Published online Nov 16, 2025. doi: 10.12998/wjcc.v13.i32.109464
Revised: June 15, 2025
Accepted: October 24, 2025
Published online: November 16, 2025
Processing time: 184 Days and 7.9 Hours
Rotator cuff tears are a chief cause of shoulder pain and disability, and surgical repair is often required when conservative management fails. As digital health technologies have expanded, especially since the coronavirus disease 2019 pan
To determine if digitally assisted rehabilitation could be as practical, or even more effective, than the traditional methods most patients currently follow.
Six electronic databases, including PubMed, Scopus, Cochrane Library, Google Scholar, EMBASE, and Web of Science, were searched to find articles that com
Three randomized controlled trial studies were enrolled in this study, including 195 cases. We did not find any significant differences between the two groups in terms of DASH score, flexion range of motion, and external rotation range of motion. There was a significant difference between the two groups for abduction range of motion.
Digital home-based rehab seems to be a strong alternative to traditional methods, offering similar results for people recovering from rotator cuff surgery. This approach might also make rehab more accessible and engaging for patients. That said, further research is needed to fully understand the potential of digital rehabilitation and ensure it works effectively for everyone.
Core Tip: This systematic review and meta-analysis evaluated the effectiveness of digitally assisted vs conventional home-based rehabilitation following rotator cuff repair. Findings from three randomized controlled trials suggest that digital rehabilitation offers comparable outcomes in Disabilities of the Arm, Shoulder and Hand scores and range of motion—with a significant improvement in abduction—highlighting its potential as an accessible, patient-friendly alternative to traditional methods. While promising, broader implementation requires addressing barriers like digital literacy, access, and privacy concerns.
- Citation: Salimi M, Keshtkar A, Mosalamiaghili S, Sharafatvaziri A, Feeley BT. Digitally assisted vs conventional home-based rehabilitation after rotator cuff repair: A meta-analysis. World J Clin Cases 2025; 13(32): 109464
- URL: https://www.wjgnet.com/2307-8960/full/v13/i32/109464.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i32.109464
Rotator cuff tears are one of the most common causes of shoulder pain and disability, affecting almost 30% of individuals older than 60 years[1]. Surgical intervention, specifically rotator cuff repair, is the second line of treatment after about 40% of patients do not respond to conservative physical therapy (PT)[2-4]. In the United States alone, more than 300000 rotator cuff repair (RCR) are performed annually, accounting for an annual financial burden of $3 billion on the United States economy[5,6]. Factors such as tear size and patient-specific risk factors are crucial in determining a patient's suitability for surgical intervention. Rehabilitation following rotator cuff repair surgery is critical for recovery and the return[7-11] of function.
With an aging population and increasing surgical intervention rates, rotator cuff repair has become a common and costly procedure, with over 300000 surgeries annually in the United States alone. The coronavirus disease 2019 (COVID-19) pandemic accelerated the adoption of digital health tools, making digital rehabilitation a critical alternative to traditional care. Digital health platforms, now more accessible than ever, offer scalable, patient-centered solutions that may improve recovery outcomes and adherence.
Rehabilitation typically involves in-person PT sessions guided by healthcare professionals. These programs rely on patients performing exercises in person, and then repeating them at home, with periodic in-person visits with their surgeon for assessment and progression of the rehabilitation plan[12,13]. The COVID-19 pandemic has created a new need for home-based digital solutions for the rehabilitation process[14,15]. These home-based rehabilitations without real-time human supervision offer the potential to improve the efficiency and reduce the costs of rehabilitation.
Digitally assisted rehabilitation programs leverage various technologies, such as mobile applications, augmented reality (AR), and telehealth platforms, to deliver personalized and interactive rehabilitation exercises remotely[16]. Evidence shows that digital therapeutics can enhance outcomes, personalize care, and reduce costs[17]. While it has been shown extensively that internet-based rehabilitation have the similar effects in comparison to face-to-face rehabilitation in some orthopedic-related condition such as joint replacement[18-23], there remains significant unexplored potential in the field of post-rotator cuff repair rehabilitation[24,25].
While both conventional and digitally assisted home-based rehabilitation programs have shown promise, there is a lack of comprehensive comparison between these two approaches in the context of post-cuff repair recovery. This systematic review and meta-analysis identify strategies that optimize patient outcomes by comparing digitally assisted and conventional home-based rehabilitation programs.
Preferred reporting items of systematic reviews and meta-analysis was used to conduct this study[26].
A systematic search was done in PubMed, Scopus, Cochrane Library, Google Scholar, EMBASE, and Web of Science to find clinical trials investigating digital rehabilitation's role for patients who had rotator cuff rupture. To find these article MESH words including (“Virtual reality”, “Augmented reality”, “Virtual Reality, Exposure Therapy”, Exergaming) AND (“Rotator Cuff”, “Rotator Cuff Tear Arthropathy”, “Rotator Cuff Injuries”) was used. Moreover, relevant non-MESH words were also searched in the mentioned databases including (“Active-Video Gaming*”, “Educational Virtual Realit*”, “Instructional Virtual Realit*”, “Mixed Realit*”, “Virtual Reality Immersion Therapy”) AND (“Cuff Tear Arthropathy”, “Milwaukee Shoulder”, “Rotator Cuff Tendiniti*”, “Rotator Cuff Tendinos*”, “Glenoid Labral Tear*”). Furthermore, all reference list of articles that met the inclusion were manually searched to find all relevant articles (Supplementary Table 1).
Inclusion criteria: Patients who used digital rehabilitation after rotator cuff surgery or rapture. Parallel or cross-over randomized control trials. Cohort studies.
Exclusion criteria: Review articles. Study protocols. Articles that did not report the outcome in both intervention and control groups.
Two authors independently checked the articles to find relevant articles. Any disagreement between the authors was discussed between them. After discussing the disagreements, senior author was consulted if the author did not reach an agreement. This article did not have any language restriction to find eligible articles.
Data extraction was also done by two authors independently whereas senior author was also present to resolve disagreements. A checklist was designed consisting of first author's name, year of publication, study participants, kind of digital rehabilitation used, comparison group, outcomes, follow-up, and any funding of conflict of interest reported in the study. In cases that an article has reported the outcome at different times, we extracted the post-treatment one.
Quality assessment was done independently by two authors using the Cochrane risk-of-bias tool for randomized trials for randomized clinical trial articles and the New-Castle Ottawa statement for cohort studies (Table 1)[27-29].
Statistical analysis of this study was done by STATA software version 18 (Stata Corp. College Station, TX, United States). Mean and SD of the articles were used to calculate the effect size. All of the included articles were used mean and SD in their study so no changes were made to calculate the mean and SD. Random (when I2 was more than 50%) or fixed effect models were used to assess the overall effect size. P value less than 0.05 was considered statistically significant.
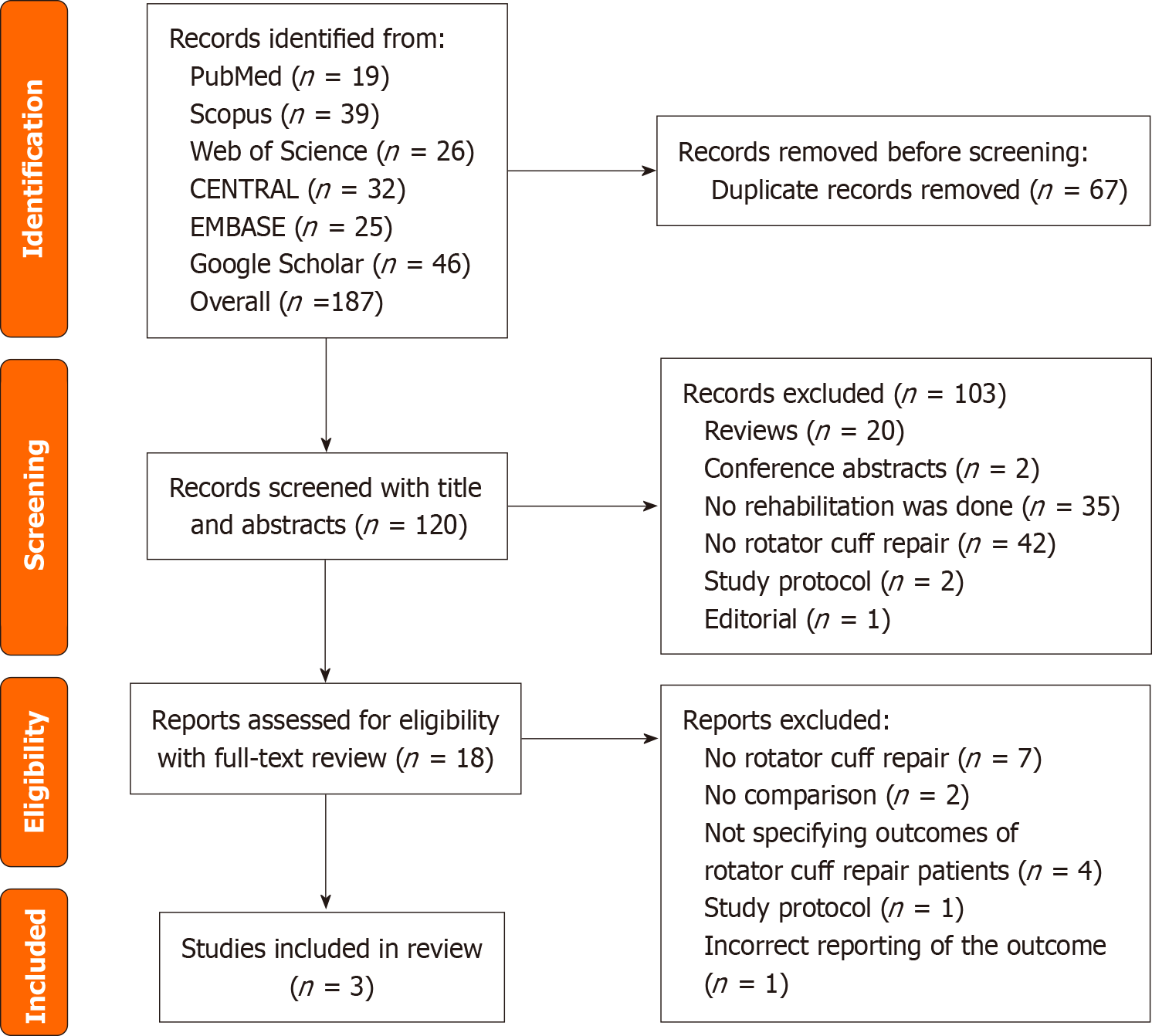
Total 187 studies were included for screening and 67 of them were duplicated and removed. 120 articles entered the screening process. 101 articles were excluded and 18 were entered into the full-text screening process. 15 articles were excluded in this phase because seven studies did not report rotator cuff rapture, and four of them did not specify outcomes of rotator cuff repair patients, two of them had no comparison between the conventional rehabilitation and digital-based rehabilitation, one was study protocol and one of them was not reporting the outcome correctly. Finally, three studies find eligibility to enter the review (Figure 1). Moreover, the reason for the exclusion of each included studies were reported in the Supplementary Table 2.
Two studies[27,28] were published in 2022 and one of them[29] in 2023. The participants of the studies ranged between 30 to 115 cases. All the studies included both male and female genders. 195 patients were included in our review with a mean age of 56.72 ± 6.60. 126 (64%) of patients were female. The duration of digital rehabilitation was between 6 to 12 weeks and the duration of follow-up was 6 weeks to 12 months. Detailed characteristics of the included studies are reported in Table 2[27-29].
| Ref. | Country | Study design | Population | Digital rehabilitation intervention | Comparison | Outcome of interest | Longest Follow-up period | Funding and conflict of interest |
| Correia et al[27], 2022 | Portugal | Nonblind parallel randomized controlled trial | All patients over 18 years old and under 70 years old who had primary arthroscopic rotator cuff repair | Mobile app+ inertial motion trackers: Immediate post-surgery phase (weeks 0-2); immobilization period (weeks 3-4); passive mobilization (weeks 5-8); active movement (weeks 9-10); and strengthening (weeks 11-12) performed for both groups. Patients in digital assistance used SWORD mobile app installed on their phone, along with three inertial motion trackers | Conventional therapy | CM score, quick DASH score, shoulder active pain-free range of motion | 12 months | The writers of this article were the employee and chief medical officer of SWORD health |
| Menek et al[28], 2022 | Turkey | Single blinded randomized controlled trial | Individuals with partial rupture of the rotator cuff aged between 18-60 without previous shoulder surgery | Video-base game rehabilitation: A video-based game using "Arm rotate" and "Uball" by using Fizuosoft Extremity range of motion. Moreover, "Balance adventure" and "Balance surf" games by using the Fizyosoft Balance System. These games were used twice a week for 6 weeks under the supervision of a physiotherapist | Conventional therapy: Wand and shoulder wheel exercise, finger ladder exercise, holding the endpoint, and stretching exercises. These exercises were performed twice a week for 6 weeks | Pain severity (VAS), pain threshold (Algometer), evaluation of joint ROM (Fizyosoft Extremity ROM), joint position sense, evaluation of shoulder approximation force, evaluation of shoulder approximation force (DASH), evaluation of quality of life for the shoulder (RCQOL) | 6 weeks | None |
| Shim et al[29], 2023 | South Korea | Single blinded randomize controlled trial | Patients ≥ 50 years old who underwent rotator cuff repair surgery | AR-based rehabilitation: It consists of three phases including on-brace phase (from immediate to 6 weeks postoperatively), the off-brace phase (6-9 weeks postoperatively), and the active mobilization phase (9-12 weeks post-operatively) by using brochure-based exercises for 6 weeks followed by AR-based exercises for 6 weeks | Conventional treatment: The same as digital rehabilitation except they did not use AR based rehabilitation for them and just used brochure-based exercises for 12 weeks | Simple shoulder test change, DASH score, SPADI index, EQ5D5 L questionnaire, NRS, and shoulder ROM | 24 weeks | Funded by the Ministry of Health Welfare, Republic of Korea/No conflict of interest reported |
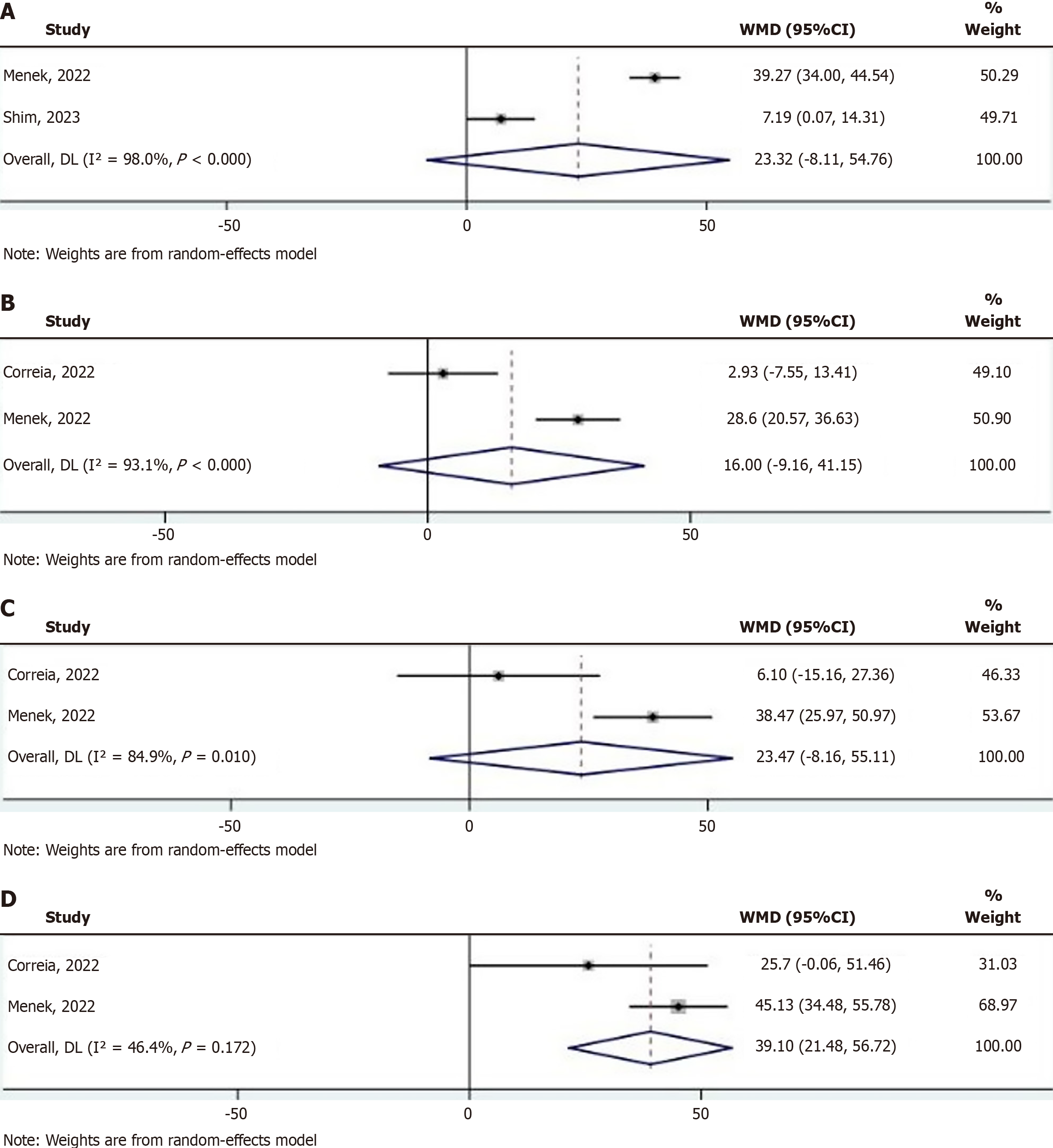
Based on two studies[28,29], indicated that there are no significant differences between digital-based rehabilitation and conventional rehabilitation in DASH score [weighted mean difference (WMD): 23.32 and 95%CI: -8.11 to 54.76. There was significant between-study heterogenicity (I2: 98%, P < 0.001) (Figure 2A).
Moreover, we could not find significant differences between the two groups for external rotation (WMD: 16 and 95%CI: -9.16 to 41.15) and flexion range of motion (WMD: 23.47 and 95%CI: -8.16 to 55.11). Both results showed significant between-study heterogeneity with I2: 93.1, P < 0.001 and I2: 84.9%, P < 0.001 respectively (Figure 2B and C).
We find significant differences between two groups in abduction range of motion with WMD: 39.10, 95%CI: 21.48-56.72. There was no significant heterogenicity between studies with I2: 46%, P = 0.17 (Figure 2D).
Our meta-analysis aimed to compare digitally assisted and conventional home-based rehabilitation for patients re
In terms of patient-reported outcomes (PROs), our analysis showed mixed but generally comparable results between digital and conventional rehabilitation. Shim et al[29] reported significant improvements in the Disabilities of the Arm, Shoulder and Hand (DASH) score, Shoulder Pain and Disability Index, and EQ5D5 L scores over time in their digital rehabilitation group compared to the conventional rehabilitation group. Similarly, Menek et al[28] found significant improvements in functionality and quality of life measures in their video game exercise group. Correia et al[27] reported superior Quick DASH score improvements in both their digital and conventional groups compared to previous studies[30-32], suggesting that both approaches can lead to significant improvements in PROs.
Regarding of range of motion, our findings were similarly mixed, but generally showed no significant differences between digital and conventional approaches for most movements. While our initial analysis suggested a potential improvement in abduction range of motion favoring digitally assisted rehabilitation, it's important to note that this finding may be due to underpowered studies or random effects rather than a true superiority of digital interventions. Both Correia et al[27] and Menek et al[28] reported improvements in range of motion, with no clear superiority of digital over conventional methods. These results suggest that digital rehabilitation can achieve range of motion outcomes comparable to conventional rehabilitation, which is the primary concern for patients undergoing rotator cuff repair recovery.
The effectiveness of digital rehabilitation interventions observed in our meta-analysis may be attributed to several factors. Digital interventions often provide visual and sensory feedback, which can increase patient engagement and potentially lead to better adherence to exercise regimens[33,34]. They also allow for more frequent and targeted exercises, with real-time feedback and monitoring enabling more personalized and adaptive rehabilitation programs. Additionally, digital platforms may promote long-term behavior change, as suggested by Correia et al's observation of better functional outcomes in the digital group at 12 months post-intervention[27].
However, digital technology in rehabilitation also presents several limitations that must be acknowledged. These include challenges in identifying red flags, equipment barriers, reimbursement issues for telerehabilitation services, medicolegal concerns, lack of digital literacy and skills, and limited access. To address these limitations, initial face-to-face visits should be conducted for complex cases, necessary equipment should be planned for upfront, and personalized technological tools should be used to protect patient privacy and health-related data.
While digital technology offers numerous advantages for rehabilitation, it also presents several limitations that must be acknowledged. These include challenges in identifying red flags, equipment barriers, reimbursement issues for telerehabilitation services, medicolegal concerns, lack of digital literacy and skills, and limited access. To address these limitations, several solutions can be implemented. For complex cases, initial face-to-face visits should be conducted to screen for any red flags[35]. Planning for necessary equipment should be done upfront, and monthly subscription fees can be adjusted based on the diagnosis. Additionally, protecting patient privacy and health-related data is crucial, which can be achieved by using personalized technological tools. Customized and individualized protocols should be developed following a detailed assessment of each patient[36].
To overcome barriers to digital rehabilitation, clinical pathways could include hybrid rehab models with initial in-person sessions followed by remote monitoring. Ensuring equitable access, educating patients on digital literacy, and using secure, personalized platforms are essential. Future research should prioritize large, multicenter randomized controlled trial s with standardized outcome reporting and inclusion of diverse patient populations.
The high heterogeneity observed in most pooled outcomes, particularly for DASH score and flexion range of motion, suggests variability across study designs, patient populations, types of digital interventions, and follow-up durations. Small sample sizes and different outcome reporting methods may also contribute. Future meta-analyses may benefit from subgroup analyses stratified by digital modality, rehab duration, and geographic region to minimize statistical variability.
Our study has several limitations that warrant consideration. The small number of included studies (n = 3) and participants limits the generalizability of our findings and increases the risk of bias. The high heterogeneity observed in most outcomes suggests considerable variability in study designs, interventions, and outcome measures. It's also important to note that patients in the digital platforms knew they were being studied, which may have led to improved performance due to the Hawthorne effect. This potential bias should be considered when interpreting the results of digital rehabilitation studies.
Our findings show that digital rehab is a promising option for many patients, offering convenience without sacrificing effectiveness. But it’s important to choose the right approach for each individual. As digital health tools continue to evolve, they could play a significant role in making recovery easier and more accessible for everyone. In short, digital rehabilitation has the potential to change the way we approach recovery after rotator cuff surgery, but it’s essential to keep the patient’s specific needs in mind when deciding the best path forward.
| 1. | Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699-1704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 550] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 2. | Ross D, Maerz T, Lynch J, Norris S, Baker K, Anderson K. Rehabilitation following arthroscopic rotator cuff repair: a review of current literature. J Am Acad Orthop Surg. 2014;22:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Wani Z, Abdulla M, Habeebullah A, Kalogriantis S. Rotator cuff tears: Review of epidemiology, clinical assessment and operative treatment. Trauma. 2016;18:190-204. [RCA] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | van der Windt DA, Koes BW, Boeke AJ, Devillé W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract. 1996;46:519-523. [PubMed] |
| 5. | Aurora A, McCarron J, Iannotti JP, Derwin K. Commercially available extracellular matrix materials for rotator cuff repairs: state of the art and future trends. J Shoulder Elbow Surg. 2007;16:S171-S178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 119] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Barr KP. Rotator cuff disease. Phys Med Rehabil Clin N Am. 2004;15:475-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 33] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Jackins S. Postoperative shoulder rehabilitation. Phys Med Rehabil Clin N Am. 2004;15:vi, 643-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Kokmeyer D, Dube E, Millett PJ. Prognosis Driven Rehabilitation After Rotator Cuff Repair Surgery. Open Orthop J. 2016;10:339-348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Littlewood C, Bateman M. Rehabilitation following rotator cuff repair: a survey of current UK practice. Shoulder Elbow. 2015;7:193-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Millett PJ, Wilcox RB 3rd, O'Holleran JD, Warner JJ. Rehabilitation of the rotator cuff: an evaluation-based approach. J Am Acad Orthop Surg. 2006;14:599-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 97] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012;31:589-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 475] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 12. | Sciarretta FV, Moya D, List K. Current trends in rehabilitation of rotator cuff injuries. SICOT J. 2023;9:14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 13. | Lisinski P, Huber J, Wilkosz P, Witkowska A, Wytrazek M, Samborski W, Zagloba A. Supervised versus uncontrolled rehabilitation of patients after rotator cuff repair-clinical and neurophysiological comparative study. Int J Artif Organs. 2012;35:45-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Eccleston C, Blyth FM, Dear BF, Fisher EA, Keefe FJ, Lynch ME, Palermo TM, Reid MC, Williams ACC. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain. 2020;161:889-893. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 344] [Cited by in RCA: 339] [Article Influence: 56.5] [Reference Citation Analysis (0)] |
| 15. | Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, Curtis S, Roman M, Poon EG, Ferranti J, Katz JN, Tcheng J. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27:957-962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 965] [Cited by in RCA: 993] [Article Influence: 165.5] [Reference Citation Analysis (0)] |
| 16. | Viglialoro RM, Condino S, Turini G, Carbone M, Ferrari V, Gesi M. Review of the Augmented Reality Systems for Shoulder Rehabilitation. Information. 2019;10:154. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Bain EE, Shafner L, Walling DP, Othman AA, Chuang-Stein C, Hinkle J, Hanina A. Use of a Novel Artificial Intelligence Platform on Mobile Devices to Assess Dosing Compliance in a Phase 2 Clinical Trial in Subjects With Schizophrenia. JMIR Mhealth Uhealth. 2017;5:e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 18. | Wang Q, Lee RL, Hunter S, Chan SW. The effectiveness of internet-based telerehabilitation among patients after total joint arthroplasty: A systematic review and meta-analysis of randomised controlled trials. J Telemed Telecare. 2023;29:247-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Moffet H, Tousignant M, Nadeau S, Mérette C, Boissy P, Corriveau H, Marquis F, Cabana F, Belzile ÉL, Ranger P, Dimentberg R. Patient Satisfaction with In-Home Telerehabilitation After Total Knee Arthroplasty: Results from a Randomized Controlled Trial. Telemed J E Health. 2017;23:80-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 97] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 20. | Moffet H, Tousignant M, Nadeau S, Mérette C, Boissy P, Corriveau H, Marquis F, Cabana F, Ranger P, Belzile ÉL, Dimentberg R. In-Home Telerehabilitation Compared with Face-to-Face Rehabilitation After Total Knee Arthroplasty: A Noninferiority Randomized Controlled Trial. J Bone Joint Surg Am. 2015;97:1129-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 208] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 21. | Russell TG, Buttrum P, Wootton R, Jull GA. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2011;93:113-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 274] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 22. | Russell TG, Buttrum P, Wootton R, Jull GA. Low-bandwidth telerehabilitation for patients who have undergone total knee replacement: preliminary results. J Telemed Telecare. 2003;9 Suppl 2:S44-S47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 54] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Tousignant M, Boissy P, Moffet H, Corriveau H, Cabana F, Marquis F, Simard J. Patients' satisfaction of healthcare services and perception with in-home telerehabilitation and physiotherapists' satisfaction toward technology for post-knee arthroplasty: an embedded study in a randomized trial. Telemed J E Health. 2011;17:376-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 117] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 24. | Carnevale A, Longo UG, Schena E, Massaroni C, Lo Presti D, Berton A, Candela V, Denaro V. Wearable systems for shoulder kinematics assessment: a systematic review. BMC Musculoskelet Disord. 2019;20:546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 25. | Wang Q, Markopoulos P, Yu B, Chen W, Timmermans A. Interactive wearable systems for upper body rehabilitation: a systematic review. J Neuroeng Rehabil. 2017;14:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 172] [Cited by in RCA: 178] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 26. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9207] [Cited by in RCA: 8336] [Article Influence: 521.0] [Reference Citation Analysis (2)] |
| 27. | Correia FD, Molinos M, Luís S, Carvalho D, Carvalho C, Costa P, Seabra R, Francisco G, Bento V, Lains J. Digitally Assisted Versus Conventional Home-Based Rehabilitation After Arthroscopic Rotator Cuff Repair: A Randomized Controlled Trial. Am J Phys Med Rehabil. 2022;101:237-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 28. | Menek B, Tarakci D, Tarakci E, Menek MY. Investigation on the Efficiency of the Closed Kinetic Chain and Video-Based Game Exercise Programs in the Rotator Cuff Rupture: A Randomized Trial. Games Health J. 2022;11:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 29. | Shim GY, Kim EH, Baek YJ, Chang WK, Kim BR, Oh JH, Lee JI, Hwang JH, Lim JY. A randomized controlled trial of postoperative rehabilitation using digital healthcare system after rotator cuff repair. NPJ Digit Med. 2023;6:95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 30. | Macdermid JC, Khadilkar L, Birmingham TB, Athwal GS. Validity of the QuickDASH in patients with shoulder-related disorders undergoing surgery. J Orthop Sports Phys Ther. 2015;45:25-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 31. | Nishimori M, Warner JJ, Gill TJ, Warren L, Carwood CM, Ballantyne JC. Long term outcomes following discharge from shoulder surgery in an ambulatory setting. Ambul Surg. 2007;13:72-76. |
| 32. | Feyzioğlu Ö, Dinçer S, Akan A, Algun ZC. Is Xbox 360 Kinect-based virtual reality training as effective as standard physiotherapy in patients undergoing breast cancer surgery? Support Care Cancer. 2020;28:4295-4303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 33. | Gianola S, Stucovitz E, Castellini G, Mascali M, Vanni F, Tramacere I, Banfi G, Tornese D. Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty: A randomized controlled trial. Medicine (Baltimore). 2020;99:e19136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 34. | Moody L, Wood E, Needham A, Booth A, Jimenez-Aranda A, Tindale W. Identifying individual enablers and barriers to the use of digital technology for the self-management of long-term conditions by older adults. J Med Eng Technol. 2022;46:448-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 35. | Turolla A, Rossettini G, Viceconti A, Palese A, Geri T. Musculoskeletal Physical Therapy During the COVID-19 Pandemic: Is Telerehabilitation the Answer? Phys Ther. 2020;100:1260-1264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 112] [Cited by in RCA: 175] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 36. | McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67:267-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1210] [Cited by in RCA: 1596] [Article Influence: 122.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/