Published online Aug 16, 2023. doi: 10.12998/wjcc.v11.i23.5602
Peer-review started: May 24, 2023
First decision: June 19, 2023
Revised: July 1, 2023
Accepted: July 17, 2023
Article in press: July 17, 2023
Published online: August 16, 2023
Processing time: 83 Days and 13.7 Hours
Ex vivo liver resection and autotransplantation (ELRA) is an essential approach for treating patients with end-stage hepatic alveolar echinococcosis (AE), and its surgical indications involve severe invasion of important hepatic vessels, which makes in vivo resection impossible. Revascularization is a major step in the process of ELRA, which is extremely challenging when the invaded vessels have huge defects.
Herein, we have reported the case of a 26-year-old patient with hepatic AE in an autologous liver graft who underwent complex inferior vena cava (IVC) reconstruction using disease-free IVC, autologous portal vein fragments, and umbilical vein within the ligamentum teres hepatis. The patient showed good surgical recovery without vascular-related complications during the long-term follow-up.
We reviewed three studies that have reported complex revascularization of the IVC. This case report and systematic review showed that the use of autologous perihepatic vessels prevents donor-area trauma, immune rejection, and other adverse reactions. When the blood vessel is severely invaded and a single vascular material cannot repair and reconstruct the defect, ELRA may provide a safe and feasible surgical approach, which has good prospects for clinical application.
Core Tip:Ex vivo liver resection and autotransplantation (ELRA) is an essential approach to cure end-stage hepatic alveolar echinococcosis (AE). Revascularization is a central and challenging step in the process of ELRA when the invaded vessels have large defects. Here, we report the case of a 26-year-old patient with hepatic AE in an autologous liver graft who underwent complex inferior vena cava (IVC) reconstruction using disease-free IVC, autologous portal vein fragments and umbilical vein within the ligamentum teres hepatis and with good surgical recovery without vascular-related complications at long-term follow-up. This study demonstrate that the blood vessel is severely invaded and a single vascular material cannot repair and reconstruct the defect, this technique may provide a feasible surgical option for revascularization during ELRA and has good prospects for clinical application.
- Citation: Humaerhan J, Jiang TM, Aji T, Shao YM, Wen H. Complex inferior vena cava reconstruction during ex vivo liver resection and autotransplantation: A case report. World J Clin Cases 2023; 11(23): 5602-5609
- URL: https://www.wjgnet.com/2307-8960/full/v11/i23/5602.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i23.5602
Hepatic alveolar echinococcosis (AE) is a rare zoonotic infection that is caused by Echinococcus multilocularis[1]. It is an invasive disease with systemic metastasis[2]; however, its insidious onset and slow progression make early diagnosis difficult. Radical hepatectomy combined with antiparasitic medication is the only curative treatment approach for patients with hepatic alveolar echinococcosis; however, this approach is feasible for only 35% of patients due to delay in diagnosis[3,4]. Previous studies have shown that ex vivo liver resection and autotransplantation (ELRA) can be an effective alternative to allotransplantation in patients with end-stage hepatic AE[5-7]. Compared with allotransplantation, ELRA overcomes the limitations of shortage of liver sources and long-term postoperative immunosuppression[8-10]. Therefore, ELRA is a better choice for patients with end-stage hepatic AE where complete resection of the lesion is not possible and technical challenges, such as in vivo revascularization, are difficult to overcome[9,11,12]. End-stage hepatic AE can invade major bile ducts and blood vessels, which requires additional repair and reconstruction procedures of the vessels during ELRA[1,2,13]. In this case, the selection of an appropriate revascularization material is significant. Based on the degree of vascular invasion, reconstruction materials can be selected from autologous vessels, allogeneic vessels, and artificial vessels. Complex revascularization with multiple vascular remnants can also be an effective treatment approach when the area of lesion invasion is huge and a single vascular patch is not sufficient for revascularization. Herein, we have presented a case of complex reconstruction of the inferior vena cava (IVC) using autologous portal vein (PV) fragments, umbilical vein within the ligamentum teres hepatis (LTH), and disease-free IVC during ELRA. Furthermore, the available literature on the complex reconstruction of the IVC during ELRA was reviewed to summarize the experience of the complex reconstruction of the IVC.
A 26-year-old Chinese woman presented to the general surgery clinic with a complaint of upper right abdominal pain for 2 wk.
Symptoms started 2 wk before presentation with recurrent upper right abdominal pain.
No previous complaints of discomfort.
The patient has a long history of living in a pastoral area. She denied any family history of malignant tumours.
On physical examination, the vital signs were as follows: Body temperature, 36.2℃; blood pressure, 121/72 mmHg; heart rate, 76 beats per min; respiratory rate, 16 breaths per min. Flat abdomen, no abdominal varicose veins, no abdominal muscle tension, no tenderness, no rebound pain, no liquid wave tremor, no water vibration sound, no abdominal mass, bowel sound 4 times per minute.
No abnormality was found in routine blood, urine analyses, biochemical test and serum tumour markers.
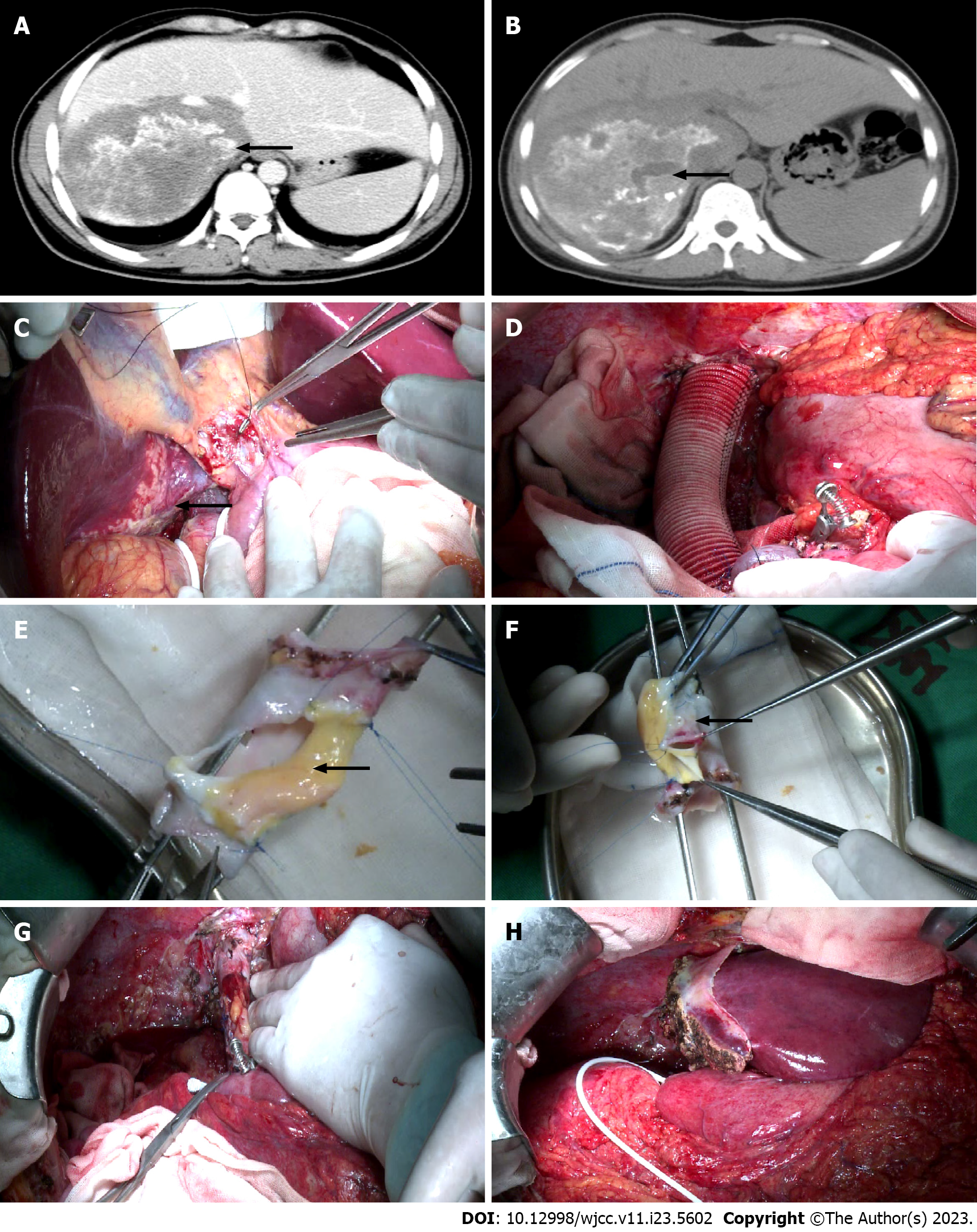
Abdominal color doppler ultrasound revealed a moderate to high echogenic lesion in the right lobe of the liver with a size of approximately 9.5 cm × 8.7 cm. Abdominal computed tomography (CT) revealed space-occupying lesions in the right posterior lobe and the caudate lobe of the liver. The right branch of the PV, the middle hepatic vein (HV), and the initial part of the left HV were invaded. The hepatic IVC was surrounded by lesions and narrowed due to compression (Figure 1A and B).
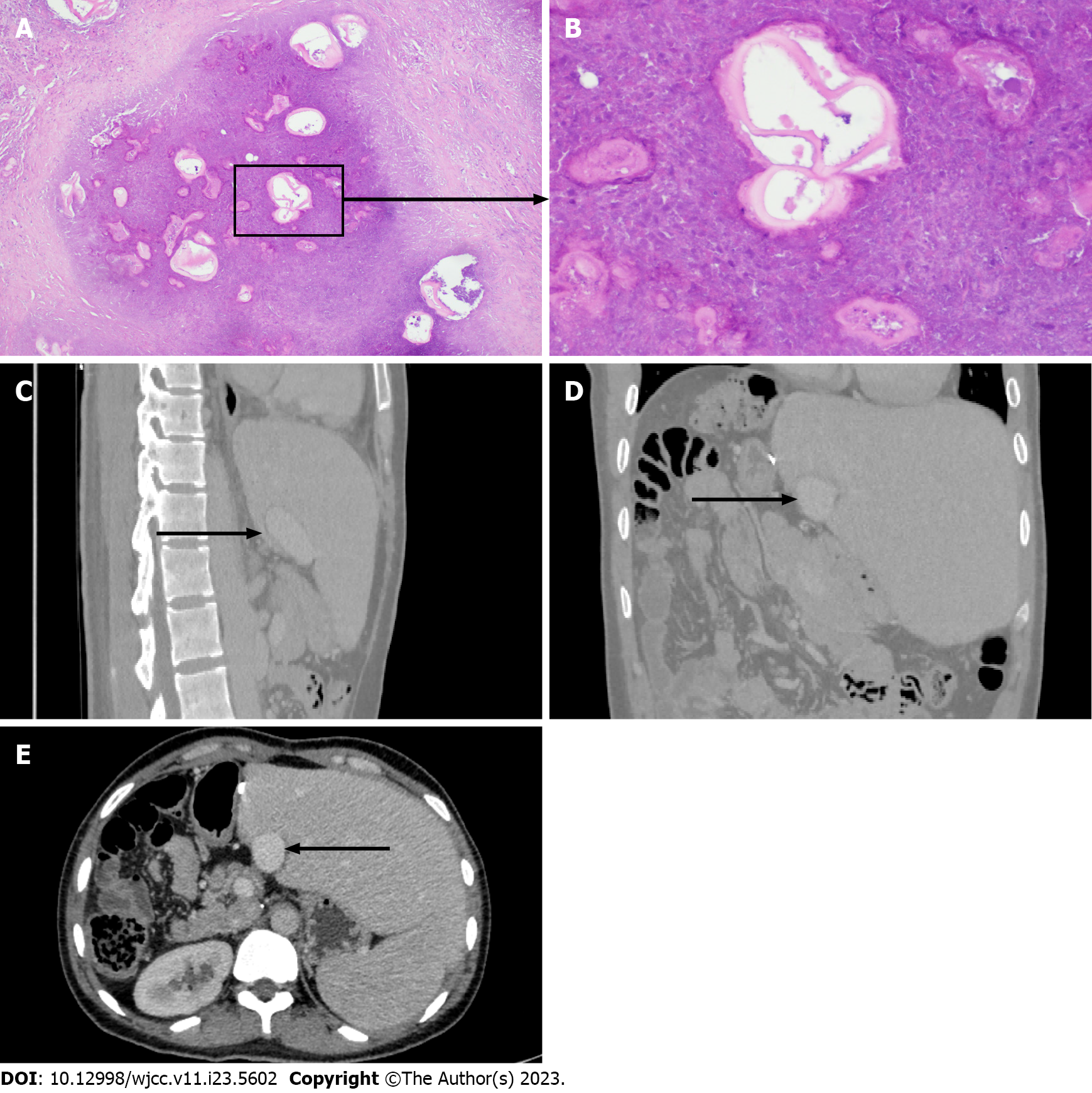
Liver tissues were fixed for more than 24 h and then cut into 5 μm sections after paraffin embedding. Hematoxylin and eosin staining was performed according to the instructions. The staining results showed abundant granulomatous reaction and coagulative necrosis around the laminated parasitic membranes (Figure 2A and B).
Combined with the patient’s medical history, the final diagnosis was hepatic AE (P4N0M0/PI–II, VI–VIII, and I1V1M0).
The patient underwent ELRA. The right posterior lobe of the liver, most of the right anterior lobe, the caudate lobe, and a part of the left inner lobe were invaded. The right HV, the root of the middle HV, and the root of the left HV were encircled, and the anterior and lateral walls of the hepatic IVC were surrounded by a lesion of almost 5 cm in size. After the entire liver was dissociated, the important vascular regions were transected and the infected part of the liver was removed. The hepatic IVC was reconstructed with artificial vessels to perform a temporary portal shunt. The entire liver was isolated and rapidly perfused through the left branch of PV with Histidine–Tryptophan–Ketoglutarate solution at 0 to 4℃. The hepatic parenchyma was severed at 2.0 cm along with the right edge of the falciform ligament, the vessels along the way were ligated, and the lesions that invaded the vessels were removed.
The anterolateral wall of the hepatic IVC was invaded by the lesion. Because the resection of the autograft iliac vein and internal jugular vein can be locally traumatic to the patient, we used the umbilical vein within the LTH, PV fragment, and disease-free IVC to reconstruct the huge defect of the hepatic IVC. The anastomosis between the IVC and artificial blood vessel was dismantled, and end-to-end anastomosis of the upper and lower edges of the repaired hepatic IVC was performed. The PV was anastomosed, which opened all blood vessels and ended the anhepatic phase. End-to-end anastomosis of the right branch of the proper hepatic artery with the trunk type of a proper hepatic artery was performed. Furthermore, Roux-en-Y hepaticojejunostomy was performed to drain the left hepatobiliary duct (Figure 1C-H).
The entire surgery took 14 h and 5 min to complete with stable hemodynamics. The patient had a blood loss of almost 700 mL and was transfused 630 mL of fresh plasma and 528 mL of autologous.
The patient developed pleural effusion 6 d post-surgery, which was treated with a pleural puncture and catheter drainage. Ultrasonography was performed on days 0, 1, 2, 4, and 6, which showed unobstructed blood flow signals in IVC. Regular abdominal CT showed normal visualization of the IVC, no distinct stenosis, and a filled defect. The follow-up time was 84 mo (Table 1). The patient showed good liver functions and no revascularization-related complications during follow-ups. The abdominal CT of the patient showed good filling of the vessels after 84 mo with no obstruction or stenosis (Figure 2C-E).
| Variables | Case 1 |
| Residual liver volume (m3) | 530 |
| RLV/SLV (%) | 46.2 |
| Operation time (h) | 14.08 |
| Cold ischemia time (min) | 403 |
| Warm ischemia time (min) | 18 |
| Anhepatic phase (min) | 421 |
| Time of inferior vena cava occlusion (min) | 122 |
| Blood loss (mL) | 800 |
| Blood transfusion volume | |
| Suspended RBC (units) | 6 |
| Plasma (mL) | 1070 |
| Autotransfusion (mL) | 750 |
| Cryoprecipitate (units) | 0 |
| Platelet (units) | 0 |
| ICU stay time (h) | 65.4 |
| Hospital stays (d) | 35 |
| Postoperative complications | |
| Pulmonary infection | N |
| Pleural effusion | Y |
| Ascites | N |
| Outflow tract stenosis | N |
It's been eight years since the operation, the patient was still alive.
Hepatic AE is a zoonotic infection found worldwide that is caused by Echinococcus multilocularis[14]. It is mainly endemic in the northern hemisphere, especially in western China. Radical surgery is the best approach to treat this condition. However, its diagnosis can be delayed because obvious symptoms are not observed during the early stages. Therefore, patients are sometimes deprived of radical surgery due to the significant invasion of vital blood vessels by the time of diagnosis. Chui et al[15] achieved good results with the first ELRA in 2003. Therefore, this surgery has gradually become an effective approach for treating end-stage hepatic AE. ELRA has garnered increasing attention in recent years owing to its advantages of radical excision of lesions with no requirement of an immunosuppressive agent. Compared with allotransplantation, ELRA has better long-term efficacy for treating end-stage hepatic AE or benign liver tumors[12]. The major challenge in ELRA is repairing and reconstructing the invaded blood vessels in vitro[5,14]. Oldhafer et al[16] proposed in situ hepatic resection and allotransplantation, which facilitate safe and complex revascularization of hepatic lesions that cannot be treated by combined liver surgery. Individual management of revascularization is challenging and crucial for patient prognosis[5].
Sometimes, the defects in the key blood vessels of the healthy side of the liver are too extensive to be repaired and recreated in vivo due to the substantial invasion of end-stage hepatic AE lesions. Therefore, selecting and obtaining proper materials for blood vascular repair is more difficult in ELRA compared with that in allotransplantation. Our center has reported 24 cases of ELRA with revascularization using LTH between August 2010 and October 2018[6]. We have also reported cases of using other vessels, such as internal jugular veins, iliac veins, or artificial vessels, as vascular substitutes[4,5]. However, only a few studies have reported complex revascularization using multiple materials.
In this study, due to the significant area of IVC invasion in the patient, a single vascular material was insufficient for repair and reconstruction. Moreover, blood vessel bank or donation after cardiac death (DCD) vessels was not available during the surgery. In this case, using a range of vascular substitutes that have been proven to be safe was the final option for reconstructing the IVC because of several reasons. Using artificial blood vessels increases the risk of thrombosis and failure of vascular repair and reconstruction[17]. Using a DCD vascular graft requires a blood vessel bank, which is not available in all centers. Autologous vascular grafts are used for vascular reconstruction. Many studies have shown the safety of IVC repair with various autologous venous grafts in allotransplantation[18,19]. The acquisition of autologous vein grafts in other parts of the patient’s body, such as the saphenous vein, and internal jugular vein, require local surgery and cause additional donor-area trauma to the patient. The use of perihepatic vessels, such as LTH and PV, can prevent additional donor-area trauma to the patient and the occurrence of revascularization-related complications because of similar blood vessel endothelium. The patient’s safety was preliminarily validated during the long-term follow-up and no vascular stenosis, thrombosis, or other complications were reported. This study and all previous studies have shown that complex vascular reconstruction, a key technique, opens up new possibilities for the successful implementation of liver transplantation, both liver transplantation and ELRA.
Herein, we reviewed three previous cases with lesions that severely invaded the hepatic IVC and required complex IVC reconstruction. A total of 3 studies with detailed descriptions of 3 cases of complex reconstruct IVC in ELRA were found[20-22]. Table 2 presents the detailed data of these studies (Table 2). Based on the specific data obtained from these studies, the methods for complex reconstruction of the IVC in ELRA were summarized and analyzed. Of the 3 studies, 2 studies were reported from China, and 1 study was from the United Kingdom. These studies reported the complex reconstruction of the IVC in three patients during ELRA. In all three patients, two or more types of blood vessels except IVC were used to reconstruct IVC. The two studies from China reported two patients with hepatic AE who underwent ELRA with the IVC reconstruction. In one patient, the disease-free hepatic IVC, bilateral autologous saphenous veins, and unilateral common iliac vein were used for reconstruction, whereas in the other patient, the bilateral saphenous, inferior, and middle HV, inferior mesenteric vein, and a portion of the lateral wall of the hepatic IVC were used. The United Kingdom study reported a patient with intrahepatic smooth muscle sarcoma during ELRA. The complex reconstruction of the IVC was performed using the left iliac vein of 2 deceased donors and an autologous disease-free IVC from the patient. The postoperative prognosis was good and IVC revascularization-related complications did not occur in all the patients.
| Ref. | Country | Diagnose | Cases | Complex reconstruction of IVC | Reconstructive method | Complications associated with outflow tract reconstruction | Survival |
| Jianyong et al[20], 2015 | China | Alveolar echinococcosis | 1 | 1 | Bilateral great saphenous vein, part of the retro hepatic inferior vena and the middle hepatic vein, the inferior mesenteric vein, part of the infra hepatic vena cava | Not mentioned | 1 |
| Hu et al[21], 2016 | China | Alveolar echinococcosis | 12 | 1 | Disease-free RHIVC, bilateral autogenous great saphenous veins, unilateral common iliac vein | Not mentioned | 11 |
| Buchholz et al[22], 2020 | United Kingdom | Intrahepatic Caval Leiomyosarcoma | 1 | 1 | 2 caval grafts and the left iliac vein of the graft | Not mentioned | 1 |
IVC invasion, huge lesions in the central location, and lesions near the IVC and HV junction are not suitable for surgical resection, and untreated patients have a dismal prognosis[23]. The patient reported in this study benefited from an extracorporeal technique of ELRA and underwent complex revascularization. Ex vivo surgery with complicated revascularization is a complex and challenging technique, which is a new possible treatment for patients with end-stage hepatic AE for whom other conventional treatment options are not available.
The present study has certain limitations. This is a retrospective study of a new case report and 3 previous case reports. Due to the small sample size of this study, future studies with more cases and longer follow-ups should investigate the long-term complications of complex revascularization to verify the safety and feasibility of complex revascularization techniques.
To conclude, we showed that complex IVC reconstruction using autogenous multi-vein fragments is feasible and has a good prognosis during ELRA in patients with end-stage hepatic AE. The use of autologous perihepatic vessels prevents donor-area trauma, immune rejection, and other adverse reactions. When the blood vessel is severely invaded and a single vascular material cannot repair and reconstruct the defect, ELRA may provide a safe and feasible surgical approach for revascularization, which has good prospects for clinical application.
| 1. | Wen H, Vuitton L, Tuxun T, Li J, Vuitton DA, Zhang W, McManus DP. Echinococcosis: Advances in the 21st Century. Clin Microbiol Rev. 2019;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 704] [Article Influence: 100.6] [Reference Citation Analysis (0)] |
| 2. | Kern P, Menezes da Silva A, Akhan O, Müllhaupt B, Vizcaychipi KA, Budke C, Vuitton DA. The Echinococcoses: Diagnosis, Clinical Management and Burden of Disease. Adv Parasitol. 2017;96:259-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 353] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 3. | Wen H, Dong JH, Zhang JH, Zhao JM, Shao YM, Duan WD, Liang YR, Ji XW, Tai QW, Aji T, Li T. Ex vivo liver resection followed by autotransplantation for end-stage hepatic alveolar echinococcosis. Chin Med J (Engl). 2011;124:2813-2817. [PubMed] |
| 4. | Wen H, Dong JH, Zhang JH, Duan WD, Zhao JM, Liang YR, Shao YM, Ji XW, Tai QW, Li T, Gu H, Tuxun T, He YB, Huang JF. Ex Vivo Liver Resection and Autotransplantation for End-Stage Alveolar Echinococcosis: A Case Series. Am J Transplant. 2016;16:615-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 5. | Aji T, Dong JH, Shao YM, Zhao JM, Li T, Tuxun T, Shalayiadang P, Ran B, Jiang TM, Zhang RQ, He YB, Huang JF, Wen H. Ex vivo liver resection and autotransplantation as alternative to allotransplantation for end-stage hepatic alveolar echinococcosis. J Hepatol. 2018;69:1037-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 6. | Jiang T, Ran B, Guo Q, Zhang R, Duan S, Zhong K, Wen H, Shao Y, Aji T. Use of the ligamentum teres hepatis for outflow reconstruction during ex vivo liver resection and autotransplantation in patients with hepatic alveolar echinococcosis: A case series of 24 patients. Surgery. 2021;170:822-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Jiang T, Aji T, Wang Z, Bo R, Guo Q, Zhang R, Tuergan T, Zhong K, Shao Y, Wen H. Reconstruction of hepatic venous outflow and management of its complications using ex vivo liver resection and autotransplantation: a single-center experience. Expert Rev Gastroenterol Hepatol. 2022;16:279-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Hwang R, Liou P, Kato T. Ex vivo liver resection and autotransplantation: An emerging option in selected indications. J Hepatol. 2018;69:1002-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Zhang Y, Lai ECH, Yang C, Yang H, Liu J, Zhou G, Xian D, Deng S, Lau WY. In situ reconstruction of vascular inflow/outflow to left lateral liver section, ex-vivo liver resection and autologous liver transplantation of remaining liver remnant for hepatic alveolar echinococcosis. Int J Surg Case Rep. 2020;69:39-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Yang X, Qiu Y, Huang B, Wang W, Shen S, Feng X, Wei Y, Lei J, Zhao J, Li B, Wen T, Yan L. Novel techniques and preliminary results of ex vivo liver resection and autotransplantation for end-stage hepatic alveolar echinococcosis: A study of 31 cases. Am J Transplant. 2018;18:1668-1679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | Kato T, Hwang R, Liou P, Weiner J, Griesemer A, Samstein B, Halazun K, Mathur A, Schwartz G, Cherqui D, Emond J. Ex Vivo Resection and Autotransplantation for Conventionally Unresectable Tumors - An 11-year Single Center Experience. Ann Surg. 2020;272:766-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Yang X, Wang T, Kong J, Huang B, Wang W. Resection of retrohepatic inferior vena cava without reconstruction in ex vivo liver resection and autotransplantation: a retrospective study. BMC Surg. 2020;20:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Qiu Y, Yang X, Shen S, Huang B, Wang W. Vascular infiltration-based surgical planning in treating end-stage hepatic alveolar echinococcosis with ex vivo liver resection and autotransplantation. Surgery. 2019;165:889-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (2)] |
| 14. | Yang C, Yang HJ, Deng SP, Zhang Y. Current status of ex-vivo liver resection and autologous liver transplantation for end-stage hepatic alveolar echinococcosis. Ann Palliat Med. 2020;9:2271-2278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Chui AK, Island ER, Rao AR, Lau WY. The longest survivor and first potential cure of an advanced cholangiocarcinoma by ex vivo resection and autotransplantation: a case report and review of the literature. Am Surg. 2003;69:441-444. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Oldhafer KJ, Lang H, Schlitt HJ, Hauss J, Raab R, Klempnauer J, Pichlmayr R. Long-term experience after ex situ liver surgery. Surgery. 2000;127:520-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 93] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Thorat A, Jeng LB, Yang HR, Li PC, Li ML, Yeh CC, Chen TH, Hsu SC, Poon KS. Outflow reconstruction for right liver allograft with multiple hepatic veins: "V-plasty" of hepatic veins to form a common outflow channel versus 2 or more hepatic vein-to-inferior vena cava anastomoses in limited retrohepatic space. Liver Transpl. 2016;22:192-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Lee SG. Techniques of reconstruction of hepatic veins in living-donor liver transplantation, especially for right hepatic vein and major short hepatic veins of right-lobe graft. J Hepatobiliary Pancreat Surg. 2006;13:131-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Quinones-Baldrich W, Alktaifi A, Eilber F. Inferior vena cava resection and reconstruction for retroperitoneal tumor excision. J Vasc Surg. 2012;55:1386-93; discussion 1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 20. | Jianyong L, Jingcheng H, Wentao W, Lunan Y, Jichun Z, Bing H, Ding Y. Ex vivo liver resection followed by autotransplantation to a patient with advanced alveolar echinococcosis with a replacement of the retrohepatic inferior vena cava using autogenous vein grafting: a case report and literature review. Medicine (Baltimore). 2015;94:e514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Hu H, Huang B, Zhao J, Wang W, Guo Q, Ma Y. Liver autotransplantation and retrohepatic vena cava reconstruction for alveolar echinococcosis. J Surg Res. 2017;210:169-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Buchholz BM, Pinter Carvalheiro da Silva Boteon A, Taniere P, Isaac JR, Gourevitch D, Muiesan P. Autotransplantation of the Liver for Ex Vivo Resection of Intrahepatic Caval Leiomyosarcoma: A Case Report. Exp Clin Transplant. 2020;18:396-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Baker MA, Maley WR, Needleman L, Doria C. Ex vivo resection of hepatic neoplasia and autotransplantation: a case report and review of the literature. J Gastrointest Surg. 2015;19:1169-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Transplantation
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Amante MF, Argentina; Uhlmann D, Germany S-Editor: Liu JH L-Editor: A P-Editor: Liu JH