Published online Feb 26, 2024. doi: 10.12998/wjcc.v12.i6.1130
Peer-review started: October 1, 2023
First decision: January 2, 2024
Revised: January 10, 2024
Accepted: January 30, 2024
Article in press: January 30, 2024
Published online: February 26, 2024
Processing time: 141 Days and 23.5 Hours
Simple bone cysts (SBC) are benign tumor-like bone lesions typically identified in children. While SBC may lead to growth disturbances or growth arrest, such cases are uncommon. The mechanisms behind these observations remain unclear. Addi
Here, we present our experience in the successful surgical management of a 10-year-old girl with SBC, who presented with a pathological fracture complicated by malunion of the displaced fracture, varus deformity, and limb length discre
As per current literature, acute correction of acute angular deformity in proximal humeral SBC is not well comprehended. However, in this specific case, acute correction was considered an optimal solution.
Core Tip: We successfully operated on a 10-year-old girl with simple bone cysts (SBC), who presented with varus deformity, limb length discrepancy, and malunion resulting from a neglected pathological fracture. We proposed two potential causes for the humeral growth arrest and varus deformity in this patient: (1) Direct disruption of the physis by fluid from the cyst itself; and (2) damage to the epiphysis due to recurrent pathological fractures associated with SBC. Presently, the literature lacks a comprehensive understanding of the acute correction of angular deformity in proximal humeral SBC. However, in this specific case, acute correction was considered an ideal option.
- Citation: Lin CS, Lin SM, Rwei SP, Chen CW, Lan TY. Simple bone cysts of the proximal humerus presented with limb length discrepancy: A case report. World J Clin Cases 2024; 12(6): 1130-1137
- URL: https://www.wjgnet.com/2307-8960/full/v12/i6/1130.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i6.1130
Simple bone cysts (SBC), also known as solitary bone cysts are benign, fluid-filled tumor-like bone lesions commonly found in the proximal humerus (70%) or femur (25%) of children and adolescents[1,2]. While SBC may occasionally result in growth disturbances or growth arrest, such cases are uncommon. The underlying mechanisms behind this remain un
A 10-year-old Chinese girl presented at our orthopedics clinic with a history of restricted left shoulder elevation and left upper limb length discrepancy spanning six months.
The patient experienced difficulty lifting her left arm during undressing, leading her mother to observe a noticeable length difference in the left arm. Concerned about these issues, the mother brought her to our clinic for evaluation.
The patient had no pre-existing medical conditions. No history of trauma, fever, local infection, or other precipitating factors in the left shoulder were noted.
The patient's mother denied any family history of tumors.
During physical examination, it was observed that the patient’s left arm was approximately 4-5 cm shorter than the right. The active range of motion (ROM) for the left shoulder was limited due to pain (Table 1). However, the distal circulation was found to be intact, and no focal neurological signs or symptoms were observed.
| Preoperative active ROM | Postoperative-1 month active ROM | Postoperative-1 year active ROM | |
| Flexion | 70 | 176 | 180 |
| Abduction | 80 | 175 | 180 |
| External rotation | 45 | 90 | 95 |
| Internal rotation | 10 | 65 | 75 |
Serum C-reactive protein levels were within the normal range, and routine blood and urine analyses showed no abnor
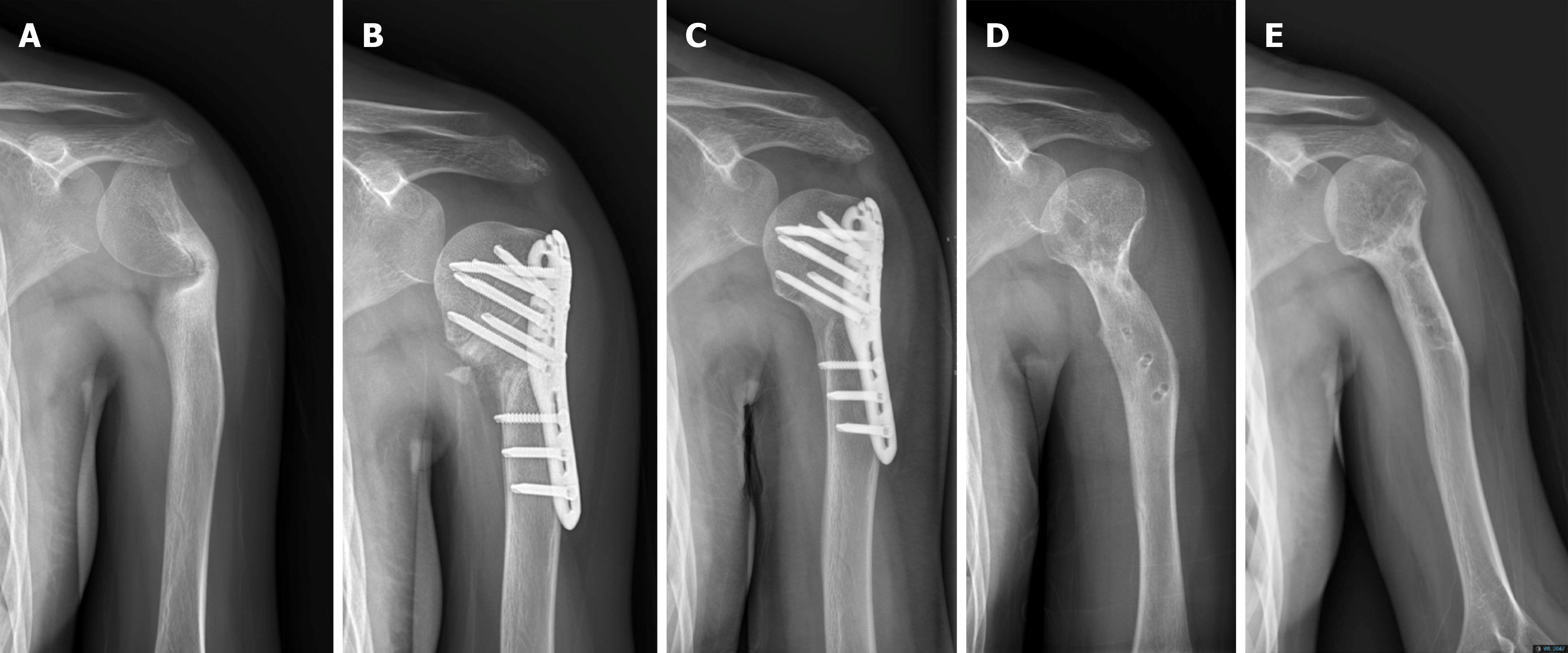
Initial imaging studies indicated an angulated old fracture at the proximal left humeral neck (Figure 1). Subsequent exa
Considering the patient’s medical history, the final diagnosis indicated a case of left humerus SBC with varus malunion or suspected postinfection sequelae of osteomyelitis.
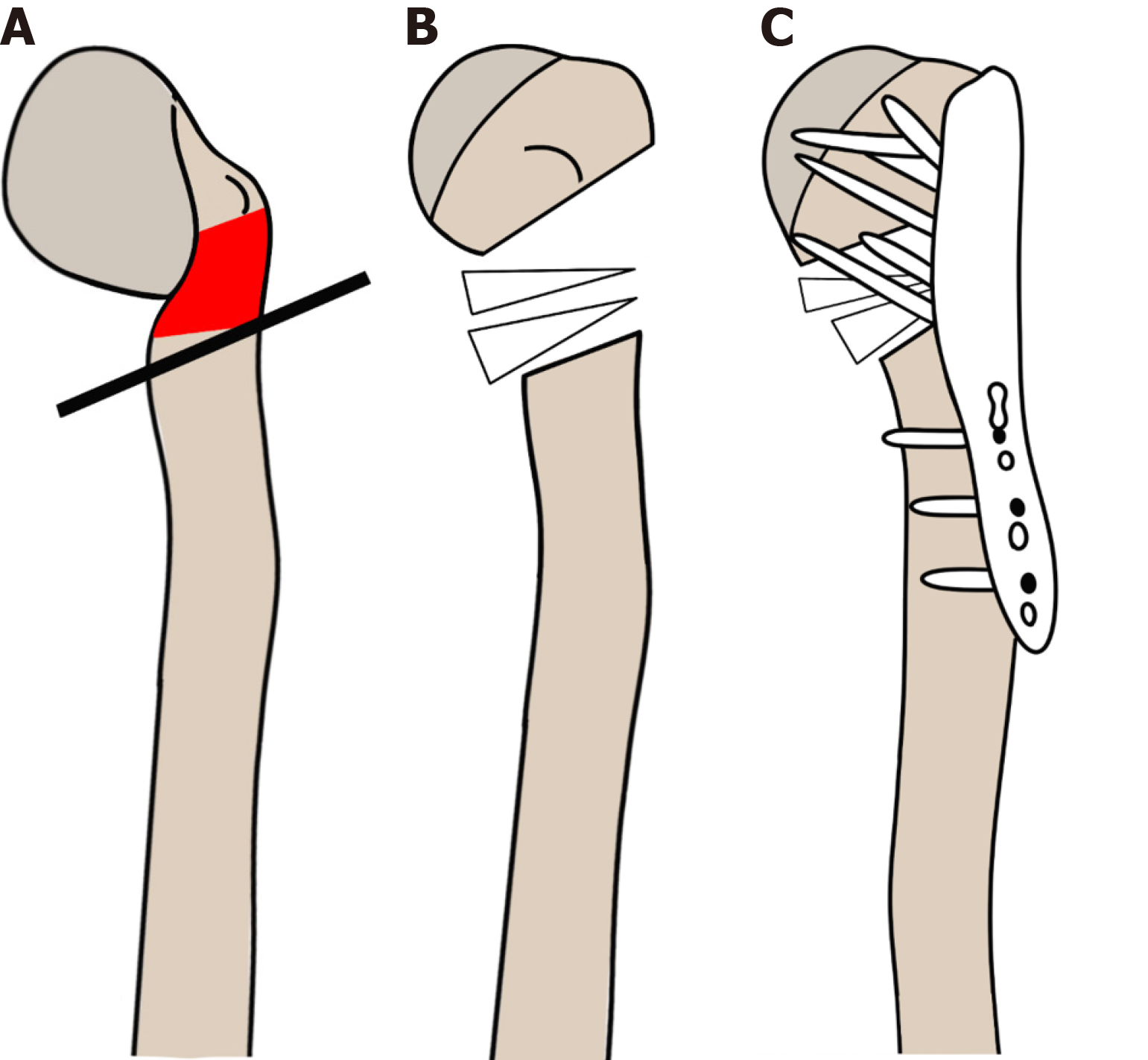
Surgical intervention was recommended for this case of left humerus SBC with varus malunion or suspected postinfection sequela of osteomyelitis. The procedure involved placing the patient under general anesthesia in a semi-sitting position. The anterior approach was utilized to expose the proximal metaphysis and diaphysis of the left humerus. Os
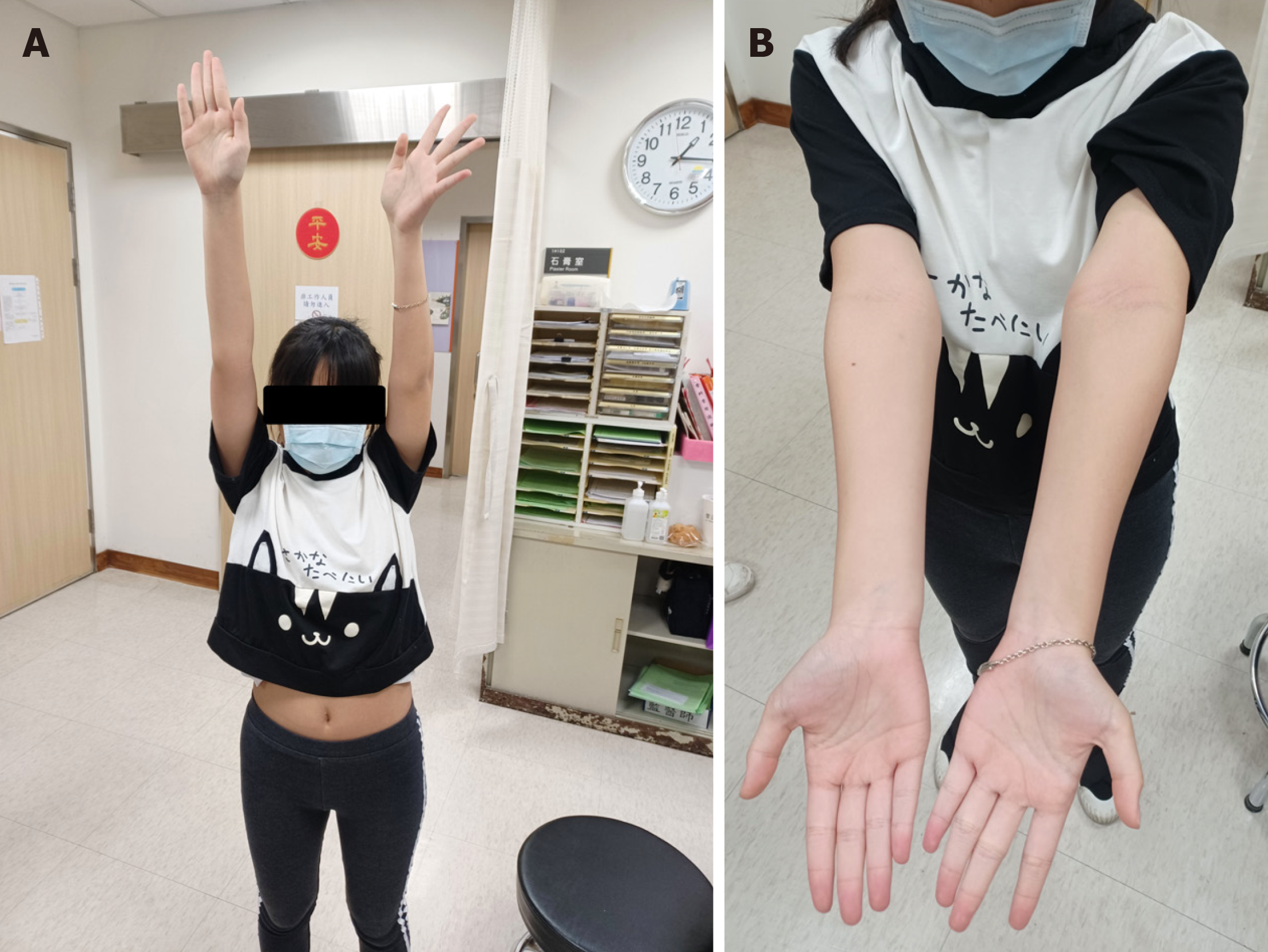
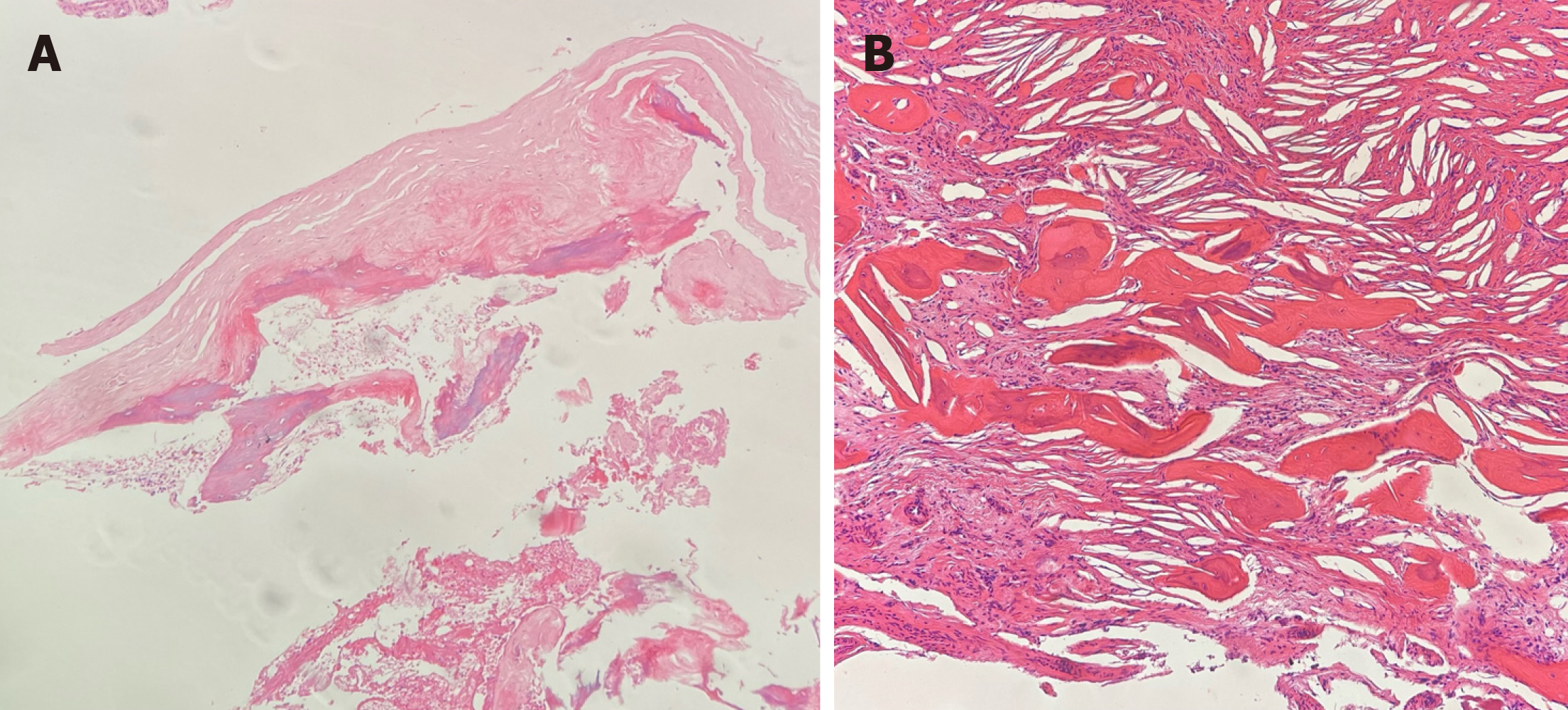
Postoperatively, the patient was immobilized in a sling for 2 wk. The left shoulder length discrepancy was reduced by 2 cm. After 1 month, she exhibited full active ROM in the left shoulder, with no reported wound complications or infection (Table 1 and Figure 4). Follow-up radiographs indicated no progression of the lesion; the osteotomy site showed solid union at 1 month and 1 year postoperatively (Figure 1). The histological report revealed degenerated cortical bone and cartilage tissue, with fibrous cystic wall with fibrin-like materials, cholesterol clefts and surrounding some new bone formation (Figure 5), leading to the diagnosis of SBC. While no pain or discomfort was reported, the implant was re
SBC are benign metaphyseal lytic lesions predominantly occurring in males[3]. Despite research, the etiology of SBC remains inconclusive[4,5]. Most cases of SBC are asymptomatic and are discovered incidentally. Spontaneous resolution of SBC occurs in only about 5% to 10% of cases[6,7]. Symptomatic cases are often associated with pathological fractures (63%-87%)[1,8] and less than 15% of cysts resolve spontaneously after a fracture occurs[5,9]. Presently, there is no con
The primary differential diagnoses for pathological fractures in children aged 5–10 years include SBC, aneurysmal bone cysts (ABC), non-ossifying fibroma, and osteomyelitis[11]. In our patient, the lesion was located in the proximal humerus, consistent with the predisposing location of SBC. As our patient exhibited no signs of inflammation, bruises, or swelling, and had not received antibiotic treatment, chronic osteomyelitis was ruled out. Given the similar clinical sym
Radiographic findings in our case revealed an old, angulated fracture at the proximal left humeral neck (Figure 1). Although the characteristic cystic lesions of SBC were not visibly evident on radiography and MRI, the possibility of SBC could not be ruled out. Furthermore, MRI showed a smoother sclerotic junction with the absence of fat stranding or in
A pathological fracture occurred in association with the benign lesion, leading to the subsequent displacement of the fracture and resulting in a malunion at the left humeral neck. The histological report showed fibrous cystic wall with fi
As such, we posit that this patient experienced an initially asymptomatic pathologic fracture due to low-energy trau
On rare occasions, SBC may lead to growth disturbances, and, the underlying mechanism remains a subject of debate. Some evidence suggests that the cyst fluid itself may directly disrupt the physis, causing growth disturbances[12-14]. Other potential processes include: (1) Fractures through the cyst, damaging the physis and resulting in growth arrest; (2) direct extension of the cyst through the physis; and (3) iatrogenic damage to a developing physis due to surgical removal of a cyst in proximity[6,12-18]. Regardless of the etiology, growth disturbances ultimately result in angular deformity and/or limb length discrepancy in the affected limb. In the case of our patient, limb length discrepancy was evident be
We proposed two hypotheses to explain the etiology of our patient’s condition. First, we considered the possibility of direct extension of the SBC through the epiphysis on the medial side, or the direct disruption of the physis by the cyst fluid itself, leading to growth arrest and subsequent varus deformity of the humerus. Given that the proximal physis con
The second hypothesis proposed was that the epiphysis was damaged by repetitive pathological fractures due to SBC. The bone affected by SBC is weakened and prone to pathological fractures, which can, in turn, damage the epiphysis. As a consequence of these pathological fractures, varus humeral head angulation developed. The muscles pulling on the proximal humerus allowed pathological fractures to heal with an increasing varus deformity, giving rise to the typical complaint of severe shoulder ROM limitations in abduction and flexion. Furthermore, due to a defective medial epi
We presented two surgical intervention options for the patient. The first option involved acute correction of the pro
Thus, the surgical treatment of acute correction for the proximal humerus varus deformity was performed. This ap
In conclusion, we presented a case of SBC presenting with a pathological fracture, complicated with malunion of the displaced fracture, varus deformity, and limb length discrepancy. The discussion included differential diagnoses of SBC, alongside a comprehensive review of the current literature. In our case, the patient’s limb length discrepancy and varus deformity emerged as complications of the SBC and pathological fracture. It underscores the importance of close follow-up in patients with SBC to monitor the potential occurence of growth arrest.
| 1. | Zhang K, Wang Z, Zhang Z. Comparison of curettage and bone grafting combined with elastic intramedullary nailing vs curettage and bone grafting in the treatment of long bone cysts in children. Medicine (Baltimore). 2019;98:e16152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Donaldson S, Chundamala J, Yandow S, Wright JG. Treatment for unicameral bone cysts in long bones: an evidence based review. Orthop Rev (Pavia). 2010;2:e13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Deventer N, Deventer N, Gosheger G, de Vaal M, Vogt B, Budny T. Current strategies for the treatment of solitary and aneurysmal bone cysts: A review of the literature. J Bone Oncol. 2021;30:100384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 4. | Zhang P, Zhu N, Du L, Zheng J, Hu S, Xu B. Treatment of simple bone cysts of the humerus by intramedullary nailing and steroid injection. BMC Musculoskelet Disord. 2020;21:70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Sung AD, Anderson ME, Zurakowski D, Hornicek FJ, Gebhardt MC. Unicameral bone cyst: a retrospective study of three surgical treatments. Clin Orthop Relat Res. 2008;466:2519-2526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Ahn JI, Park JS. Pathological fractures secondary to unicameral bone cysts. Int Orthop. 1994;18:20-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 57] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Chuo CY, Fu YC, Chien SH, Lin GT, Wang GJ. Management strategy for unicameral bone cyst. Kaohsiung J Med Sci. 2003;19:289-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Erol B, Onay T, Topkar OM, Tokyay A, Aydemir AN, Okay E. A comparative study for the treatment of simple bone cysts of the humerus: open curettage and bone grafting either without instrumentation or with intramedullary nailing. J Pediatr Orthop B. 2017;26:5-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Neer CS 2nd, Francis KC, Marcove RC, Terz J, Carbonara PN. Treatment of unicameral bone cyst. A follow-up study of one hundred seventy-five cases. J Bone Joint Surg Am. 1966;48:731-745. [PubMed] |
| 10. | Hou HY, Wu K, Wang CT, Chang SM, Lin WH, Yang RS. Treatment of unicameral bone cyst: a comparative study of selected techniques. J Bone Joint Surg Am. 2010;92:855-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Canavese F, Samba A, Rousset M. Pathological fractures in children: Diagnosis and treatment options. Orthop Traumatol Surg Res. 2016;102:S149-S159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Stanton RP, Abdel-Mota'al MM. Growth arrest resulting from unicameral bone cyst. J Pediatr Orthop. 1998;18:198-201. [PubMed] |
| 13. | Gupta AK, Crawford AH. Solitary bone cyst with epiphyseal involvement: confirmation with magnetic resonance imaging. A case report and review of the literature. J Bone Joint Surg Am. 1996;78:911-915. [PubMed] |
| 14. | Ovadia D, Ezra E, Segev E, Hayek S, Keret D, Wientroub S, Lokiec F. Epiphyseal involvement of simple bone cysts. J Pediatr Orthop. 2003;23:222-229. [PubMed] |
| 15. | Cohen J. Unicameral bone cysts. a current synthesis of reported cases. Orthop Clin North Am. 1977;8:715-736. [PubMed] |
| 16. | Violas P, Salmeron F, Chapuis M, Sales de Gauzy J, Bracq H, Cahuzac JP. Simple bone cysts of the proximal humerus complicated with growth arrest. Acta Orthop Belg. 2004;70:166-170. [PubMed] |
| 17. | Haims AH, Desai P, Present D, Beltran J. Epiphyseal extension of a unicameral bone cyst. Skeletal Radiol. 1997;26:51-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Reif TJ, Matthias J, Fragomen AT, Rozbruch SR. Limb Length Discrepancy and Angular Deformity due to Benign Bone Tumors and Tumor-like Lesions. J Am Acad Orthop Surg Glob Res Rev. 2021;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 19. | Lee FY, Schoeb JS, Yu J, Christiansen BD, Dick HM. Operative lengthening of the humerus: indications, benefits, and complications. J Pediatr Orthop. 2005;25:613-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu TF, China S-Editor: Liu JH L-Editor: A P-Editor: Xu ZH