Current status of cell-based therapies for respiratory virus infections: applicability to COVID-19. Eur Respir J. 2020;55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 183] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 12. | Waterman RS, Tomchuck SL, Henkle SL, Betancourt AM. A new mesenchymal stem cell (MSC) paradigm: polarization into a pro-inflammatory MSC1 or an Immunosuppressive MSC2 phenotype. PLoS One. 2010;5:e10088. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 798] [Cited by in RCA: 973] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 13. | Baig AM, Khaleeq A, Ali U, Syeda H. Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. ACS Chem Neurosci. 2020;11:995-998. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1435] [Cited by in RCA: 1423] [Article Influence: 237.2] [Reference Citation Analysis (0)] |
| 14. | South AM, Brady TM, Flynn JT. ACE2 (Angiotensin-Converting Enzyme 2), COVID-19, and ACE Inhibitor and Ang II (Angiotensin II) Receptor Blocker Use During the Pandemic: The Pediatric Perspective. Hypertension. 2020;76:16-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 15. | Trifirò G, Crisafulli S, Andò G, Racagni G, Drago F; Italian Society of Pharmacology. Should Patients Receiving ACE Inhibitors or Angiotensin Receptor Blockers be Switched to Other Antihypertensive Drugs to Prevent or Improve Prognosis of Novel Coronavirus Disease 2019 (COVID-19)? Drug Saf. 2020;43:507-509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Lee KS. Pneumonia Associated with 2019 Novel Coronavirus: Can Computed Tomographic Findings Help Predict the Prognosis of the Disease? Korean J Radiol. 2020;21:257-258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 17. | PLOS ONE Staff. Correction: fractal feature of particle-size distribution in the rhizospheres and bulk soils during natural recovery on the loess plateau, China. PLoS One. 2015;10:e0140305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Song Z, Zhang C, Liu G, Qu D, Xue S. Fractal feature of particle-size distribution in the rhizospheres and bulk soils during natural recovery on the loess plateau, China. PLoS One. 2015;10:e0138057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Giulio M, Maggioni D, Montroni I, Ugolini G, Capelli P, Ceppi L, Bonfanti P, Mariani A, Achilli F. Being a doctor will never be the same after the COVID-19 pandemic. Am J Med. 2020;133:652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Santini D, Tonini G. Brief letter of a doctor to his psychologist in the COVID-19 outbreak era. ESMO Open. 2020;5:e000801. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Cao H, Ruan L, Liu J, Liao W. The clinical characteristic of eight patients of COVID-19 with positive RT-PCR test after discharge. J Med Virol. 2020;92:2159-2164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 22. | He J, Wu B, Chen Y, Tang J, Liu Q, Zhou S, Chen C, Qin Q, Huang K, Lv J, Peng D. Characteristic Electrocardiographic Manifestations in Patients With COVID-19. Can J Cardiol. 2020;36:966.e1-966.e4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 23. | Wang H, Wei R, Rao G, Zhu J, Song B. Characteristic CT findings distinguishing 2019 novel coronavirus disease (COVID-19) from influenza pneumonia. Eur Radiol. 2020;30:4910-4917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 24. | Lv B, Li Z, Chen Y, Long C, Fu X. Global COVID-19 fatality analysis reveals Hubei-like countries potentially with severe outbreaks. J Infect. 2020;81:e87-e88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Sun L, Ding MJ, Cai TC, Fan HJ, Gao HM, Zhang JP. Using a new plateau hyperbaric chamber to alleviate high altitude hypoxia: Rabbit and human studies. Am J Emerg Med. 2017;35:1536-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Wei D, Wei L, Li X, Wang Y. Effect of Hypoxia on Ldh-c Expression in Somatic Cells of Plateau Pika. Int J Environ Res Public Health. 2016;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Li YX, Liu FY, Hu L, Liu SM, Wu TY. [Comparative study of high altitude chronic hypoxia on renal function in yak and migrated cattle on Qinghai-Tibetan plateau]. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 2016;32:440-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 28. | Wu H, Gu Q, Xie Y, Lou Z, Xue P, Fang L, Yu C, Jia D, Huang G, Zhu B, Schneider A, Blom J, Lasch P, Borriss R, Gao X. Cold-adapted Bacilli isolated from the Qinghai-Tibetan Plateau are able to promote plant growth in extreme environments. Environ Microbiol. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 29. | Ding Z, Li L, Wei R, Dong W, Guo P, Yang S, Liu J, Zhang Q. Association of cold temperature and mortality and effect modification in the subtropical plateau monsoon climate of Yuxi, China. Environ Res. 2016;150:431-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Bing H, Wu Y, Zhou J, Li R, Luo J, Yu D. Vegetation and Cold Trapping Modulating Elevation-dependent Distribution of Trace Metals in Soils of a High Mountain in Eastern Tibetan Plateau. Sci Rep. 2016;6:24081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 31. | Norsang G, Chen YC, Pingcuo N, Dahlback A, Frette Ø, Kjeldstad B, Hamre B, Stamnes K, Stamnes JJ. Comparison of ground-based measurements of solar UV radiation at four sites on the Tibetan Plateau. Appl Opt. 2014;53:736-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Ademola JA. Exposure to high background radiation level in the tin mining area of Jos Plateau, Nigeria. J Radiol Prot. 2008;28:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 33. | Polkinghorne A, Branley J. Evidence for decontamination of single-use filtering facepiece respirators. J Hosp Infect. 2020;105:663-669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 34. | Rathnasinghe R, Karlicek RF, Schotsaert M, Koffas MA, Arduini B, Jangra S, Wang B, Davis JL, Alnaggar M, Costa A, Vincent R, Garcia-Sastre A, Vashishth D, Balchandani P. Scalable, effective, and rapid decontamination of SARS-CoV-2 contaminated N95 respirators using germicidal ultra-violet C (UVC) irradiation device. medRxiv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | De Larochelambert Q, Marc A, Antero J, Le Bourg E, Toussaint JF. Covid-19 Mortality: A Matter of Vulnerability Among Nations Facing Limited Margins of Adaptation. Front Public Health. 2020;8:604339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 36. | Earhart AP, Holliday ZM, Hofmann HV, Schrum AG. Consideration of dornase alfa for the treatment of severe COVID-19 acute respiratory distress syndrome. New Microbes New Infect. 2020;35:100689. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 37. | Colla J, Rodos A, Seyller H, Weingart S. Fighting COVID-19 Hypoxia With One Hand Tied Behind Our Back: Blanket Prohibition of High-Flow Oxygen and Noninvasive Positive End-Expiratory Pressure in US Hospitals. Ann Emerg Med. 2020;75:791-792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Respiratory system
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Arabey AA S-Editor: Wu YXJ L-Editor: Wang TQ P-Editor: Liu JH