Published online May 6, 2024. doi: 10.12998/wjcc.v12.i13.2248
Peer-review started: December 11, 2023
First decision: February 8, 2024
Revised: February 29, 2024
Accepted: March 28, 2024
Article in press: March 28, 2024
Published online: May 6, 2024
Processing time: 136 Days and 3.7 Hours
Cardiac arrest (CA) induced by electric shock is a rare occurrence, particularly in cases of prolonged CA. Currently, there is limited literature on similar incidents, and we present a relevant case report.
A 27-year-old Asian male man, experiencing respiratory CA due to electric shock, was successfully restored to sinus rhythm after 50 min of cardiopulmonary re
Prolonging resuscitation time can enhance the chances of survival for patients, this study provide valuable insights into the management of electric shock-indu
Core Tip: The successful management of a young patient experiencing respiratory cardiac arrest due to electrical injury was accomplished through prolonged cardiopulmonary resuscitation. This study emphasizes the significance of persisting in res
- Citation: Zhang J, Qiao YR, Yang YD, Pan GZ, Lv CQ. Recovering from prolonged cardiac arrest induced by electric shock: A case report. World J Clin Cases 2024; 12(13): 2248-2253
- URL: https://www.wjgnet.com/2307-8960/full/v12/i13/2248.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i13.2248
Timely and proficient implementation of cardiopulmonary resuscitation (CPR) is crucial for the successful resuscitation of patients who undergo electric shock-induced cardiac arrest (CA), a critical and urgent condition in the emergency de
The electrical shock led to a 50-min respiratory CA.
A 27-year-old healthy young man suffered from respiratory and CA due to accidental electric shock (AC 380 V). The family members at the scene cut off power and began to implement CPR within 5 min. Paramedics arrived at the scene in 15 min and continued CPR, while transferring the patient to the emergency department of our hospital.
He used to be healthy.
The parents are in good health and have no reported family history of genetic disease, infectious disease, or similar conditions.
Upon arrival at the emergency department, the patient displayed no spontaneous respiration or heartbeat. Immediate measures, including electrocardiography monitoring, tracheal intubation, continuous external chest compression, and intravenous administration of rapid fluid rehydration, adrenaline, and dopamine were implemented. Approximately 20 min later after receiving rescue medication, the patient regained a spontaneous heartbeat, only to suffer from repeated ventricular fibrillation. The patient achieved sinus rhythm after 8 electric defibrillation attempts, a 150 mg amiodarone intravenous push, and a 1 mg/min intravenous drip. However, the patient remained unconscious with frequent convul
The results of peripheral blood examination and arterial blood gas analysis are presented in Table 1.
| Blood examination | WBC | RBC | Hg (g/L) | PLT | ALT (U/L) | AST (U/L) | TBIL (μmol/L) | Troponin (μg/L) | Myoglobin (μg/L) | CKMB (μg/L) | Arterial blood gas analysis | |||||
| pH | PaO2 (mmHg) | PaCO2 (mmHg) | HCO3 (mmol/L) | Lac (mmol/L) | BE (mmol/L) | |||||||||||
| Day 1 | 21.1 | 6.12 | 166 | 397 | 163 | 290 | 11 | 15.4 | 3811 | 79.2 | 7.27 | 59.2 | 37.8 | 17 | 12.9 | -9.13 |
| Day 2 | 21 | 5.48 | 146 | 309 | 164 | 125 | 6.1 | 9.76 | 2028 | 50.2 | 7.361 | 189.5 | 40.4 | 26.5 | 1 | 0.48 |
| Reference value | 3.5-9.5 | 4.3-5.8 | 130-175 | 125-350 | 9-52 | 14-36 | 3-22 | 0.02-0.25 | 0-140 | 0-25 | 7.35-7.45 | 80-100 | 35-45 | 22-26 | 1.0-1.7 | -3.0 to 3.0 |
The aforementioned information is referenced in the section dedicated to treatment.
Electrical injury, respiratory and CA, and postcardiac arrest syndrome.
The patient underwent a sequence of interventions, including administration of amiodarone to stabilize cardiac rhythm, rapid rehydration with succinyl gelatin, acid correction using sodium bicarbonate, sedation and muscle relaxation th
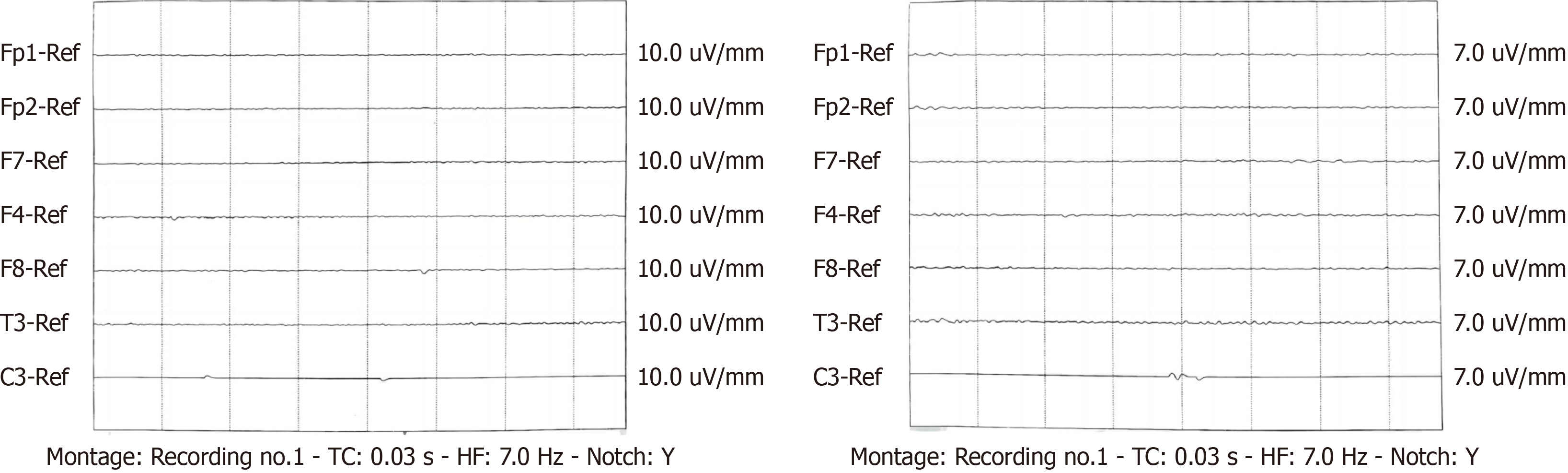
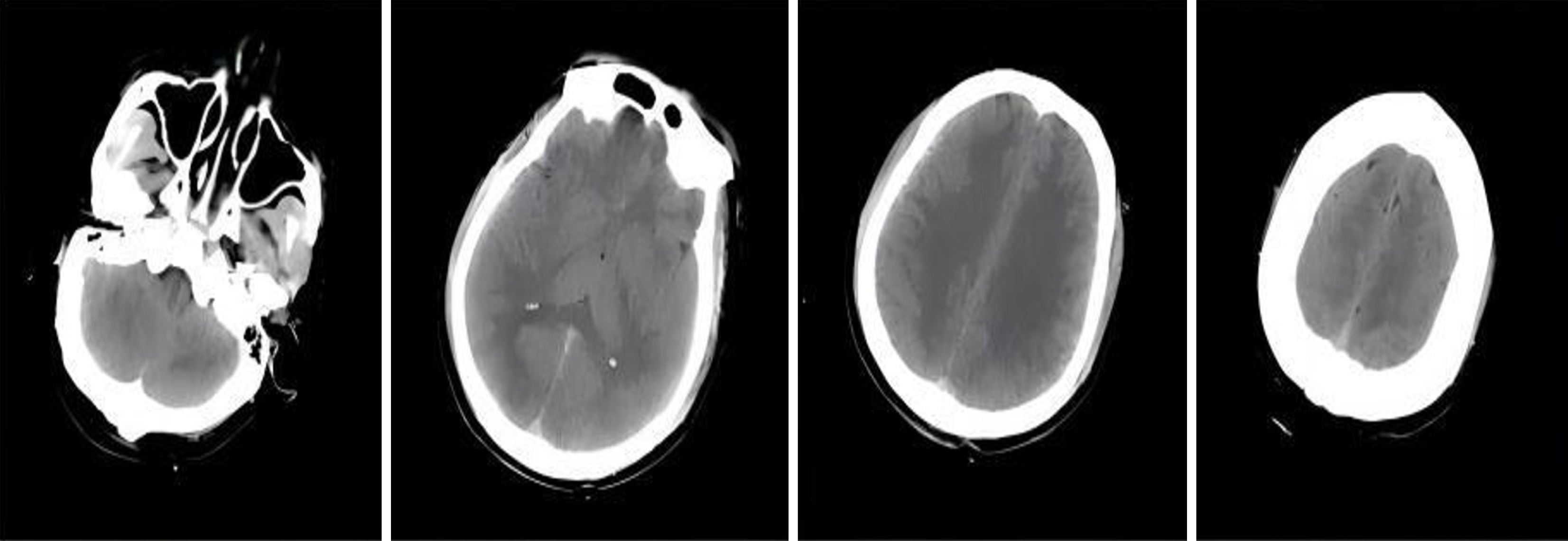
Two days post-admission, the patient underwent a repeated blood test (Table 1). The abdominal physical examination showed no positive signs, and bowel sounds were approximately 4 per minute. Enteral nutrition was administered, and ambulatory electroencephalography examination revealed severe abnormal brain waves (low voltage) (Figure 1). The computed tomography scan of the head, however, revealed no apparent abnormalities (Figure 2). Troxerutin brain pro
The patient's respiratory function improved 4 d post-admission, with Venturi oxygen used instead of mechanical ven
Electrical injury results in tissue damage and dysfunction upon entry of the current into the body, clinically manifesting as localized damage at the shock site, systemic injuries, particularly to the cardiovascular and nervous systems, and, in severe cases, respiratory and CA. The severity of electric injury is contingent on the intensity, type, voltage, contact resistance, duration, and pathway of the current within the body. Electric current typically follows the course of blood vessels and nerves, and when it traverses the heart, it can elicit respiratory depression or arrest, ventricular fibrillation, or CA[1]. In this case report, the patient promptly entered a coma subsequent to electric shock. Continuous CPR was im
The probability of successful CPR for patients with CA decreases to less than 3% if spontaneous rhythm recovery is not achieved within 20 min, and clinical CPR may be terminated if there is still no detectable cardiac electrical activity after 30 min. However, given that most patients with electrical injuries are young adults with normal heart and lung function, medical professionals should embrace the concept of ultra-long CPR and endeavor to extend the CPR time in clinical practice, actively rescuing and saving lives[6].
Due to changes in societal roles, elderly individuals seldom encounter respiratory and CA caused by external or human factors, which sets them apart significantly from non-elderly adult patients. The primary etiologies of out-of-hospital CA (OHCA) among the elderly encompass cardiogenic and respiratory ailments as well as asphyxia. Owing to physiological deterioration, exacerbation of chronic underlying conditions, and diminished drug responsiveness fo
This case report presents a young male patient who underwent continuous CPR for 50 min, ultimately restoring au
Modern medical resuscitation strategies prioritize cardiopulmonary and cerebral resuscitation. Even during the resuscitation process, interventions such as hypothermia, dehydration, cranial pressure reduction, hyperbaric oxygen, and cerebral nerve protection should be implemented to ensure effective cerebral resuscitation. The timeliness and efficacy of cerebral resuscitation are crucial for patient recovery. Following successful CPR in this case, the patient received hypothermia, dehydration, brain tissue protection and early hyperbaric oxygen therapy. Hyperbaric oxygen therapy has been extensively used in cerebral resuscitation, and literature indicates that it can alleviate post-CPR organ ischemia and hypoxia, facilitating brain function recovery[7]. Therefore, it is recommended to administer hyperbaric oxygen therapy promptly.
In summary, the successful treatment in this case can be attributed to the following factors: (1) Implementation of effective rescue measures, including continuous and uninterrupted chest compressions, defibrillation, prompt esta
For patients experiencing sudden cardiac and respiratory arrest secondary to electrical injuries, particularly those aged between young and middle-aged without significant organ dysfunction, the pursuit of rescuing should not be relin
| 1. | Fish R. Electric shock, Part II: Nature and mechanisms of injury. J Emerg Med. 1993;11:457-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (2)] |
| 2. | Yan S, Gan Y, Jiang N, Wang R, Chen Y, Luo Z, Zong Q, Chen S, Lv C. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 167] [Cited by in RCA: 614] [Article Influence: 102.3] [Reference Citation Analysis (0)] |
| 3. | Merchant RM, Topjian AA, Panchal AR, Cheng A, Aziz K, Berg KM, Lavonas EJ, Magid DJ; Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, Resuscitation Education Science, and Systems of Care Writing Groups. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S337-S357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 668] [Cited by in RCA: 485] [Article Influence: 80.8] [Reference Citation Analysis (0)] |
| 4. | Bai Z, Wang L, Yu B, Xing D, Su J, Qin H. The success rate of cardiopulmonary resuscitation and its correlated factors in patients with emergency prehospital cardiac arrest. Biotechnol Genet Eng Rev. 2023;1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Sladjana A, Gordana P, Ana S. Emergency response time after out-of-hospital cardiac arrest. Eur J Intern Med. 2011;22:386-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Liu W, Liu LN, Lin CW, Wang HY, Wang XD. Successful Recovery After Prolonged Cardiopulmonary Resuscitation and Rescue Thrombolytics in a Patient with Cardiac Arrest Secondary to Presumed Massive Pulmonary Embolism. Risk Manag Healthc Policy. 2021;14:4253-4256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Schmitz J, Liebold F, Hinkelbein J, Nöhl S, Thal SC, Sellmann T. Cardiopulmonary resuscitation during hyperbaric oxygen therapy: a comprehensive review and recommendations for practice. Scand J Trauma Resusc Emerg Med. 2023;31:57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mallet RT, United States S-Editor: Zheng XM L-Editor: A P-Editor: Xu ZH