Published online Oct 16, 2023. doi: 10.12998/wjcc.v11.i29.7248
Peer-review started: August 19, 2023
First decision: September 4, 2023
Revised: September 10, 2023
Accepted: September 22, 2023
Article in press: September 22, 2023
Published online: October 16, 2023
Processing time: 55 Days and 0.5 Hours
Thyroglossal duct cysts (TDC) are common congenital deformities. Most of them are cysts formed by the thyroglossal ducts that do not disappear and degenerate in the early embryonic stage. TDC exists alone and is rarely complicated by other congenital embryonic malformations. Only a few reports of TDC with branchial cleft cysts, thyroid cancer, thyroid hematoma, and epidermoid cysts have been reported. Therefore, we report a patient with TDC and parathyroid cyst (PC), a rare disease that has never been reported.
A 47-year-old woman presented to clinic in April 2021 with a neck tumor which she had noticed 5 d earlier. We perfected the relevant examinations, such as ultrasound and computed tomography, and resected the tumor. After surgical treatment, the pathology revealed a cervical thyroglossal duct cyst and a left lobe parathyroid cyst. The patient was followed up for 1 year without significant recurrence.
We report a patient with a simultaneous TDC and a PC to explore the correlation between the two congenital anomalies.
Core Tip: Thyroglossal duct cysts (TDC) exists alone and is rarely complicated by other congenital embryonic malformations. Only a few reports of TDC with branchial cleft cysts, thyroid cancer, thyroid hematoma, and epidermoid cysts have been reported. However, the patient coexisted with TDC and parathyroid cyst (PC), a rare disease that has never been reported in the weapons literature. Therefore, we report a patient with a simultaneous TDC and a PC to explore the correlation between the two congenital anomalies.
- Citation: Chen GY, Li T. Simultaneous thyroglossal duct cyst with parathyroid cyst: A case report. World J Clin Cases 2023; 11(29): 7248-7252
- URL: https://www.wjgnet.com/2307-8960/full/v11/i29/7248.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i29.7248
Thyroglossal duct cysts (TDC) are common congenital deformities. Most of them are cysts formed by the thyroglossal ducts that do not disappear and degenerate in the early embryonic stage. TDC exists alone and is rarely complicated by other congenital embryonic malformations. Only a few reports of TDC with branchial cleft cysts, thyroid cancer, thyroid hematoma, and epidermoid cysts have been reported. Therefore, we report a patient with TDC and parathyroid cyst (PC), a rare disease that has never been reported.We report a patient with a simultaneous TDC and a PC to explore the correlation between the two congenital anomalies.
A neck tumor which she had noticed 5 d earlier.
A 47-year-old woman presented to clinic in April 2021 with a neck tumor which she had noticed 5 d earlier. Clinical examination revealed a 4cm-diameter soft mass under the jaw, which could be moved up and down with swallowing and tongue extension, and a 2-cm soft mass could be palpated under the left thyroid lobe. Preoperative examination of blood parathyroid hormone, serum calcium and serum phosphorus were all at normal levels. Ultrasonography revealed a Thyroglossal duct cyst and a cystic mass in the left thyroid lobe, computed tomography (CT) scan of the neck showed a low-density lesion anterior to the left thyroid cartilage, and a lesion posterior to the lower pole of the left thyroid lobe.
Without special past illness.
Without special personal and family history.
Clinical examination revealed a 4 cm-diameter soft mass under the jaw, which could be moved up and down with swallowing and tongue extension, and a 2-cm soft mass could be palpated under the left thyroid lobe.
Preoperative examination of blood parathyroid hormone, serum calcium and serum phosphorus were all at normal levels.
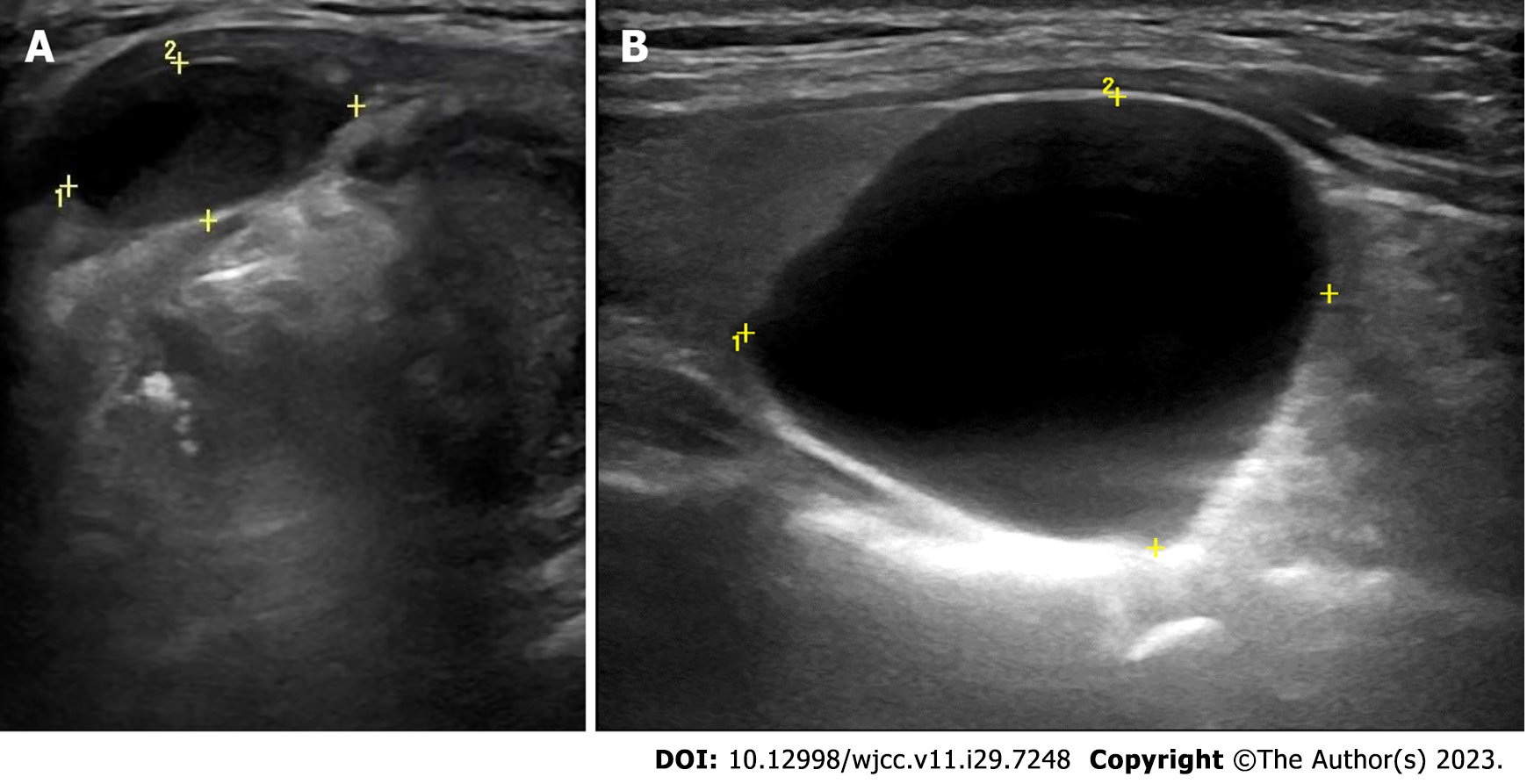
Ultrasonography revealed a thyroglossal duct cysts and a cystic mass in the left thyroid lobe, see Figure 1. CT scan of the neck showed a low-density lesion anterior to the left thyroid cartilage, and a lesion posterior to the lower pole of the left thyroid lobe, as shown in Figure 2.
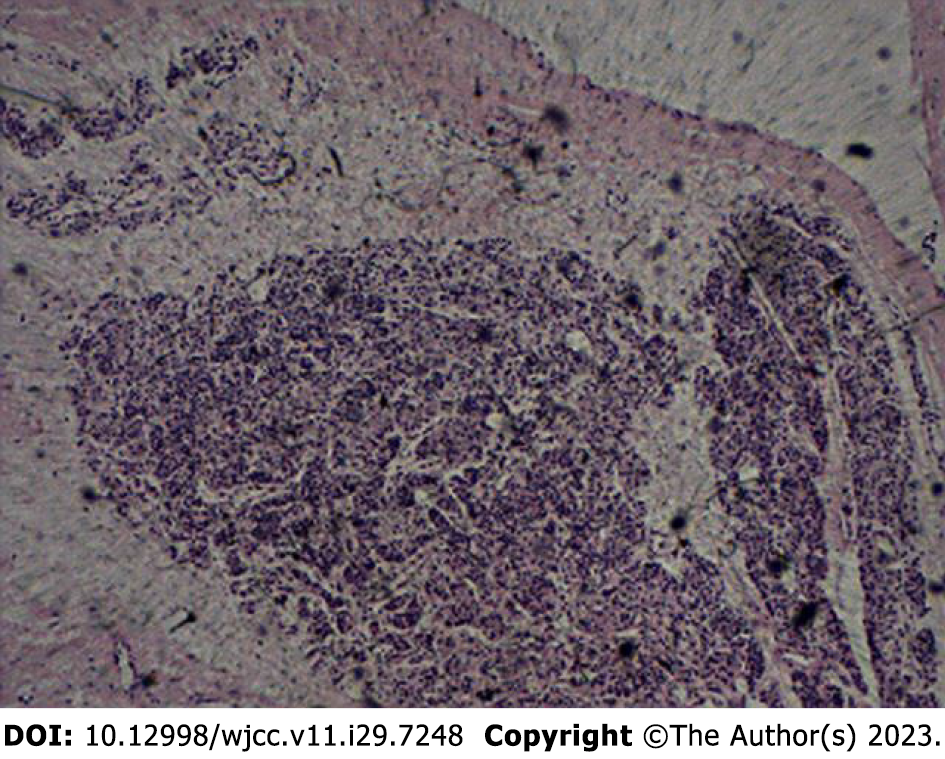
After surgical treatment, the pathology revealed a cervical TDC and a left lobe parathyroid cyst, as shown in Figure 3.
The TDC was treated by the classic Sistrunk procedure, and parathyroid cyst was treated by surgical resection.
The patient was followed up for 1 year without significant recurrence.
TDC are common congenital deformities. Only a few case of TDC with other congenital deformities have been reported[1-5], while PC are rare, and are easily misdiagnosed as thyroid cysts. When the embryo develops to the sixth week, the thyroglossal duct degenerates on its own, leaving only a shallow depression at its starting point, the cecum. If the degeneration of the thyroglossal duct is incomplete during this process, the remaining epithelium may form a TDC in the course of the anterior median neck from the base of the tongue to the thyroid. The pathogenesis of PC is still unclear, but the pathogenic factors currently considered include: (1) The third or fourth pharyngeal sac remains during embryonic development[6]; (2) the residual Kursteiner’s canal develops; (3) the fusion of microcysts[7]; (4) hemorrhage or degeneration of parathyroid adenoma[8]; and (5) parathyroid secretions are retained in vesicles[9]. Most scholars support the first hypothesis, because the third or fourth pharyngeal sac can form cysts during embryonic development, and such cysts are characterized by thin walls and transparent fluid inside, while other hypotheses form cysts with thick walls, the cyst fluid is bloody or purulent. In this case, both TDC and parathyroid cysts were combined, and the patient had a history of congenital malformations such as primary iris cysts, which further indicated that there was a correlation between the embryonic origins of these three diseases.
Clinically, TDC presents as anterior neck mass that moves on protruding the tongue or swallowing due to its attachment to the hyoid bone. However, although clinical history and examination may suggest the diagnosis, imaging is required to confirm the clinical diagnosis and assess the anatomic extent of the lesion prior to treatment[10].
Ultrasonography is an ideal initial imaging investigation for neck masses as it available, inexpensive, and does not involve ionizing radiation. For a curved surface such as the neck, using a gel pad can obtain more panoramic ultrasound images, and it allows the detection of otherwise-missed peri- or intra-lesional flow signals on Doppler imaging, increasing the diagnostic role of this technique in differential diagnosis of superficial lesions[11,12]. The typical ultrasonography description of a TDC is that of a well-circumscribed, round or oval anechoic lesion with thin walls and increased through-transmission; no internal fow with Doppler imaging[13].
The classic Sistrunk procedure is currently the preferred method for the treatment of TDC, which significantly reduces the postoperative recurrence rate[14,15]. The treatment of NPC has not yet been finalized. The current treatment methods include puncture aspiration or absolute ethanol ablation, surgical resection, and regular review. Surgical resection has gradually become the mainstream method for the treatment of NPC. The traditional anterior cervical approach surgery can completely remove the cyst and relieve the compression symptoms of the patient, which is a safe and effective treatment method[16,17]. In this case, no recurrence was found in the 1-year follow-up after surgical resection.
Simultaneous parathyroid cysts and TDC is very rare, and the embryologic origins of TDC and inferior PC appear to be associated.
| 1. | Shahin A, Burroughs FH, Kirby JP, Ali SZ. Thyroglossal duct cyst: a cytopathologic study of 26 cases. Diagn Cytopathol. 2005;33:365-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Bhansali SA, Chang CH, Hotaling AJ. Pathologic quiz case 2. Epidermoid cyst and thyroglossal duct (TGD) cyst. [DOI] [Full Text] |
| 3. | Cherian MP, Nair B, Thomas S, Somanathan T, Sebastian P. Synchronous papillary carcinoma in thyroglossal duct cyst and thyroid gland: case report and review of literature. Head Neck. 2009;31:1387-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Tyson RW, Groff DB. An unusual lateral neck cyst with the combined features of a bronchogenic, thyroglossal, and branchial cleft origin. Pediatr Pathol. 1993;13:567-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Tsang SK, Maher J. Thyroid hemiagenesis accompanying a thyroglossal duct cyst: a case report. Clin Nucl Med. 1998;23:229-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Ippolito G, Palazzo FF, Sebag F, Sierra M, De Micco C, Henry JF. A single-institution 25-year review of true parathyroid cysts. Langenbecks Arch Surg. 2006;391:13-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Castleman B, Mallory TB. The Pathology of the Parathyroid Gland in Hyperparathyroidism: A Study of 25 Cases. Am J Pathol. 1935;11:1-72.17. [PubMed] |
| 8. | Pontikides N, Karras S, Kaprara A, Cheva A, Doumas A, Botsios D, Moschidis A, Efthimiou E, Wass J, Krassas G. Diagnostic and therapeutic review of cystic parathyroid lesions. Hormones (Athens). 2012;11:410-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Lima AC, Fregnani ER, Silva-Sousa YT, da Cruz Perez DE. Parathyroid hormone/parathyroid hormone-related peptide receptor 1 expression in odontogenic cystic lesions. Int Endod J. 2012;45:209-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Huoh KC, Durr ML, Meyer AK, Rosbe KW. Comparison of imaging modalities in pediatric thyroglossal duct cysts. Laryngoscope. 2012;122:1405-1408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Corvino A, Sandomenico F, Corvino F, Campanino MR, Verde F, Giurazza F, Tafuri D, Catalano O. Utility of a gel stand-off pad in the detection of Doppler signal on focal nodular lesions of the skin. J Ultrasound. 2020;23:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 12. | Tsui BC, Tsui J. A flexible gel pad as an effective medium for scanning irregular surface anatomy. Can J Anaesth. 2012;59:226-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Corvino A, Pignata S, Campanino MR, Corvino F, Giurazza F, Tafuri D, Pinto F, Catalano O. Thyroglossal duct cysts and site-specific differential diagnoses: imaging findings with emphasis on ultrasound assessment. J Ultrasound. 2020;23:139-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Rohof D, Honings J, Theunisse HJ, Schutte HW, van den Hoogen FJ, van den Broek GB, Takes RP, Wijnen MH, Marres HA. Recurrences after thyroglossal duct cyst surgery: Results in 207 consecutive cases and review of the literature. Head Neck. 2015;37:1699-1704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Goins MR, Beasley MS. Pediatric neck masses. Oral Maxillofac Surg Clin North Am. 2012;24:457-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Xu P, Xia X, Li M, Guo M, Yang Z. Parathyroid cysts: experience of a rare phenomenon at a single institution. BMC Surg. 2018;18:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Ujiki MB, Nayar R, Sturgeon C, Angelos P. Parathyroid cyst: often mistaken for a thyroid cyst. World J Surg. 2007;31:60-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Corvino A, Italy S-Editor: Liu JH L-Editor: A P-Editor: Liu JH