Published online Sep 6, 2025. doi: 10.12998/wjcc.v13.i25.108244
Revised: April 25, 2025
Accepted: May 27, 2025
Published online: September 6, 2025
Processing time: 88 Days and 22.3 Hours
Restless legs syndrome (RLS) is a neurological disorder characterized by an uncontrollable urge to move the legs during rest. Standard treatments may provide short-term relief but are limited by long-term adverse effects. Herbal medicine containing Paeoniae Radix (HCP) has traditionally been used in Korean medicine to treat RLS symptoms.
To investigate the clinical effectiveness and safety of HCP in treating RLS.
This retrospective chart review study included 15 patients with RLS who were treated with HCP between September 2017 and August 2022 at the Kyung Hee University Korean Medicine Hospital. The demographic, disease-related, and treatment-related characteristics, as well as the impressions of each patient, were analyzed. The study also evaluated the changes in the subjective complaints of RLS symptoms, the Korean version of the International Restless Legs Scale (K-IRLS) scores before and after treatment, and the adverse events after HCP administration.
Following HCP administration, 14 patients (93.3%) experienced a decrease in the degree of discomfort associated with their symptoms, with an average reduction to 44.7 ± 35.1% compared to their discomfort levels before taking the drug. After treatment, the mean total K-IRLS score decreased significantly from 23.00 ± 9.75 to 13.93 ± 10.9 (P = 0.005). Among the HCP, a significant reduction in the K-IRLS score was observed in the Gyejibokryeonghwan (26.0 ± 9.7 to 10.0 ± 9.4, P = 0.028) and Jakyakgamchotang (23.2 ± 12.6 to 6.6 ± 4.2, P = 0.042) groups. Additionally, no adverse events were reported.
HCP improved symptoms in RLS patients. These results suggest that HCP may be an effective and safe alternative for RLS. A randomized controlled trial is required to confirm these findings.
Core Tip: Restless legs syndrome (RLS) is a chronic condition, but is difficult to manage due to the limitations associated with the long-term use of conventional treatments. This retrospective chart review study demonstrated that herbal medicine containing Paeoniae Radix (HCP) effectively and safely alleviated RLS symptoms. HCP may serve as a promising alternative therapy for patients with RLS. These findings highlight the potential role of herbal medicine in RLS management.
- Citation: Lee YS, Lee HG, Kwon S, Cho SY, Jung WS, Park SU, Moon SK, Park JM, Ko CN. Effects of herbal medicines containing Paeoniae Radix on patients with restless legs syndrome: A retrospective chart review study. World J Clin Cases 2025; 13(25): 108244
- URL: https://www.wjgnet.com/2307-8960/full/v13/i25/108244.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i25.108244
Restless legs syndrome (RLS) is a sensorimotor neurological disorder characterized clinically by an urge to move legs during a resting state that is often difficult to control, and these symptoms are relieved by movement. RLS worsens at night, causing sleep disturbance[1]. Moreover, RLS is referred to as Willis–Ekbom disease as Willis first reported the phenomenon in 1672 and Karl Ekbom described the clinical manifestations of RLS in 1945[2]. The prevalence of RLS ranges from 5%-15% worldwide and varies by race and country[3], with a prevalence of 7.2% in the United States[4], and 1.3%-8.3% in South Korea[5,6]. Despite that the condition is relatively common, RLS is rarely diagnosed owing to low awareness of the disease, with only 16% of patients receiving appropriate treatment[7].
Moreover, the clinical efficacy of dopamine in alleviating RLS symptoms, the exacerbation of symptoms by dopamine antagonists, and the correlation between diurnal fluctuations in dopamine levels and the onset and aggravation of RLS symptoms support the role of dopamine in the pathophysiology of RLS[8]. Therapeutic agents for RLS include anticonvulsants, dopamine agonists, benzodiazepines, opiates, and iron[9]. Dopamine agonists, while providing rapid and effective initial symptomatic relief, may lead to augmentation with long-term use (6 months or more), making them less suitable for the chronic nature of RLS, which requires long-term management[10]. Therefore, alternative treatments for RLS are required.
In Korean medicine, which is one of the Traditional East Asian Medicines, herbal medicine is used to treat RLS, and its effectiveness is becoming increasingly recognized[11]. Among them, herbal medicines containing Paeoniae Radix (HCP) accounted for the largest proportion. A previous case report reported successful treatment of chronic RLS symptoms with HCP[12]. Additionally, treatment with HCP alone or in combination with Western medicine had significantly better symptomatic effects than those observed with Western medicine alone[13]. Paeoniflorin, the main component in Paeoniae Radix, has been reported to acts as an activator of the adenosine A1 receptor (A1R) and is responsible for slowing and stabilizing brain metabolism by reducing synaptic discharge[14]. In this study, we aimed to verify the clinical potential of HCP as a treatment for RLS using quantitative evaluation and statistical validation through retrospective chart review to determine the actual treatment effect of HCPs on patients with RLS.
Between September 2017 and August 2022, 15 patients (male: 3, female: 12) were recruited from the Stroke and Brain Disease Center of Kyung Hee University Korean Medicine Hospital, Seoul, Republic of Korea. The inclusion criteria were as follows: Patients diagnosed with RLS according to the International Restless Legs Syndrome Study Group criteria, patients prescribed HCP for the treatment of RLS symptoms, and patients who completed the Korean version of the International Restless Legs Scale (K-IRLS) before and after consuming HCP. The exclusion criteria were as follows: Patients with unclear medication adherence regarding HCP, and patients who were not followed up within 15 days of starting HCP treatment.
The study protocol was approved by the Institutional Review Board of Kyung Hee University Korean Medicine Hospital (KOMCIRB 2023-01-005, approved on February 27, 2023). Additionally, the study was conducted in accordance with the guidelines of the Declaration of Helsinki.
Characteristics of participants: The sex, age, disease-related characteristics (diagnosis, symptoms, onset, medical history, medication information, and surgical history), and HCP-associated details (type, dosage, and duration) of the study participants were investigated.
Change in subjective complaints of RLS symptoms before and after administration: At the initial visit, the degree of discomfort due to RLS symptoms, including sleep disturbance, was considered 100, and the degree of improvement from the first visit to the subsequent visit was expressed as a percentage. If the patient was unable to quantify their improvement numerically by at least 10%, we categorized it as "improved" and considered it a 10% improvement.
K-IRLS: We used the K-IRLS[15], a Korean translation of the original scale developed by the International Restless Legs Syndrome Study Group, to assess the changes in RLS symptoms. The scale consists of 10 questions, each scored from 0 to 4 points for each item. Furthermore, the scores of the 10 items are summed, with high scores indicating higher severity. The total score was 40 points, and severity was categorized into four levels: 0-10, mild; 11-20, moderate; 21-30, severe; and 31-40, very severe. The score included an assessment of the main symptoms of RLS, their severity and frequency, their relationship with sleep disturbances, and their impact on the mood and daytime functioning of patients. The K-IRLS results were collected at the initial visit and follow-up tests were conducted at subsequent visits.
Adverse events: The presence and types of adverse events reported by the patients after HCP administration were investigated using medical records.
Statistical analyses were performed using the SPSS for Windows version 25. The Wilcoxon signed-rank test was used to examine whether the changes in subjective discomfort and K-IRLS scores before and after HCP administration were significant. All data were expressed as mean ± standard deviation (SD) or as a number (%). In the study, the statistical significance was defined as P < 0.05 for all analyses.
The participants comprised 12 (80.0%) females and three (20.0%) males, with an average age of 60.6 years. The majority of patients reported experiencing symptoms for more than 5 years but less than 10 years, accounting for 33.3% of the sample. This was followed by 26.6% of patients who reported experiencing symptoms for less than 1 year. Five patients used a combination of HCP and conventional Western medicine during treatment (two with iron and four with dopamine agents). Five patients underwent a blood test for iron-deficiency anemia before starting treatment, and all results were within the normal range. The average duration of HCP administration was 58.4 ± 46.1 (Table 1). The HCPs used were Jakyakgamchotang (Shakuyakukanzoto in Japanese, Shaoyao Gancao Tang in Chinese), Gyejibokryeonghwan (Keishibukuryogan in Japanese, Guizhi Fuling Hwan in Chinese), Gamisoyosan (Kamishoyosan in Japanese, Jiawei Xiaoyao San in Chinese), Sihogyejitang (Saikokeishito in Japanese, Chaihu Guizhi Tang in Chinese), Dangguijakyaksan (Tokishakuyakusan in Japanese, Danggui Shaoyao San in Chinese), Danggwisayeokgaohsuyusaenggangtang (Tokishigyakukagoshuyushokyoto in Japanese, Danggui Sini Jia Wuzhuyu Shengjiang Tang in Chinese) and all the prescriptions were in the form of extracts formula. Seven participants (46.7%) were administered two or more HCPs, with Gyejibokryeonghwan being the most commonly administered HCP (seven cases, 46.7%), followed by Jakyakgamchotang (five cases, 33.3%) (Table 2, Supplementary Table 1).
| General characteristics | Number of patients (%) | |
| Sex | Male | 3 (20.0) |
| Female | 12 (80.0) | |
| Age | 20s | 1 (6.6) |
| 30s | 0 (0) | |
| 40s | 3 (20.0) | |
| 50s | 0 (0) | |
| 60s | 7 (46.6) | |
| 70s | 4 (26.6) | |
| Duration of symptom | Less than 1 year | 3 (20.0) |
| 1-3 years | 2 (13.2) | |
| 3-5 years | 1 (6.6) | |
| 5-10 years | 5 (33.3) | |
| More than 10 years | 3 (20.0) | |
| Undetermined | 1 (6.6) | |
| Symptom site | Sole | 3 (20.0) |
| Thigh | 5 (33.3) | |
| Calves | 8 (53.3) | |
| Ankle | 6 (40.0) | |
| Knee | 1 (6.6) | |
| Feet | 1 (6.6) | |
| History | Hypertension | 6 (40.0) |
| Parkinson’s disease | 1 (6.6) | |
| Dyslipidemia | 4 (26.6) | |
| Iron deficiency anemia | 1 (6.6) | |
| Cardiovascular disease | 3 (20.0) | |
| Spinal stenosis | 2 (13.2) | |
| Lung disease | 1 (6.6) | |
| HIVD of L-Spine | 2 (19.8) | |
| Gynecological disease | 2 (13.2) | |
| Chronic kidney disease | 1 (6.6) | |
| HCP administrating duration | 2-4 weeks | 4 (26.7) |
| 4-6 weeks | 5 (33.3) | |
| More than 6 weeks | 6 (40.0) |
| Case | Age/Sex | Intervention/HCP use period | History | RLS duration/site | Other treatment | K-IRLS before and after treatment/Patient’s complaint after treatment | Adverse events |
| P1 | 68/F | Gyejibokryeonghwan/2P#2 51 days, 1P#1 85 days | Atherosclerosis, HTN, spinal stenosis | 2 weeks/sole | None | K-IRLS: Total: Before 12 after 6; Urge to move: before 2 after 0; Duration; before 3 after 1; 0% of symptoms compared to pre-treatment, only noticeable when aware of symptoms | None |
| P2 | 48/F | Gamisoyosan/3P#3 140 days | Uterine myoma | 2 years/calves, ankle | None | K-IRLS: Total: Before 19 after 13; Urge to move: before 3 after 1; Severity: Before 3 after 1; 40% of symptoms compared to pre-treatment; Frequency decreased to once a week | None |
| P3 | 23/F | Dangguijakyaksan/2P#2 84 days | Nonspecific | 6 years/thigh | None | K-IRLS: Total: Before 22 after 9; Discomfort: Before 3 after 2; Frequency: Before 3 after 1; 20% of symptoms compared to pre-treatment; Declined symptoms severity and occurrence from 4-5 times a week to once a week after treatment | None |
| P4 | 73/F | Gyejibokryeonghwan Gamisoyosan/both 2P#2 28 days | HTN, dyslipidemia, HIVD of L-Spine | 12 years/sole | Dopamine agonist (Pramipexole) | K-IRLS: Total: Before 35 after 21; Discomfort: Before 4 after 2; Urge to move: Before 4 after 2; Severity: Before 4 after 2; Relief from movement: Before 4 after 2; 70% of symptoms compared to pre-treatment, especially sleep disorder | None |
| P5 | 62/M | Jakyakgamchotang Gyejibokryeonghwan/both 1P#1 15 days | Nonspecific | 8 years/calves, thigh, knee | None | K-IRLS: Total: Before 24 after 10; Discomfort: Before 3 after 1; Urge to move: Before 3 after 1; Frequency: Before 4 after 1; 30% of symptoms compared to pre-treatment, especially daytime tiredness | None |
| P6 | 68/F | Gyejibokryeonghwan/3P#3 14 days 2P#2 28 days, 1P#1 42 days; Dangguijakyaksan 1P#1/1P#1 30 days | HTN, dyslipidemia | 4 years/sole | Dopamine agonists (Levodopa, Ropinirole hydrochloride) | K-IRLS: Total: Before 18 after 0; Discomfort: Before 2 after 0; Urge to move: Before 2 after 0; Frequency: Before 3 after 0; 0% of symptoms compared to pre-treatment | None |
| P7 | 60/F | Jakyakgamchotang 2P#2; Gyejibokryeonghwan 1P#1/113 days | HTN, dyslipidemia, asthma, HIVD of L-Spine | 6 months/calves, ankle | Iron supplements (Iron acetyltransferrin) | K-IRLS: Total: Before 40 after 0; 0% of symptoms compared to pre-treatment | None |
| P8 | 70/F | Jakyakgamchotang 2P#2/35 days; Gyejibokryeonghwan 3P#3/35 days; Sihogyejitang 3P#3/28 days | Meningioma, angina pectoris | Unknown/calves, ankle, sole | None | K-IRLS: Total: Before 30 after 9; Discomfort: Before 4 after 1; Urge to move: before 4 after 1; Severity: Before 4 after 1; 50% of symptoms compared to pre-treatment, especially sleep disorder | None |
| P9 | 44/M | Gamisoyosan/2P#2 28 days | Nonspecific | 8 years/calves | None | K-IRLS: Total: Before 16 after 14; Discomfort: Before 2 after 1; Urge to move: Before 2 after 1; 20% of symptoms compared to pre-treatment; especially sleep disorder | None |
| P10 | 43/F | Dangguijakyaksan Sihogyejitang/both 2P#2 30 days | CKD | 7 years/calves, thigh, feet | GABA (Pregabalin); Iron supplements (Iron acetyltransferrin) Benzodiazepines (Clonazepam) | K-IRLS: Total: Before 37 after 36; 80% of symptoms compared to pre-treatment; even after the Pregabalin administration was stopped. Symptom frequency and duration were prolonged | None |
| P11 | 71/F | Sihogyejitang Danggwisayeokgaohsuyusaenggangtang Gyejibokryeonghwan/all 2P#2 14 days | HTN, dyslipidemia, spinal stenosis, iron deficiency anemia | 10 years / ankle | Iron supplements (Dried ferrous sulfate); Benzodiazepines (Clonazepam); Dopamine agonist (Pramipexole) | K-IRLS: Total: Before 23 after 24; Discomfort: Before 4 after 3; Urge to move: before 4 after 2; 70% of symptoms compared to pre-treatment | None |
| P12 | 69/M | Jakyakgamchotang/1P#1 84 days | HTN, BPH | 1 month/thigh | None | K-IRLS: Total: Before 9 after 5; Discomfort: Before 2 after 1; Sleep disorder: Before 2 after 0; 60% of symptoms compared to pre-treatment, the frequency of symptoms occurrence decreased to once a week after treatment; Increased quality of sleep time | None |
| P13 | 68/F | Dangguijakyaksan/2P#2 14 days | Nonspecific | 50 years/calves, thigh, ankle | None | K-IRLS: Total: Before 32 after 34; Urge to move: before 4 after 3; Sleep disorder: Before 4 after 3; No change of symptoms | None |
| P14 | 74/F | Danggwisayeokgaohsuyusaenggangtang /2P#2 14 days | Nonspecific | 10 years/calves | None | K-IRLS: Total: Before 15 after 19; 90% of symptoms compared to pre-treatment | None |
| P15 | 60/F | Jakyakgamchotang/1P#1 14 days | Parkinson’s disease | 1 year/ankle | Dopamine agonists (Pramipexole, Rasagiline); NSAIDs (Naproxen, Celecoxib) | K-IRLS: Total: Before 13 after 9; Severity: Before 2 after 0; Frequency before 2 after 0; 90% of symptoms compared to pre-treatment; Reduced RLS symptom duration from 1 hour to less than 1 minute | None |
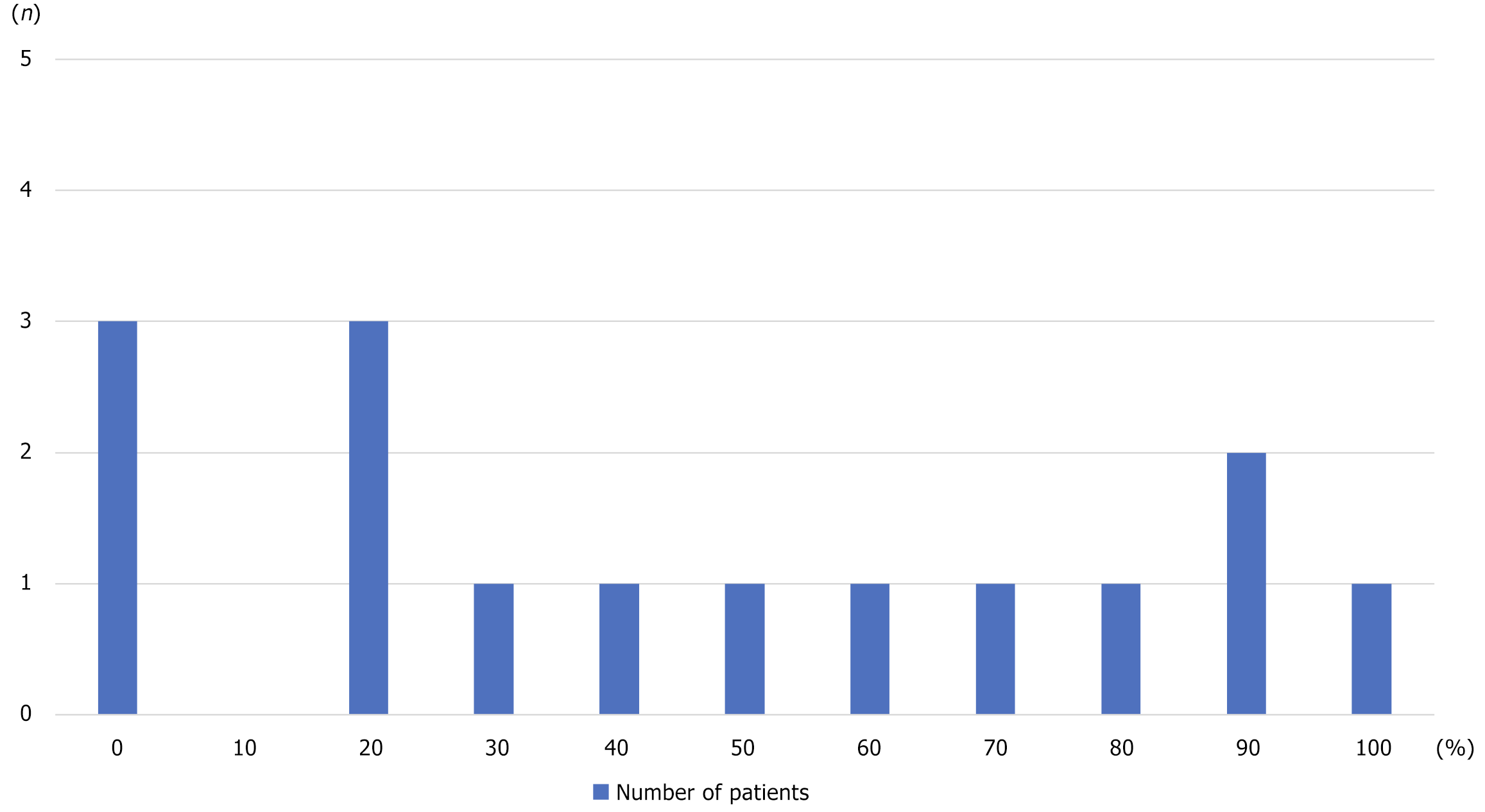
Subjective complaints decreased in 14 (93.3%) patients after HCP administration compared to their pre-treatment condition, with a mean reduction of 44.7 ± 35.1%. The most common improvements were observed in patients whose complaints decreased from 100% to 10% or less, and from 20% or more, each accounting for three patients (20.0%) (Figure 1). Detailed clinical information and outcomes of the patients are presented in Table 2.
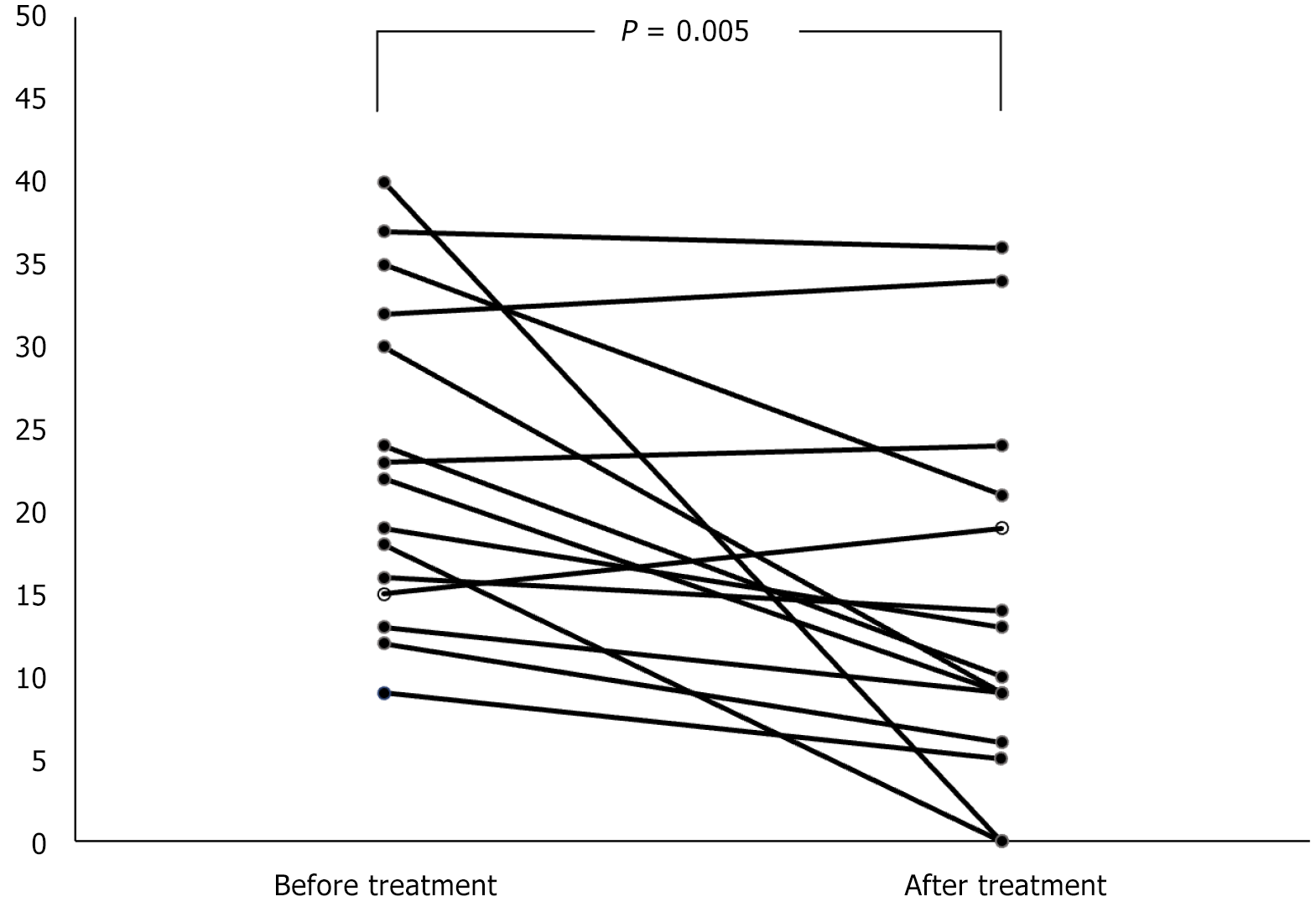
After HCP administration, the total K-IRLS score decreased significantly from 23.0 ± 9.7 to 13.9 ± 10.9 (P = 0.005). The scores improved in all 10 items, and among them, discomfort (2.6 ± 1.2 to 1.6 ± 1.1, P < 0.033), urge to move (2.8 ± 1.1 to 1.3 ± 1.1, P = 0.002), frequency (3.0 ± 0.9 to 1.6 ± 1.4, P = 0.007), severity (2.8 ± 1.0 to 1.2 ± 1.3, P = 0. 003), duration (2.4 ± 1.1 to 1.6 ± 1.1, P = 0.033), and effect on daily affairs (1.8 ± 1.5 to 0.8 ± 1.1, P = 0.035) significantly decreased. The scores of all other items also decreased; however, the decrease was not statistically significant (Table 3, Figure 2). When comparing K-IRLS changes based on HCP type, a significant decrease was observed in the scores in the Gyejibokryeonghwan (26.0 ± 9.7 to 10.0 ± 9.4, P = 0.028) and Jakyakgamchotang (23.2 ± 12.6 to 6.6 ± 4.2, P = 0.042) treatment groups. However, no significant difference in the respective non-administration groups was observed. Additionally, no significant differences were noted in the scores of the other HCPs in the administration group (Table 4).
| K-IRLS | Baseline | After treatment | P value |
| Total score | 23.0 ± 9.7 | 13.9 ± 10.9 | 0.0051 |
| Discomfort | 2.6 ± 1.2 | 1.6 ± 1.1 | 0.0331 |
| Urge to move | 2.8 ± 1.1 | 1.3 ± 1.1 | 0.0021 |
| Relief from movement | 2.2 ± 1.3 | 1.6 ± 1.2 | 0.168 |
| Sleep disorder | 2.2 ± 1.3 | 1.6 ± 1.4 | 0.071 |
| Day time tiredness | 1.3 ± 1.4 | 1.0 ± 1.2 | 0.632 |
| Severity | 2.8 ± 1.0 | 1.2 ± 1.3 | 0.0031 |
| Frequency | 3.0 ± 0.9 | 1.6 ± 1.4 | 0.0071 |
| Duration | 2.4 ± 1.1 | 1.6 ± 1.4 | 0.0331 |
| Effect on daily affairs | 1.8 ± 1.5 | 0.8 ± 1.1 | 0.0351 |
| Mood disturbance | 1.4 ± 1.4 | 1.0 ± 1.2 | 0.305 |
| HCP | Administration group | ||
| Baseline | After treatment | P value | |
| Gyejibokryeonghwan (n = 7) | 26.0 ± 9.7 | 10.0 ± 9.4 | 0.0281 |
| Jakyakgamchotang (n = 5) | 23.2 ± 12.6 | 6.6 ± 4.2 | 0.0421 |
| Sihogyejitang (n = 3) | 30.0 ± 7.0 | 23.0 ± 13.5 | 0.414 |
| Dangguijakyaksan (n = 4) | 27.3 ± 8.8 | 19.8 ± 18.0 | 0.273 |
| Danggwisayeokgaohsuyusaenggangtang (n = 2) | 19.0 ± 5.7 | 21.5 ± 3.5 | 0.180 |
| Gamisoyosan (n = 3) | 23.3 ± 10.2 | 16.0 ± 4.4 | 0.109 |
No adverse events were reported since the administration of HCP.
In this retrospective observational study, patients with RLS who took HCPs demonstrated improvement in subjective symptoms as well as significant improvement in K-IRLS scores compared to their pre-treatment conditions. Specifically, significant improvements were observed in six of the 10 K-IRLS items, including discomfort, urge to move, severity, frequency, duration, and effect on daily affairs.
The hypothesis of dopamine hypofunction is supported as a possible pathogenesis of RLS[16]. Reduced iron, which is essential for the activation of tyrosine hydroxylase, the rate-determining step in dopamine synthesis, can lead to decreased dopamine activity, consequently resulting in RLS[8]. Reduced iron is stored in the brain and dysfunction of dopaminergic neurons may be associated with decreased function of hepatic dopamine cell A11, which regulates sensory, motor, and sympathetic nerve activity[17].
Paeoniflorin, one of the main constituents of Paeoniae Radix, has been reported to act as an activator of the A1R, which is responsible for inhibiting the activation of synaptic transmission and thus reducing metabolism in the brain[18]. In an experimental study, iron-deficient diets were discovered to lower the activity of A1R and dopamine D2 receptors, suggesting that A1R activity could serve as an indicator of iron stores in the brain[19]. Based on this evidence, it can be hypothesized that paeoniflorin induced dopaminergic activity through the activation of A1R function, which restored the function of brainstem A11 dopamine neurons and relieved RLS symptoms.
Of the HCPs used in this study, all six cases of Gyejibokryeonghwan and five cases of Jakyakgamchotang demon
Gyejibokryeonghwan has been reported to have anti-inflammatory effects[20] and it prevents nitric oxide-induced neuronal death in cerebellar granule cells[21]. Therefore, it was speculated that Gyejibokryeonghwan alleviated leg discomfort through anti-inflammatory, neuroprotective, and analgesic effects. Jakyakgamchotang inhibits inflammation by modulating the production of various pro-inflammatory cytokines in the body[22] and has been implicated in the regulation of the dopaminergic nervous system[23]. Dangguijakyaksan activates the synthesis of acetylcholine and norepinephrine and improves the central cholinergic nervous system[24], as well as inhibits beta-amyloid-induced neuronal damage[25]. Sihogyejitang is a combination of soshihotang and gyejitang, of which soshihotang has been reported to exert antidepressant effects by increasing the level of monoamine neurotransmitters[26]. The enhanced peripheral blood flow recovery and increased skin temperature[27], observed with Danggwisayeokgaohsuyusaenggangtang suggest its potential efficacy, particularly in patients with RLS experiencing lower extremity coldness.
This study has several limitations. First, it was a retrospective, single-arm observational study that lacked comparative validation with a control group, which may have led to biased interpretation. Second, a small number of patients required non-parametric tests. To increase the statistical power, analyzing symptom changes before and after taking HCPs in a large number of patients is necessary. Third, since all prescribed HCPs with varied duration treatment were included in the analysis, multiple herbal medicines with different treatment periods were utilized, which may have significantly complicated the interpretation of treatment effects. Verifying the effectiveness of each herbal medicine used in this study is necessary, such as Gyejibokryeonghwan and Jakyakgamchotang, which presented high frequency and favorable effects. Fourth, the relatively short duration of treatment, with more than half of the treatments lasting less than six weeks, requires cautious interpretation of the safety of HCPs in this study. Fifth, this study lacks correction for multiple comparisons which may cause the risk of Type I error. Since this study was exploratory in nature, correction for multiple comparisons was not applied despite the risk of Type I error, as correction for multiple comparisons would increase the risk of Type II error and may obscure potentially meaningful results that warrant further investigation. Therefore, based on the results of this study, designing a large-scale prospective randomized controlled trial with controlled intervention, treatment duration, and follow-up period to further strengthen the evidence for the effectiveness of herbal medicines for RLS presented in this study is necessary.
HCP significantly improved subjective discomfort and K-IRLS scores in patients with RLS. Among the HCPs, Gyejibokryeonghwan and Jakyakgamchotang were the most effective. We recommend that HCP is effective in improving RLS symptoms; therefore, HCP has the potential to be an alternative treatment for RLS.
This manuscript was written based on Young Seon Lee’s thesis for a master’s degree at Kyung Hee University in 2023.
| 1. | Trenkwalder C, Paulus W. Restless legs syndrome: pathophysiology, clinical presentation and management. Nat Rev Neurol. 2010;6:337-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 211] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 2. | Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, Zucconi M, Ferri R, Trenkwalder C, Lee HB; International Restless Legs Syndrome Study Group. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria--history, rationale, description, and significance. Sleep Med. 2014;15:860-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1325] [Cited by in RCA: 1098] [Article Influence: 91.5] [Reference Citation Analysis (1)] |
| 3. | O'Regan D, Anderson KN. Restless legs syndrome and periodic limb movements of sleep. Br J Hosp Med (Lond). 2020;81:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Allen RP, Bharmal M, Calloway M. Prevalence and disease burden of primary restless legs syndrome: results of a general population survey in the United States. Mov Disord. 2011;26:114-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 166] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 5. | Kim KW, Yoon IY, Chung S, Shin YK, Lee SB, Choi EA, Park JH, Kim JM. Prevalence, comorbidities and risk factors of restless legs syndrome in the Korean elderly population - results from the Korean Longitudinal Study on Health and Aging. J Sleep Res. 2010;19:87-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Kim TJ, Yoon JE, Park JA, Lee SK, Chu MK, Yang KI, Kim WJ, Park SH, Thomas RJ, Shin C, Yun CH. Prevalence and Characteristics of Restless Legs Syndrome in Korean Adults: A Study in Two Independent Samples of the General Population. Neuroepidemiology. 2019;52:193-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Cho YW, Shin WC, Yun CH, Hong SB, Kim JH, Allen RP, Earley CJ. Epidemiology of restless legs syndrome in Korean adults. Sleep. 2008;31:219-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 97] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Gossard TR, Trotti LM, Videnovic A, St Louis EK. Restless Legs Syndrome: Contemporary Diagnosis and Treatment. Neurotherapeutics. 2021;18:140-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 117] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 9. | Kang S. Updates on the Diagnosis and Treatment of Restless Legs Syndrome. J Korean Neuropsychiatr Assoc. 2020;59:13. [DOI] [Full Text] |
| 10. | Kurlan R, Rabin M. Augmentation in restless legs syndrome: poor response to sudden withdrawal of dopaminergic therapy. JPRLS. 2013;3:49-52. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Lee Y, Lee J, Kim S, Yoo J. The Study on Effect of Korean Medical Treatment for Patients with Restless Legs Syndrome. JON. 2015;26:357-364. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Lee HG, Kwon S, Goto H, Fujimoto M, Kainuma M, Cho KH. Successful treatment of restless legs syndrome accompanied by headaches for 30 years with herbal prescriptions containing Paeoniae Radix: A case report. Explore (NY). 2024;20:103003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Kwon S, Jin C, Cho SY, Park SU, Jung WS, Moon SK, Park JM, Ko CN, Cho KH. Paeoniae Radix-containing herbal medicine for patients with restless legs syndrome: A systematic review and meta-analysis. Complement Ther Clin Pract. 2019;35:329-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Liu DZ, Xie KQ, Ji XQ, Ye Y, Jiang CL, Zhu XZ. Neuroprotective effect of paeoniflorin on cerebral ischemic rat by activating adenosine A1 receptor in a manner different from its classical agonists. Br J Pharmacol. 2005;146:604-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 105] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 15. | Yang JG, Kim DH, Lee JB, Park KH, Jung KY, Shin WC. The reliability and validity of the Korean versions of the international restless legs scale and the restless legs syndrome quality of life questionnaire. J Korean Neurol Assoc. 2010;28:263-269. |
| 16. | Earley CJ, Kuwabara H, Wong DF, Gamaldo C, Salas R, Brasic J, Ravert HT, Dannals RF, Allen RP. The dopamine transporter is decreased in the striatum of subjects with restless legs syndrome. Sleep. 2011;34:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 107] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Clemens S, Rye D, Hochman S. Restless legs syndrome: revisiting the dopamine hypothesis from the spinal cord perspective. Neurology. 2006;67:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 339] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 18. | Ferré S, Quiroz C, Guitart X, Rea W, Seyedian A, Moreno E, Casadó-Anguera V, Díaz-Ríos M, Casadó V, Clemens S, Allen RP, Earley CJ, García-Borreguero D. Pivotal Role of Adenosine Neurotransmission in Restless Legs Syndrome. Front Neurosci. 2017;11:722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (1)] |
| 19. | Quiroz C, Gulyani S, Ruiqian W, Bonaventura J, Cutler R, Pearson V, Allen RP, Earley CJ, Mattson MP, Ferré S. Adenosine receptors as markers of brain iron deficiency: Implications for Restless Legs Syndrome. Neuropharmacology. 2016;111:160-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Yoshihisa Y, Furuichi M, Ur Rehman M, Ueda C, Makino T, Shimizu T. The traditional Japanese formula keishibukuryogan inhibits the production of inflammatory cytokines by dermal endothelial cells. Mediators Inflamm. 2010;2010:804298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Shimada Y, Yokoyama K, Goto H, Sekiya N, Mantani N, Tahara E, Hikiami H, Terasawa K. Protective effect of keishi-bukuryo-gan and its constituent medicinal plants against nitric oxide donor-induced neuronal death in cultured cerebellar granule cells. Phytomedicine. 2004;11:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Kim BW. Anti-inflammatory effect of Jakyakgamcho-tang. J Int Korean Med. 2010;31:177-183. |
| 23. | Wang D, Wang W, Zhou Y, Wang J, Jia D, Wong HK, Zhang ZJ. Studies on the regulatory effect of Peony-Glycyrrhiza Decoction on prolactin hyperactivity and underlying mechanism in hyperprolactinemia rat model. Neurosci Lett. 2015;606:60-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Toriizuka K, Hou P, Yabe T, Iijima K, Hanawa T, Cyong JC. Effects of Kampo medicine, Toki-shakuyaku-san (Tang-Kuei-Shao-Yao-San), on choline acetyltransferase activity and norepinephrine contents in brain regions, and mitogenic activity of splenic lymphocytes in ovariectomized mice. J Ethnopharmacol. 2000;71:133-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Egashira N, Iwasaki K, Akiyoshi Y, Takagaki Y, Hatip-Al-Khatib I, Mishima K, Kurauchi K, Ikeda T, Fujiwara M. Protective effect of Toki-shakuyaku-san on amyloid beta25-35-induced neuronal damage in cultured rat cortical neurons. Phytother Res. 2005;19:450-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Ma J, Wu CF, Wang F, Yang JY, Dong YX, Su GY, Zhang K, Wang ZQ, Xu LW, Pan X, Zhou TS, Ma P, Song SJ. Neurological mechanism of Xiaochaihutang's antidepressant-like effects to socially isolated adult rats. J Pharm Pharmacol. 2016;68:1340-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Tsukada R, Yamaguchi T, Hang L, Iseki M, Kobayashi H, Inada E. Effects of a Traditional Japanese Medicine Goshajinkigan, Tokishigyakukagoshuyushokyoto on the Warm and Cold Sense Threshold and Peripheral Blood Flow. Health. 2014;06:757-763. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/