Published online Oct 6, 2025. doi: 10.12998/wjcc.v13.i28.108710
Revised: May 25, 2025
Accepted: July 8, 2025
Published online: October 6, 2025
Processing time: 108 Days and 5.3 Hours
Managing Gustilo type IIIB fractures in patients with type 2 diabetes is cha
To evaluate free-flap transfer with plate fixation for managing Gustilo IIIB fractures in diabetic patients, focusing on outcomes.
A retrospective analysis of six cases was conducted with a minimum follow-up period of three years. Patients underwent free-flap transfer and plate fixation for fracture management. Outcomes assessed included bone union, flap viability, and complications requiring intervention or plate removal. The follow-up period ranged from three to four years. Persistent infections beneath the flap developed in two patients, necessitating daily wound care.
Bone healing occurred within 17 to 34 months, with plate removal required in three patients after fracture consolidation. Traumatic osteomyelitis was observed in at least one patient. Despite challenges such as sinus formation and variations in flap pedicle anatomy, successful bone union and flap viability were achieved in all cases. Free-flap transfer combined with plate fixation shows promise for treating Gustilo type IIIB fractures in patients with diabetes. While infection and the need for plate removal surgeries were observed, consistent success in bone healing and flap viability highlights the potential of this approach.
Free-flap transfer with plate fixation effectively manages Gustilo IIIB fractures in diabetics, achieving bone/flap healing despite infection risks. Careful patient selection and further validation are critical.
Core Tip: Employing free flap transfer with plate fixation for Gustilo IIIB fractures in patients with type II diabetes shows promise in achieving successful bone union and flap viability despite challenges such as infections and plate removal. Careful patient selection and precise indications are crucial for optimizing outcomes in fracture management for diabetic individuals.
- Citation: Bao Q, Pan SW, Gong XK, Wang B, Wei ZN, Xu YQ, Zhu YL, Shi Z. Efficacy of free-flap-transfer and plate-fixation for Gustilo IIIB fractures in type II diabetic patients: A retrospective study. World J Clin Cases 2025; 13(28): 108710
- URL: https://www.wjgnet.com/2307-8960/full/v13/i28/108710.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i28.108710
Recent research has provided compelling evidence linking type II diabetes to an increased risk of fractures[1]. Among individuals with diabetes who sustain fractures, hyperglycemia has been shown to impair microcirculatory function, thereby compromising blood supply to the fracture site[2,3]. Additionally, diabetes negatively affects immune function[4], rendering patients more susceptible to infections[5]. Consequently, patients with diabetes who experience fractures often exhibit delayed healing, a greater likelihood of hardware failure, an increased risk of wound dehiscence, and higher susceptibility to infections compared with non-diabetic individuals[6,7]. Furthermore, these patients are at a significantly higher risk of developing soft tissue complications following fractures[6].
In the emergency management of Gustilo IIIB fractures in patients with diabetes, external fixation (EF) combined with flap coverage emerges as a viable therapeutic option[8,9]. This approach offers several advantages, including a reduced risk of infection and reliable stabilization of fractures[10,11]. However, it is associated with prolonged hospital stays and increased financial costs[12,13]. Despite these drawbacks, EF with flap coverage remains a valuable approach. Notably, there is limited literature on plate fixation and free flap coverage techniques, and considerable debate persists regarding the suitability of open reduction and internal fixation (ORIF) as the optimal treatment for diabetic fractures[14].
For larger wounds, the use of free flaps, which offer greater volume than local flaps, provides superior protection for IF devices and exposed bone[15]. Free flaps enhance vascularization through pedicle anastomosis, improving blood supply to the wound bed[16]. Importantly, hyperglycemia does not appear to correlate with an increased risk of flap failure[17]. The theoretical advantages of this approach include secure osseous fixation, comprehensive wound coverage with optimal vascularity, and avoidance of prolonged EF. In this study, we aimed to evaluate the indications, surgical te
A retrospective study was conducted at the 920th Hospital of Joint Logistics Support Force of PLA, Kunming, China from January 2015 to December 2018 to evaluate the efficacy of a treatment approach involving free flap transfer, plate fixation, and exposed bone management in six cases of Gustilo type IIIB fractures with concomitant type 2 diabetes. The study cohort consisted of patients with a mean age of 48 years (range: 34–67 years) at the time of injury. The postoperative hospital stay ranged from 17 to 41 days, with a mean duration of 23.2 days.
Postoperatively, flap viability was monitored three times daily to assess the success of the surgical intervention. Radiographic evaluations were performed two weeks after surgery to assess the effectiveness of plate fixation. Once satisfactory results were confirmed, the flap sutures were removed, and the patients were discharged from the hospital. A six-week course of antibiotics was administered postoperatively to reduce the risk of infection.
Following surgery, a structured non-weight-bearing ambulation protocol was implemented, emphasizing active mobilization of the knee and ankle joints. At six weeks post-surgery, partial weight-bearing was gradually introduced, progressing to full weight-bearing upon confirmation of a bridging callus. For patients undergoing upper limb re
Postoperative imaging evaluations were performed immediately after surgery and subsequently at regular intervals of 6–8 weeks. Radiographic assessments meticulously analyzed fracture healing, which was defined as the presence of a bridging callus in at least three of the four cortices, as observed in anteroposterior, lateral, and oblique views.
The study design and methodology aimed to comprehensively evaluate the treatment approach and outcomes for Gustilo type IIIB fractures.
Upon admission to the operating room, patients were administered intravenous prophylactic antibiotics. The initial surgical procedure involved thorough debridement of devitalized and contaminated tissues using a 6-liter saline wash under tourniquet control to ensure hemostasis. All necrotic tissue was meticulously excised, and bone length was stabilized with plaster splints. The wound was subsequently covered with a vacuum-assisted closure (VAC) dressing, utilizing the VERAFLO Dressing Kit (Smith and Nephew). Postoperatively, patients received a 72-hour course of first-generation cephalosporin antibiotics. The anteroposterior tibial and radial/ulnar arteries were identified and marked to facilitate subsequent anastomosis with the vascular pedicle of the free flap. Repeated debridement and VAC were performed until the wound displayed clean tissue and robust granulation.
Reconstructive surgery was conducted under general anesthesia, with patients positioned in both supine and lateral postures (the lateral position was exclusively used for free flap harvest). Both surgical teams operated simultaneously, performing their respective procedures. Group 1 irrigated the wound with 3 liters of sterile saline solution and performed fracture fixation using locking compression plates (LCPs). The recipient flap arteries and veins were carefully identified, exposed, and prepared.
Group 2 focused on meticulous flap harvesting. Flap dimensions were designed to exceed the defect size by 1 cm in both width and length. For vascular anastomosis, the vascular pedicles of the free lateral circumflex femoral artery perforator (LCFAP) flap (n = 1) and the free peroneal artery perforator flaps (n = 3) were precisely anastomosed to the radial/ulnar arteries and veins and the cephalic vein, respectively. Similarly, the pedicles of the latissimus dorsi (LD) flaps (n = 2) were anastomosed as follows: one to the posterior tibial artery/vein, and one to the anterior tibial artery/vein. Following the completion of pedicle anastomosis, flap viability was rigorously assessed. All reconstructive procedures were performed in a single session.
The surgical technique adhered to meticulous standards, consistent with established academic and professional guidelines.
During hospitalization, patient management included short-acting insulin for blood glucose control and long-term glucose monitoring. The therapeutic target was to maintain random non-fasting blood glucose levels below 10.0 mmol/L, with an HbA1c level under 7.0%.
The study included six patients treated using the proposed approach. The follow-up period ranged from 3 to 4 years, with no dropouts recorded. Two patients (cases 4 and 5) developed chronic infections beneath the flap post-surgery, presenting as small sinuses at the flap edge with persistent fluid collection lasting 8 and 11 months, respectively. These sinuses were managed by daily wound care. Bone healing, the primary outcome measure, was defined as the presence of a bridging callus at the fracture site, confirmed by radiographic evidence and the absence of pain during weight-bearing. The time to achieve bone healing ranged from 17 to 34 months. Three patients (cases 1, 4, and 5) underwent plate removal surgery after fracture healing. At least one patient experienced traumatic osteomyelitis during the minimum 3-year follow-up period.
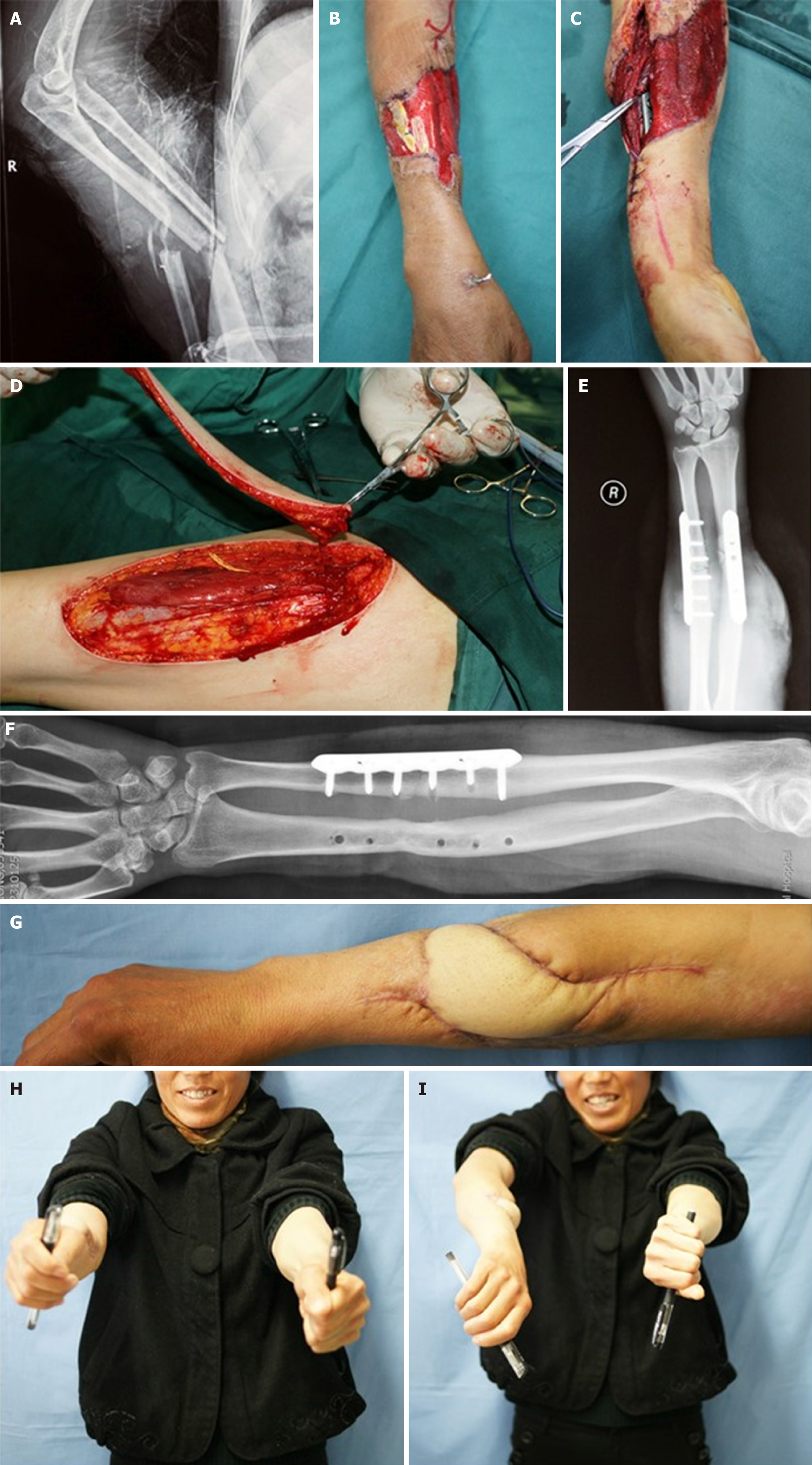
Case 1: A 40-year-old female worker sustained a machine-induced right forearm injury. Multiple debridement procedures and VAC were performed before the final surgery. The radial and ulnar fractures were stabilized using LCP. A free LCFAP flap was harvested to cover the soft tissue defect. Postoperative radiography confirmed satisfactory bone fixation. Two years later, the radial fracture healed, and the plate was removed, while the ulnar bone required extended plate fixation. The flap successfully integrated into the forearm, allowing acceptable forearm rotation (Figure 1).
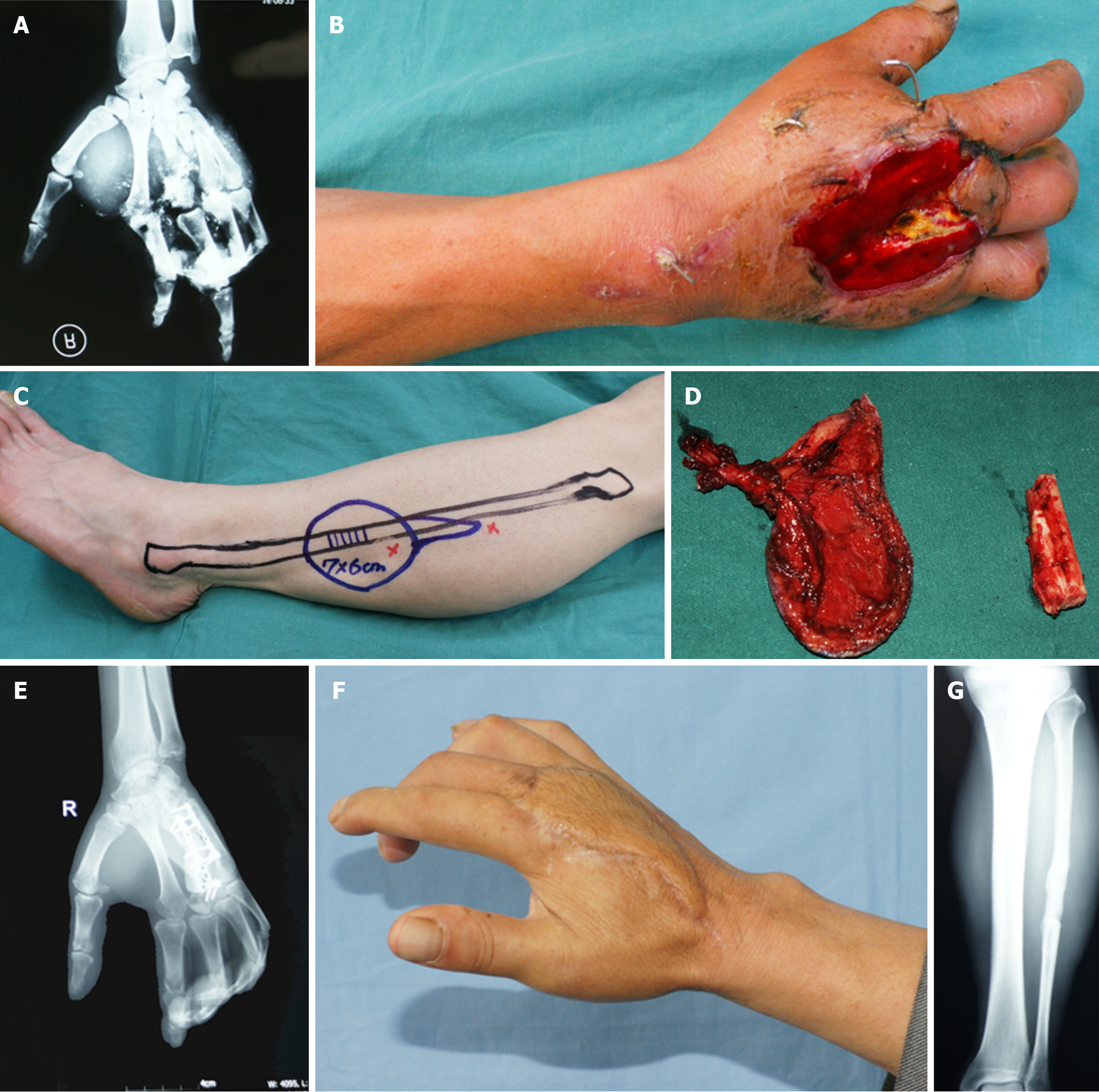
Case 2: A patient sustained a crushed right hand caused by a large stone, leading to multiple metacarpal fractures and dislocation of the third metacarpal. Following wound debridement, VAC, and temporary Kirschner wire fixation, the wound was prepared for a one-stage bone and skin defect repair. A composite fibular artery perforator flap was designed. However, intraoperative assessment revealed that the fibula was too large for the third metacarpal; therefore, half of its diameter was harvested. The fractures were fixed using a small metacarpal LCP. Bone healing occurred within nine months, and the flap recovered well. The remaining half of the fibula was reconnected during the procedure (Figure 2). No complications were noted during the 3-year follow-up.
Case 3: The patient presented with open, multiple metacarpal fractures caused by machinery, with exposed bones and dorsal tendons. A free fibular artery perforator flap was harvested, and bone fixation was performed using a mini-LCP. After 27 months, the flap was fully integrated, and wrist function was optimally preserved. Radiographic evaluation confirmed bone healing (Figure 3).
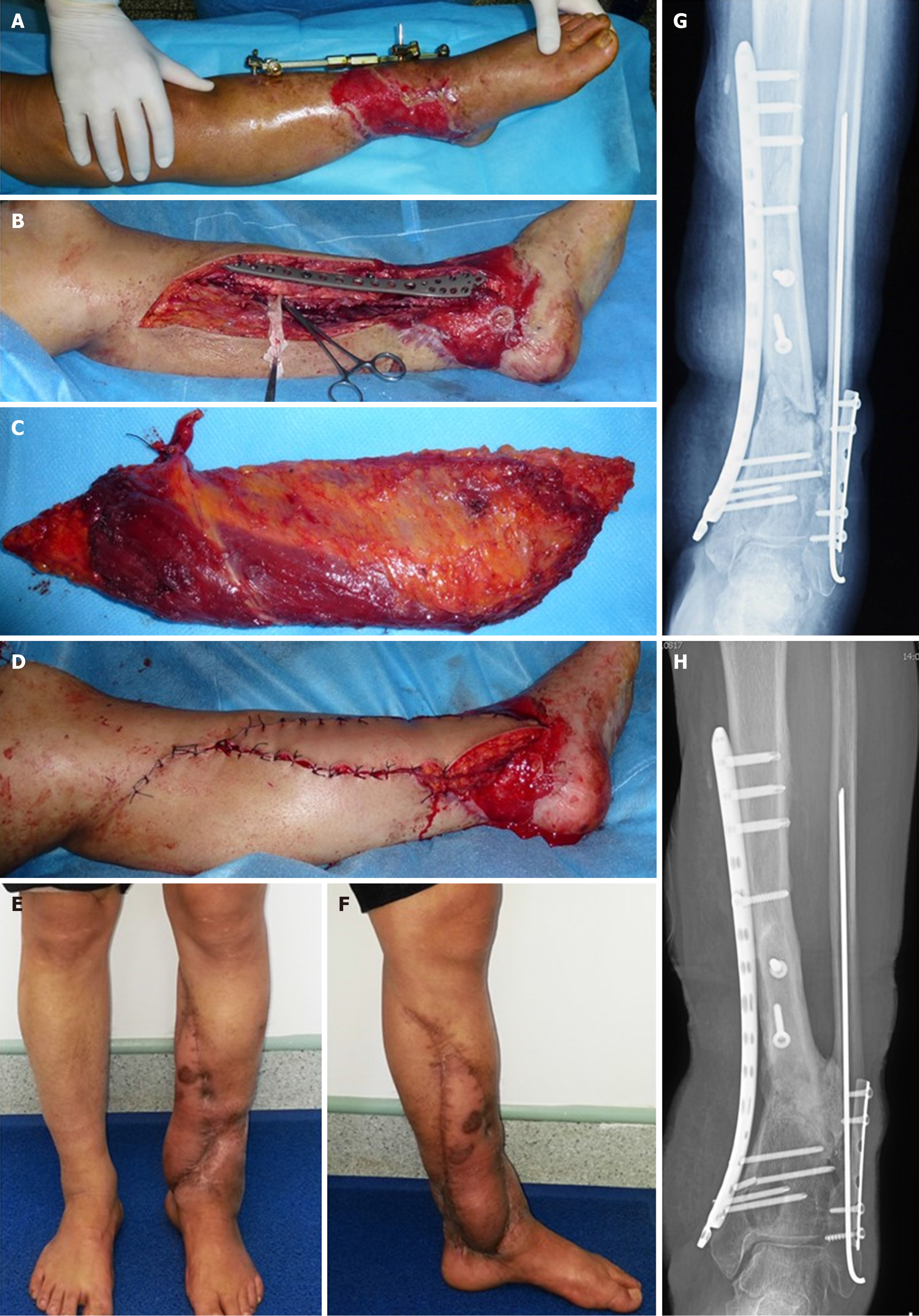
Case 4: A 57-year-old patient with diabetes sustained a left leg crush injury caused by a stone. After EF, wound debridement, and diabetes management, the wound was prepared for one-stage reconstruction 26 days post-injury. A free LD flap with a robust blood supply was used to enhance local tissue nutrition postoperatively. Bone fixation was achieved using locking plates upon external fixator removal. A small sinus at the flap's outer edge healed with daily wound care. Bone healing, absent at 18 months, was observed at 30 months, after which the IF was removed (Figure 4).
Case 5: The patient sustained a tibial fracture in a motor vehicle accident, initially stabilized using an external fixator. Thirty days later, the wound was prepared for definitive surgery. The external fixator was removed, and fixation with LCP was performed following microsurgical anastomosis of the tibial vessels. A free LD flap was used to cover the bone and plate. The flap developed a small sinus that persisted for 11 months but resolved with daily wound care. Full flap recovery was achieved at 30 months. Bone healing was not observed at 18 months but was confirmed at 29 months (Figure 5).
Case 6: The patient sustained a proximal right forearm injury caused by machinery, leading to significant infection and extensive necrotic tissue. Following debridement and VAC, the wound was prepared for reconstruction. A composite fibular artery perforator flap was designed. During dissection, it was found that the flap pedicle originated from the lateral vessels of the peroneus longus muscle rather than the peroneal vessels. Consequently, the free fibula and flap were separately anastomosed to the recipient sites (Figure 6).
Recent studies have demonstrated an association between type II diabetes and an increased risk of fractures, even though microvascular and macrovascular complications are the most prevalent in individuals with diabetes. Diabetes-related skeletal disorders include osteoporotic fractures, Charcot arthropathy, and renal osteodystrophy resulting from diabetic nephropathy. Traumatic fractures in patients with diabetes are accompanied by impaired microcirculation due to elevated blood glucose levels, leading to compromised blood supply at the fracture site and delayed healing. Addi
Compared to IF, EF exhibits the lowest infection rate, making it a prominent technique for stabilizing open fractures. Nevertheless, the prolonged application of EF, susceptibility to pin-site infections, and associated patient discomfort have driven the exploration of alternative fixation methods. For tibial fractures, some studies have reported using intra
Muscle flaps with pedicles have been employed to cover exposed prostheses or hardware[26,27]. However, free flaps offer distinct advantages due to their larger dimensions and superior vascularity, allowing surgeons to manage extensive wound defects more effectively[28]. In addition to providing broader coverage, wide free flaps, such as the free LD muscle flap, offer enhanced perfusion, potentially improving limb salvage rates. Notably, even in the presence of diabetes, which predisposes individuals to an increased risk of osteomyelitis (Case 5), residual bacteria within the wound can be effectively eradicated using free-flap techniques.
The impact of diabetes on flap survival remains debated. Early studies suggested that diabetes contributes to atheromatous small vessel disease and defective intimal repair mechanisms, increasing the likelihood of compromised flap perfusion, obstruction, and anastomotic failure, ultimately leading to unsuccessful flap surgeries[29,30]. However, free flaps have demonstrated considerable potential to enhance limb salvage rates and prevent amputations in patients with limb injuries[31]. The literature presents conflicting evidence regarding the influence of diabetes on postoperative complications following free-flap surgery for limb reconstruction. A meticulous analysis by Kantar revealed that diabetes itself is not an independent risk factor for partial or complete flap failure, as it does not directly impact flap survival[17]. Nonetheless, preoperative factors such as peripheral vascular disease, history of vascular interventions, and immunosuppression may predispose diabetic patients to an increased risk of flap loss[32]. While diabetes does not directly impair flap viability, it elevates the risk of deep incisional SSIs[19]. This increased SSI risk primarily stems from the interplay between hyperglycemia, microvascular disease, and immunosuppression, factors that can ultimately contribute to flap failure. Consequently, managing fractures in patients with diabetes necessitates careful consideration, particularly in cases with suboptimal blood glucose control. The compromised phagocytic function and diminished infection resistance in these individuals underscore the importance of judicious antibiotic use to mitigate infection risk[33].
Our findings demonstrate that placing free flaps over plate fixation hardware is a safe and reliable therapeutic option for fractures in patients with type 2 diabetes, provided the vascular pedicle is embedded within healthy soft tissue at an adequate distance from the plate. The abundant vascular network in the fascia and muscles creates a conducive environment for free-flap survival over the steel plate. To minimize nosocomial infection risk, some authors recommend wound closure within one week[34]. However, this timeframe may be inadequate for certain type IIIB fractures. In our series, all patients underwent repeated debridement and VAC to facilitate effective wound drainage and robust granulation tissue formation. After VAC removal, while the wound may superficially appear dry and fresh, it can deteriorate into a heavily contaminated state within days. Therefore, an additional waiting period of two to three days post-VAC removal was implemented to confirm the absence of fluid accumulation. Achieving dryness and vigorous granulation tissue growth is crucial for favorable outcomes with free-flap plating techniques. Establishing a safe interval after vacuum clearance is essential for success. Importantly, all patients in our cohort experienced delayed bone healing, a predictable consequence of the fractures’ initial open nature.
The theoretical underpinnings of flap coverage with the steel plate technique encompass two primary indications: Preserving exposed soft tissue defects with hardware and treating open fractures through a combined approach involving plate fixation and flap transfer. While several reports discuss these techniques collectively[35-38], we argue that using free-flap plating techniques for cases with exposed and infected internal hardware introduces greater uncertainty and higher failure risk. We acknowledge two principal limitations of our study: Its retrospective design and small sample size. Consequently, caution is necessary when expanding the application of this technique, and indications must be judiciously defined. For Gustilo type IIIB fractures, provided the wound is adequately dry, clean, and free from infection, free-flap plating yields satisfactory outcomes. This approach offers secure bone fixation, comprehensive wound coverage, ample vascular supply, and avoids inconveniences associated with prolonged EF.
This study underscores the significant potential of free-flap transfer with plate fixation for addressing Gustilo IIIB fractures in individuals with type II diabetes. Despite challenges related to postoperative infections and subsequent plate removal, consistently favorable outcomes were observed for both bone healing and flap viability. These findings provide valuable insights into managing fractures in patients with diabetes and highlight the critical importance of judicious patient selection and precise treatment criteria. Further research is needed to validate and build upon these results, ultimately enhancing the adoption and efficacy of this treatment approach in clinical practice.
The authors are grateful to the staff of the Department of Surgery, 920th Hospital of Joint Logistics Support Force of PLA and appreciate Mr. Chao Yuan from the Department of Nursing, the Second Affiliated Hospital of Zhejiang University School of Medicine for his assistance during the review process.
| 1. | Hofbauer LC, Busse B, Eastell R, Ferrari S, Frost M, Müller R, Burden AM, Rivadeneira F, Napoli N, Rauner M. Bone fragility in diabetes: novel concepts and clinical implications. Lancet Diabetes Endocrinol. 2022;10:207-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 266] [Article Influence: 66.5] [Reference Citation Analysis (0)] |
| 2. | Goldberg EM, Polachek WS, Hynes K. Ankle Fractures in Diabetic Patients: A Critical Analysis. JBJS Rev. 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 3. | Jeffcoate WJ, Price P, Harding KG; International Working Group on Wound Healing and Treatments for People with Diabetic Foot Ulcers. Wound healing and treatments for people with diabetic foot ulcers. Diabetes Metab Res Rev. 2004;20 Suppl 1:S78-S89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 143] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 4. | Wei J, Zhang L, Ding Y, Liu R, Guo Y, Hettinghouse A, Buza J, De La Croix J, Li X, Einhorn TA, Liu CJ. Progranulin promotes diabetic fracture healing in mice with type 1 diabetes. Ann N Y Acad Sci. 2020;1460:43-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Constantine RS, Le ELH, Gehring MB, Ohmes L, Iorio ML. Risk Factors for Infection After Distal Radius Fracture Fixation: Analysis of Impact on Cost of Care. J Hand Surg Glob Online. 2022;4:123-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 6. | Song W, Shibuya N, Jupiter DC. Association Between Opioid Use and Diabetes in Patients With Ankle Fracture Repair. Foot Ankle Int. 2022;43:560-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Tang Y, Kang L, Guo M, Fan L. Intertrochanteric Fracture Surgery Patients with Diabetes Mellitus are Prone to Suffer Perioperative Neurological and Endocrine/Metabolic Complications: A Propensity-Score Matched Analysis. Ther Clin Risk Manag. 2022;18:775-783. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Angan N, Feghiu B, Dumitrescu I, Feghiu V. Infected Tibial Plateau Open Reduction Internal Fixation Treated Using External Fixation and a Gastrocnemius Flap: A Case Report. Cureus. 2023;15:e46750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Gandhi A, Liporace F, Azad V, Mattie J, Lin SS. Diabetic fracture healing. Foot Ankle Clin. 2006;11:805-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Belczyk RJ, Rogers LC, Andros G, Wukich DK, Burns PR. External fixation techniques for plastic and reconstructive surgery of the diabetic foot. Clin Podiatr Med Surg. 2011;28:649-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Thomas SR, Giele H, Simpson AH. Advantages and disadvantages of pinless external fixation. Injury. 2000;31:805-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Apard T, Bigorre N, Cronier P, Duteille F, Bizot P, Massin P. Two-stage reconstruction of post-traumatic segmental tibia bone loss with nailing. Orthop Traumatol Surg Res. 2010;96:549-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 139] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 13. | Shi Z, Ou Q, Li C, Li Y, Wang B, Cheng G, Fan Y, Bao Q, Tang J. A two-stage but time-saving reconstructive scheme to treat severe lower limb length discrepancy: Two case reports. Chinese J Plast Reconstr Surg. 2023;5:68-72. [DOI] [Full Text] |
| 14. | Chaudhary SB, Liporace FA, Gandhi A, Donley BG, Pinzur MS, Lin SS. Complications of ankle fracture in patients with diabetes. J Am Acad Orthop Surg. 2008;16:159-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 97] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Kozusko SD, Liu X, Riccio CA, Chang J, Boyd LC, Kokkalis Z, Konofaos P. Selecting a free flap for soft tissue coverage in lower extremity reconstruction. Injury. 2019;50 Suppl 5:S32-S39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 66] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 16. | Graboyes EM, Hornig JD. Evolution of the anterolateral thigh free flap. Curr Opin Otolaryngol Head Neck Surg. 2017;25:416-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 17. | Kantar RS, Rifkin WJ, David JA, Cammarata MJ, Diaz-Siso JR, Levine JP, Golas AR, Ceradini DJ. Diabetes is not associated with increased rates of free flap failure: Analysis of outcomes in 6030 patients from the ACS-NSQIP database. Microsurgery. 2019;39:14-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Okonkwo UA, DiPietro LA. Diabetes and Wound Angiogenesis. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 523] [Cited by in RCA: 687] [Article Influence: 76.3] [Reference Citation Analysis (0)] |
| 19. | Martin ET, Kaye KS, Knott C, Nguyen H, Santarossa M, Evans R, Bertran E, Jaber L. Diabetes and Risk of Surgical Site Infection: A Systematic Review and Meta-analysis. Infect Control Hosp Epidemiol. 2016;37:88-99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 454] [Cited by in RCA: 435] [Article Influence: 43.5] [Reference Citation Analysis (0)] |
| 20. | Park S, Moon SW, Lee J, Kim JW. Intramedullary tibia nailing with external fixation. Eur J Trauma Emerg Surg. 2021;47:1947-1955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 21. | Ziran N, McCarty CP, Ho NC, Gilmartin NF, Ebramzadeh E, Park SH, Sangiorgio SN. A novel intramedullary nail to control interfragmentary motion in diaphyseal tibial fractures. J Orthop Res. 2022;40:1053-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Downey EA, Jaime KM, Reif TJ, Makhdom AM, Rozbruch SR, Fragomen AT. Prophylaxis and treatment of infection in long bones using an antibiotic-loaded ceramic coating with interlocking intramedullary nails. J Bone Jt Infect. 2022;7:101-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 23. | Guerado E, Cano JR, Fernandez-Sanchez F. Pin tract infection prophylaxis and treatment. Injury. 2019;50 Suppl 1:S45-S49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 24. | Ueno M, Yokoyama K, Nakamura K, Uchino M, Suzuki T, Itoman M. Early unreamed intramedullary nailing without a safety interval and simultaneous flap coverage following external fixation in type IIIB open tibial fractures: a report of four successful cases. Injury. 2006;37:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Riemer BL, Butterfield SL. Comparison of reamed and nonreamed solid core nailing of the tibial diaphysis after external fixation: a preliminary report. J Orthop Trauma. 1993;7:279-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Tielinen L, Lindahl JE, Tukiainen EJ. Acute unreamed intramedullary nailing and soft tissue reconstruction with muscle flaps for the treatment of severe open tibial shaft fractures. Injury. 2007;38:906-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Moog P, Tinwald I, Aitzetmueller M, Bauer AT, Megerle K, Machens HG, Laszlo Kovacs L, Kuekrek H. The Usage of Pedicled or Free Muscle Flaps Represents a Beneficial Approach for Periprosthetic Infection After Knee Arthroplasty. Ann Plast Surg. 2020;85:539-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Altam A, Alsaaidi A, Aljbri W, Ahmed F, Al-Wageeh S, Alyhari Q, Nasr B, Al-Naggar A, Badheeb M, Al-Shami E. Role of microsurgical free flap reconstruction in managing complex wound: a retrospective cross-sectional study. Pan Afr Med J. 2022;43:211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Barr LC, Joyce AD. Microvascular anastomoses in diabetes: an experimental study. Br J Plast Surg. 1989;42:50-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Goldenberg S, Alex M, Joshi RA, Blumenthal HT. Nonatheromatous peripheral vascular disease of the lower extremity in diabetes mellitus. Diabetes. 1959;8:261-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 172] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 31. | Ducic I, Attinger CE. Foot and ankle reconstruction: pedicled muscle flaps versus free flaps and the role of diabetes. Plast Reconstr Surg. 2011;128:173-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 32. | Oh TS, Lee HS, Hong JP. Diabetic foot reconstruction using free flaps increases 5-year-survival rate. J Plast Reconstr Aesthet Surg. 2013;66:243-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 33. | Lecube A, Pachón G, Petriz J, Hernández C, Simó R. Phagocytic activity is impaired in type 2 diabetes mellitus and increases after metabolic improvement. PLoS One. 2011;6:e23366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 154] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 34. | Gopal S, Majumder S, Batchelor AG, Knight SL, De Boer P, Smith RM. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br. 2000;82:959-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 263] [Reference Citation Analysis (0)] |
| 35. | Berkes M, Obremskey WT, Scannell B, Ellington JK, Hymes RA, Bosse M; Southeast Fracture Consortium. Maintenance of hardware after early postoperative infection following fracture internal fixation. J Bone Joint Surg Am. 2010;92:823-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 147] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 36. | Ovaska MT, Madanat R, Tukiainen E, Pulliainen L, Sintonen H, Mäkinen TJ. Flap reconstruction for soft-tissue defects with exposed hardware following deep infection after internal fixation of ankle fractures. Injury. 2014;45:2029-2034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | Viol A, Pradka SP, Baumeister SP, Wang D, Moyer KE, Zura RD, Olson SA, Zenn MR, Levin SL, Erdmann D. Soft-tissue defects and exposed hardware: a review of indications for soft-tissue reconstruction and hardware preservation. Plast Reconstr Surg. 2009;123:1256-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 38. | Zhao Y, Qi BW, Wang YQ, Liu D, Chen F, Huang Z, Pan ZY. Hardware removal or preservation? Decision making based on a newly developed rating scale. Injury. 2018;49:1999-2004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/