Published online May 6, 2023. doi: 10.12998/wjcc.v11.i13.2945
Peer-review started: February 27, 2023
First decision: March 10, 2023
Revised: March 19, 2023
Accepted: March 24, 2023
Article in press: March 24, 2023
Published online: May 6, 2023
Processing time: 57 Days and 1.9 Hours
Ectopic pregnancy (EP) is one of the most common acute abdominal diseases in gynecology. Once the condition of EP is delayed, it may lead to massive hemo
To explore the application value of TAS and TVS in the diagnosis of EP and to improve the level of clinical diagnosis.
A total of 140 patients with EP admitted to our hospital from July 2018 to July 2020 were selected for this study. All patients were divided into two groups according to the examination methods. 63 patients who underwent abdominal ultrasound examination were set as the TAS group, while 77 patients who underwent TVS examination were set as the TVS group. We compared the diagnostic accuracy and misdiagnosis rates between the two types of ultrasound examinations, as well as the postoperative pathological results of the two diagnostic methods for different types of ectopic pregnancies. We also analyzed the sonograms for the presence of mixed ectopic masses, adnexal masses, ectopic gestational sacs, the presence or absence of visible embryo and fetal heart in the ectopic sac shadow, and the detection of fluid in the rectal fossa of the uterus, such as the adnexal area, yolk sac, and embryo, etc. In addition, the diagnosis time, days of gestational sac appearance, operation time, endometrial thickness, and blood flow resistance index were compared as well.
After performing both types of ultrasound examinations in 140 patients with EP, we found that the diagnostic accuracy of TVS was significantly higher than that of TAS, and the misdiagnosis rate was significantly lower than that of TAS. The differences were statistically significant (P < 0.05). In addition, the detection rate of TVS was better than that of TAS for the presence of mixed masses, adnexal masses, ectopic gestational sacs, the presence or absence of visible embryo and fetal heart in the shadow of the ectopic sac, and sonograms such as the adnexal area, yolk sac, and embryo, etc. The coincidence rate of its postoperative pathological examination results was significantly higher than those of TAS. The diagnosis time and the days of gestational sac appearance by TVS were significantly shorter than that by TAS, and the operation time was earlier than that by TAS. What’s more, the detection rates of the endometrial thickness £ 1.5 mm and blood flow resistance £ 0.5 were significantly higher in TVS diagnosis of EP than in TAS. All differences were statistically significant (P < 0.05).
Compared with TAS, TVS has the advantages of high detection accuracy and good sonogram performance.
Core Tip: Transabdominal ultrasound (TAS) is the primary method for early detection of ectopic pregnancy (EP). However, because of the low frequency of the TAS probe and the certain distance between it and the gestational sacs, it is susceptible to interference of the probe acquisition data by factors such as the filling bladder, abdominal fat, abdominal wall trabecular contents, and intestinal wall, which further reduces the accuracy of diagnosis. With the development of clinical diagnostic technology and the improvement of the medical level, transvaginal ultrasound (TVS) is gradually applied in the diagnosis of various clinical fields. Based on this, this study aims to compare and analyze the application value of TAS and TVS in the diagnosis of EP, hoping to provide some help for the early diagnosis and treatment of EP.
- Citation: Hu HJ, Sun J, Feng R, Yu L. Comparison of the application value of transvaginal ultrasound and transabdominal ultrasound in the diagnosis of ectopic pregnancy. World J Clin Cases 2023; 11(13): 2945-2955
- URL: https://www.wjgnet.com/2307-8960/full/v11/i13/2945.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i13.2945
Ectopic pregnancy (EP) is one of the common acute abdominal diseases in gynecology, which mainly refers to the implantation of fertilized eggs outside the uterine cavity[1,2]. There are many causes of EP, such as pelvic inflammation, pelvic effusion, fallopian tube abnormalities, etc[3]. EP can be divided into tubal pregnancy, ovarian pregnancy, and cervical pregnancy according to the different locations of fertilized eggs implanted outside the uterine cavity, among which EP accounts for more than 95%[4]. Menopause, abdominal pain, and vaginal bleeding are the typical clinical manifestations of EP, especially tubal pregnancy. As a result of acute intra-abdominal bleeding and severe abdominal pain, mild cases of fainting can lead to shock and even death in severe cases, seriously threatening the lives of patients[5,6]. Therefore, improving the diagnostic accuracy of EP can help patients get timely treatment and effectively guarantee their prognosis.
At present, there are many methods to diagnose EP, such as pregnancy test, ultrasound diagnosis, posterior fornix puncture, laparoscopy, endometrial pathology examination, etc.[7], among which transabdominal ultrasound (TAS) has become a common clinical examination method because of its convenience and quick operation. However, due to factors such as the thickness of human abdominal sebum and the low frequency of the probe, misdiagnosis and missed diagnosis of abdominal ultrasound is inevitable. Therefore, it is very important to find a more efficient and accurate method for the diagnosis of EP. Transvaginal ultrasound (TVS) is a kind of intracavitary ultrasound, which requires a special vaginal probe to be placed directly in the vagina for an ultrasound examination. As a technological breakthrough in the application of obstetrical and gynecological ultrasound in recent years, compared with traditional TAS, it can clearly show the internal organ and tissue structure of the female pelvic cavity without filling the bladder. It has early and accurate characteristics for the diagnosis of normal and abnormal pregnancies and gynecological diseases[8]. Previous studies have found that TVS examination of EP can improve diagnostic accuracy and ensure the timely treatment of patients[9]. In addition, studies by Mei et al[10] have shown that TAS and TVS are the main diagnostic methods for abdominal diseases, especially in the early diagnosis of EP[11-12].
Based on this, this study aims to explore the application value and effect of TAS and TVS in the diagnosis of EP through retrospective analysis of clinical data of patients with EP, hoping to provide more valuable references for the diagnosis of EP.
In this study, 140 patients with EP admitted to our hospital from July 2018 to July 2020 were selected. All patients ranged in age from 21 to 39 years, among which 82 were primiparas, and 58 were multiparas. All patients understood the content of the study and voluntarily signed the informed consent form. According to different examination methods, we divided the 140 patients into two groups: 63 patients in the TAS group were diagnosed with TAS and 77 patients in the TVS group were diagnosed with transvaginal color Doppler ultrasound. The general data of all patients were compared and the differences were not statistically significant (P > 0.05), as shown in Table 1.
| Group | Age (years), mean ± SD | Multiparas | Primipara | Urine HCG (weak) positive | Blood HCG (weak) positive |
| TAS group (n = 63) | 35.57 ± 3.65 | 24 (38.10) | 39 (61.90) | 58 (92.06) | 60 (95.23) |
| TVS group (n = 77) | 35.56 ± 3.78 | 34 (44.16) | 43 (55.84) | 72 (93.51) | 75 (97.40) |
| T/χ2 | 0.017 | 0.581 | 0.399 | ||
| P value | 0.987 | 0.469 | 0.310 | ||
Inclusion criteria: All patients were tested for β-humanchorionic gonadotrophin, and the results were positive or weakly positive. Patients were diagnosed with EP according to the clinical symptoms and pathological features; patients had no history of EP and no other gynecological diseases.
Exclusion criteria: Patients with intrauterine abortion, ovarian cyst torsion, and acute tubal infection[13]; patients with vaginal inflammation or other contraindications to vaginal examination; patients with severe mental illness or communication disorders; patients who do not actively cooperate with the examination.
In the TAS Group, we adopted the Philips HD7 ultrasound diagnostic instrument. Before the operation, the patients were instructed to drink more water to make the bladder fill properly. Patients were placed in a supine position. The probe frequency was 3.5-5 MHz. Patients were then scanned from the pubic bone to the upper abdomen at multiple angles after applying a coupling agent on the probe tip. The focus was placed on uterine volume, uterine cavity, endometrial thickness, bilateral adnexa, and other pelvic organs[14].
In the TVS group, a Voluson 730 expert color Doppler ultrasound instrument from GE company was used, and the TVS probe frequency was 3.0-10.0 MHz. The patients were instructed to perform a vaginal ultrasound examination after complete urination and they were placed in a lithotomy position. The probe tip was coated with a coupling agent and then wrapped in a condom and slowly placed into the vagina and tightly pressed against the posterior vaginal fornix. The probe handle was slowly rotated, and a multi-directional and multi-sectional scan was performed with a focus on uterine volume, uterine cavity, endometrial thickness, bilateral adnexa, and other pelvic organs[15].
Two diagnostic methods were used to observe the presence of uterine gestational sac, adnexal gestational sac mass, extrauterine gestational sac, and cardiovascular pulsation, the presence of visible embryo and fetal heart in the external gestational sac shadow, and fluid accumulation in the rectal fossa of the uterus. In addition, the endometrial shape and blood flow were also focused on. Continuous scanning was performed to clearly show the shape of the uterine orifice to the endometrial fundus. The thickest part of the endometrial thickness was measured in a longitudinal section, and pulsed Doppler was performed at the most brightly colored areas of color Doppler flow imaging to record the endometrial thickness and blood flow resistance, and the results of TAS and vaginal ultrasound were compared and analyzed.
Analysis of the testing accuracy of TAS and TVS: Ultrasound diagnostic criteria for EP[16-18]: (1) Tubal pregnancy: During the examination, there are no gestational sacs in the uterus, a hypoechoic area appears next to the uterus, and cardiovascular pulsations and embryo can be detected inside it; (2) Ovarian pregnancy: No gestational sac in the uterus, enlarged ovaries, hypoechoic area inside, and gestational sac can be detected inside; (3) Cervical pregnancy: No gestational sacs in the uterus, enlarged cervix, gestational sac can be detected inside; (4) Cornual pregnancy: No gestational signs in the uterine cavity, and the horn of the uterus is protruding, there is a muscle wall outside the gestational sac, and cardiovascular pulsation and embryo can be detected inside; (5) Uterine stump pregnancy: There is no gestational sac in the uterus, but there is a hypoechoic area outside the uterus where the gestational sac can be detected and the placental echo can be seen and fetal activity can be detected; and (6) Abdominal pregnancy: The uterine body is enlarged and cardiovascular pulsations and embryo can be detected in the upper uterus. Diagnostic accuracy = (tubal pregnancy + ovarian pregnancy + cervical pregnancy + abdominal pregnancy + uterine stump pregnancy) / total number of cases.
Analysis of the coincidence rate of TAS and TVS on the pathological findings of EP after surgery: The laparoscopic surgery can effectively magnify the fallopian tube under the video screen to quickly locate the pregnancy location. Using laparoscopic findings as the gold standard for the diagnosis of EP, we compared the coincidence rate between TAS and TVS for postoperative pathological findings of EP in different pregnancy types, including tubal pregnancy, ovarian pregnancy, cervical pregnancy, scarred uterine pregnancy, abdominal pregnancy, and uterine stump pregnancy.
Observation of ultrasound sonographic performance in the diagnosis of EP in two groups of patients: According to the characteristics of the ultrasound image, it can be divided into the following types: (1) Mixed mass: The mixed echogenic mass with uneven density can be seen in the pelvic cavity, mainly cystic, with irregular solid echogenicity and coarse septum; (2) Gestational sac-viable type: A ring-like hyperechoic mass similar to the gestational sac can be seen in the adnexal area, which is a small fluid hyperechoic area, and yolk sac, embryo bud, and original cardiac pulsation can be seen in some types of the gestational sac; (3) Adnexal mass: Solid masses with blurred contours and varying intensity of internal echogenicity can be seen in the parametrium due to clotting plan and adhesion to surrounding tissues, which may be accompanied by a small amount of pelvic fluid; and (4) Utero-rectal fossa fluid: The utero-rectal fossa is the space between the uterus and the rectum, the lowest position in the female pelvis. When there is a small amount of exudate from the pelvic viscera and the patient has ruptured bleeding or pelvic inflammatory disease, the fluid will first accumulate in the pelvic cavity, thus forming pelvic fluid. The sonographic presentation of the different types of EP described above was compared by observing ultrasound image analysis of TAS and TVS.
Comparison of the accuracy of TAS and TVS in the diagnosis of EP: The accuracy of TAS and TVS in diagnosing EP was compared by analyzing the diagnosis time of EP, the days of the gestational sac appearance, and the operation time using an ultrasound diagnostic device.
Comparison of endometrial thickness and blood flow resistance detection in patients with EP: The patients were examined by abdominal b-mode ultrasound and transvaginal b-mode ultrasound respectively using B-mode ultrasound diagnostic instrument. The endometrial thickness and the blood flow resistance index in the mass were measured accurately, and the diagnostic accuracy of TAS and TVS in EP was analyzed.
In this study, we adopted IBM SPSS 21.0 software (SPSS Inc., Chicago, IL, USA) to process and analyze all the data. The measurement data were expressed as mean ± SD and a t-test was used for comparison between groups. The count data were expressed as n (%) and the χ2 test was used for comparison. All the differences were statistically significant at P < 0.05.
We observed the detection rate of positive EP in the two groups after different ultrasound diagnoses and found that the accuracy rate of transvaginal color Doppler ultrasound was significantly higher (97.40%) than that of TAS (88.89%), and its misdiagnosis rate (2.60%) was significantly lower than that of TAS (11.11%), which was statistically significant (P < 0.05). This indicates that the accuracy of transvaginal color Doppler ultrasound in the diagnosis of EP is better (Table 2).
| Group | Consistent with the diagnosis | Misdiagnosis | Accuracy rate |
| TAS group (n = 63) | 56 | 7 | 88.89 |
| TVS group (n = 77) | 75 | 2 | 97.40 |
| χ2 | 0.090 | 0.036 | |
| P value | 0.041 | 0.017 | |
We further compared and analyzed the coincidence rate between TAS and TVS on the postoperative pathological results of ectopic pregnancies of different pregnancy types, such as tubal pregnancy, ovarian pregnancy, cervical pregnancy, scarred uterine pregnancy, abdominal pregnancy, and uterine stump pregnancy. It was found that the coincidence rate of postoperative pathological examination by transvaginal B-mode ultrasound was better than that by TAS, and the difference was statistically significant (P < 0.05), especially in the diagnosis of postoperative pathological examination results of a tubal pregnancy (Table 3).
| Type | Consistent with the diagnosis | TAS group | TVS group | χ2 | P |
| Ovarian pregnancy | 58 | 54 (93.10) | 56 (96.55) | - | - |
| Tubal pregnancy | 20 | 7 (35.00) | 16 (80.00) | 0.011 | 0.004 |
| Cervical pregnancy | 15 | 13 (86.67) | 13 (86.67) | - | - |
| Scarred uterine pregnancy | 12 | 10 (83.33) | 11 (91.67) | - | - |
| Abdominal pregnancy | 11 | 10 (90.91) | 11 (100.00) | - | - |
| Uterine stump pregnancy | 9 | 8 (88.89) | 8 (88.89) | - | - |
| Cornual pregnancy | 15 | 13 (86.67) | 14 (93.33) | - | - |
| Total | 140 | 115 (82.14) | 129 (92.14) | 0.020 | 0.012 |
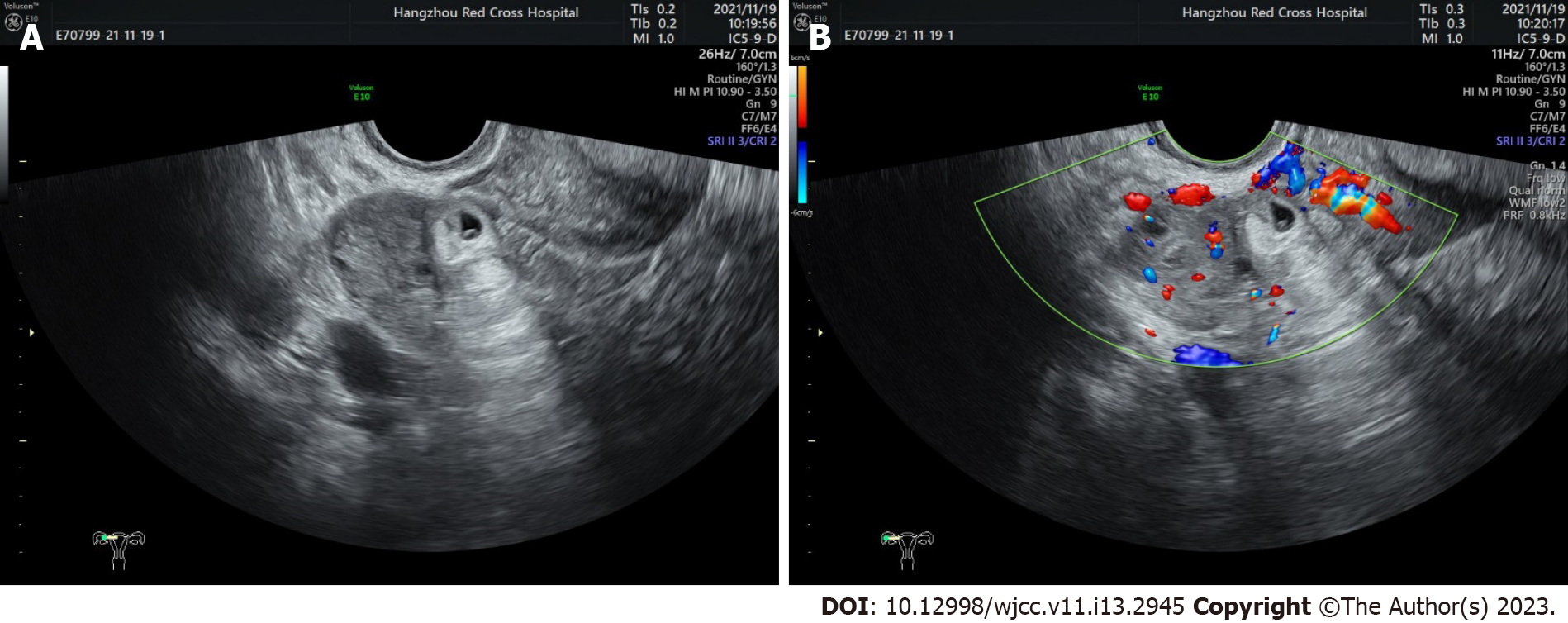
In an EP, the uterus is significantly enlarged on ultrasound, but the uterine cavity is empty, and a hypoechoic area next to the uterus or a gestational sac or fetal heart, or embryo can be seen. The EP can also be determined by the protrusion of the uterine horn on one side of the uterus, localized thickening of the muscular layer, and the presence of a visible gestational sac. To further investigate the value of vaginal ultrasound and TAS in the diagnosis of EP, we compared the sonograms of the two kinds of ultrasound diagnosis and found that compared with TAS, transvaginal color Doppler ultrasound could more clearly observe the ectopic gestational sac shadow, the presence of mixed masses, and the presence of fetal heart and embryo, the adnexal area, and the yolk sac. The difference between the two groups was statistically significant (P < 0.05), (Table 4, Figure 1).
| TAS group (n = 63) | TVS group (n = 77) | χ2 | P | |
| Extrauterine mixed mass | 17 (26.98) | 34 (44.16) | 0.054 | 0.036 |
| Ectopic gestational sac shadow | 43 (68.25) | 65 (84.42) | 0.039 | 0.023 |
| Uterine rectal fossa fluid | 15 (23.81) | 8 (10.39) | 0.057 | 0.033 |
| Fetal heart and embryo in the shadow of ectopic gestational sac | 45 (71.43) | 66 (85.71) | 0.062 | 0.038 |
| Adnexal area | 12 (19.05) | 27 (35.06) | 0.056 | 0.035 |
| Yolk sac | 52 (82.54) | 73 (94.81) | 0.039 | 0.020 |
| Consistent with the diagnosis | 152 (82.61) | 231 (84.62) | 0.062 | 0.045 |
It was found that the diagnosis time of EP and the days of gestational sac appearance in the transvaginal B-mode ultrasound group were shorter than those in the control group. At the same time, the operation time of the transvaginal B-mode ultrasound group was earlier than that of the transabdominal B-mode ultrasound group (P < 0.05). The results showed that TVS could diagnose EP earlier and the operation could be performed earlier to enhance the therapeutic effect (Table 5).
| Group | Diagnosis time | Days of gestational sac appearance | Operation time |
| TAS group (n = 63) | 38.24 ± 6.27 | 32.56 ± 5.35 | 42.33 ± 4.65 |
| TVS group (n = 77) | 34.56 ± 6.21 | 28.67 ± 5.54 | 32.59 ± 4.31 |
| T | 3.473 | 4.197 | 12.838 |
| P value | < 0.001 | < 0.001 | < 0.001 |
It was found that the detection rate of endometrial thickness ≤ 1.5 mm and blood flow resistance ≤ 0.5 in TVS diagnosis of EP was significantly higher than that in TAS diagnosis, and the difference was statistically significant (P < 0.05). This indicated that TVS could more accurately predict the site of pregnancy, identify the blood flow resistance index, and improve the diagnosis rate of EP (Table 6).
| Detection Method | Endometrial thickness | Blood flow resistance in the endometrium | ||
| ≤ 1.5 mm | ≥ 1.5 mm | ≤ 0.5 | ≥ 0.5 | |
| TAS group (n = 63) | 36 (57.14) | 27 (42.86) | 24 (38.10) | 39 (61.90) |
| TVS group (n = 77) | 46 (59.74) | 31 (40.26) | 43 (55.84) | 34 (44.16) |
| χ2 | 1.096 | 4.374 | ||
| P value | 0.019 | 0.036 | ||
In normal pregnancy, the fertilized eggs are deposited in the uterine cavity, whereas in EP, the fertilized eggs are deposited outside the uterine cavity and grow and develop[19-21]. In the early stage of EP, there is no obvious clinical manifestation, some patients present with menopause, abdominal pain, and a small amount of vaginal bleeding. Patients often suffer from acute severe abdominal pain, and recurrent episodes, and are more painful at the onset. However, there are still some patients with EP who do not have typical clinical symptoms, and the diagnosis rate is low at the early stage, which undoubtedly increases the difficulty of clinical diagnosis. And once the condition is delayed, it may lead to hemorrhage, even shock, and death in a short period[22-24]. Therefore, the principle of treatment for EP is early diagnosis and early treatment.
At present, EP is mainly treated clinically by surgery, which presupposes scientific and accurate clinical judgment[25,26]. It has been reported that ultrasound diagnosis has become the main method for early diagnosis of patients with EP because of its convenience, noninvasiveness, and freedom from the pain of diagnostic curettage and fornix puncture[27]. TAS was an earlier method of clinical diagnosis. EP is diagnosed when the diagnostic TAS image shows an increase in the thickness of the endometrium, the absence of a gestational sac in the uterine cavity, a mixed mass with uneven echogenic borders on the side of the uterus, or even a mass of gestational sac, embryo or even primitive ventricular pulsation on the side of the uterine cavity in some patients[28,29]. But TAS requires the patient to have a full bladder, and it is far away from the uterus and fallopian tube, which makes lesion detection unclear or incomplete and also prone to misdiagnosis. As a result, the application of TAS is not very ideal, and cannot improve the detection rate of clinical diagnosis.
With the development of clinical diagnosis technology and the improvement of the medical level, ultrasonic equipment and examination technology have also developed. Transvaginal ultrasonography is gradually being used in the diagnosis of various clinical fields[30,31]. Studies have shown that TVS has a higher sensitivity in the diagnosis of EP (especially in the early stage of tubal pregnancy, where there is little internal bleeding and the non-echogenic area is confined to the rectum fossa and around the uterus)[32]. TVS allows the probe to be placed into the vagina, which is closer to the pelvic tissues and organs, and can significantly reduce the interference of gas and fatty tissue in the abdominal cavity, making the uterus and ovaries appear clearer[33,34]. Calì et al[35] also found that TVS does not require the patient to have a full bladder during the diagnosis, which is suitable for the examination of gynecological emergencies, thus saving time for patients with ruptured EP-type hemorrhage. Based on this, this study aimed to compare the value of TAS and TVS in the diagnosis of EP, hoping to provide some help for the early diagnosis and treatment of EP.
In this study, TAS and TVS were performed on 140 patients with EP. The diagnostic accuracy of TVS was 97.40%, which was significantly higher than the 88.89% accuracy of TAS, and its misdiagnosis rate was significantly lower than that of TAS. In addition, a comparative sonogram analysis revealed that a transvaginal Doppler sonography was able to show more clearly the ectopic gestational sac shadow, mixed masses, and the presence of fetal heart and embryo in the ectopic sac shadow. The main reason may be that the resolution of the TVS probe is higher than that of TAS, and the penetration of the probe is stronger, which can clearly show the changes in the uterine cavity and endometrium, and accurately reflect the situation of adnexal masses. In addition, the TVS probe is directly placed into the patient’s vagina and is closer to the uterus, which is less likely to be affected by other factors[36]. In contrast, the abdominal ultrasound probe has a lower frequency and is at a certain distance from the gestational sac, so it is easy to be interfered with by factors such as the filling bladder, abdominal fat, abdominal wall invasive bowel contents, and the bowel wall, etc., thus reducing the accuracy of diagnosis[37,38].
Previous studies have shown that when there is no specificity in the sonogram of adnexal masses, special trophoblast blood flow can be formed after implantation with the help of color Doppler flow imaging, and low resistance flow can be detected in nonspecific adnexal masses that separate from the ovary, thus improving the sensitivity and specificity of EP diagnosis[39,40]. In this study, by comparing and analyzing the diagnostic time and the days of gestational sac appearance between TAS and vaginal ultrasound, it was also found that the diagnostic time of TVS for EP and the days of showing the gestational sac were significantly shorter than that of TAS, and the operation time was significantly earlier than that of TAS. This may be related to the fact that TAS requires more than 5 wk of menopause for detection, whereas TVS can detect the gestational sac within 3-30 d of menopause[41]. This suggests that TVS is more accurate and sensitive in detecting EP compared to TAS, which is consistent with the study by Ramanan et al[42]. That is to say, TVS can detect EP more accurately and its diagnostic time and days of gestational sac appearance are shorter, allowing for earlier surgical treatment options. Timely diagnosis and surgery can enhance the outcome of treatment and reduce the risk of postoperative hemorrhage, which undoubtedly increases the value of TVS and makes it more suitable for use in the diagnosis of gynecologic emergencies. In addition, our results showed that the postoperative pathological findings are more consistent with TVS than with TAS and that its postoperative diagnosis of tubal pregnancy is particularly typical, which may be related to the fact that tubal pregnancy accounts for more than 95% of ectopic pregnancies[43].
It has been found that ultrasound sonograms can reflect cyclic changes in the thickness of endometrial morphology from linear and progressive thickening in the early stages of hyperplasia to 7-10 mm in the late stages of secretion. Since the blood supply and chorionic villus development vary depending on the location of the implanted egg, making differences in the corresponding hormones and the thickness of the endometrium which directly influenced by them. Thus, a combination of endometrial thickness detection can predict the site of pregnancy and improve the accuracy of EP[44,45]. The resistance encountered by blood as it flows through the blood vessels is called blood flow resistance. Blood flow resistance is reported to be caused by energy consumption due to friction during blood flow, and increased blood flow resistance is mainly due to the influence of blood viscosity. Any factor that increases the viscosity of blood has a high potential to increase peripheral resistance and increase blood pressure, thus increasing cardiac burden. Therefore, monitoring the mass flow resistance index may improve diagnostic rates[46,47]. Based on this, we compared the endometrial thickness and blood flow resistance under two different ultrasound diagnoses. It was found that the detection rates of endometrial thickness ≤ 1.5 mm and blood flow resistance ≤ 0.5 were significantly higher in TVS diagnosis of EP than in TAS diagnosis, which is also consistent with previous studies[48]. That is to say, TVS can more accurately predict the location of the pregnancy, identify the blood flow resistance index, and improve the diagnostic rate of EP. This is related to the higher resolution and better penetration of the TVS probe, which allows for clearer visualization of the uterine cavity, endometrial changes, and blood flow. Our research also has certain limitations, the included sample size was limited, and the findings still need more multicentered studies with large samples for further confirmation. In addition, this is a retrospective study, a prospective study using these two scans for pregnant women is the next step to be undertaken.
To sum up, compared with TAS, TVS has higher diagnostic accuracy, clearer image quality, higher accuracy, and specificity in the diagnosis of EP, and is worthy of widespread promotion in the clinical setting. Of course, abdominal ultrasound also has its advantages, but it should be avoided especially for clinical use in patients with combined vaginal and intrauterine inflammation to further avoid infection aggravation. Therefore, the clinical diagnosis of EP needs to be tailored to the patient’s actual situation so that the most suitable detection method can be adopted. As for the effect of combined treatment on the positive diagnosis rate, we will further explore this in the follow-up study.
Ectopic pregnancy (EP) is the leading cause of pregnancy related deaths in the first trimester. Transvaginal ultrasound (TVS) is the key to diagnosis of EP.
140 patients with EP who underwent transabdominal ultrasound (TAS) and TVS were reviewed. The application value of TAS and TVS in the diagnosis of EP was discussed, and the difference between TAS and TVS was compared.
To explore the application value of TAS and TVS in the diagnosis of EP and improve the clinical diagnosis level of EP.
140 patients with EP who received TAS and TVS were analyzed retrospectively. The diagnostic accuracy and misdiagnosis rate of the two kinds of ultrasound examination were compared.
The results showed that the diagnostic accuracy of TVS was significantly higher than that of TAS, and the misdiagnosis rate of TVS was lower than that of TAS, the difference was statistically significant (P < 0.05).
For the diagnosis of EP, TVS is more accurate than TAS.
Compared with TAS, TVS has higher accuracy in the diagnosis of EP, and is more safe and accurate in clinical practice, which is worthy of extensive clinical promotion.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Berardi R, Italy; Dong-Wook K, South Korea S-Editor: Liu XF L-Editor: A P-Editor: Yuan YY
| 1. | Tonick S, Conageski C. Ectopic Pregnancy. Obstet Gynecol Clin North Am. 2022;49:537-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 2. | Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin No. 191: Tubal Ectopic Pregnancy. Obstet Gynecol. 2018;131:e65-e77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 115] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 3. | Yoder N, Tal R, Martin JR. Abdominal ectopic pregnancy after in vitro fertilization and single embryo transfer: a case report and systematic review. Reprod Biol Endocrinol. 2016;14:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 4. | Belics Z, Gérecz B, Csákány MG. Early diagnosis of ectopic pregnancy. Orv Hetil. 2014;155:1158-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Lipscomb GH. Ectopic pregnancy. Foreword. Clin Obstet Gynecol. 2012;55:375. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Rana P, Kazmi I, Singh R, Afzal M, Al-Abbasi FA, Aseeri A, Khan R, Anwar F. Ectopic pregnancy: a review. Arch Gynecol Obstet. 2013;288:747-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Shen Z, Liu C, Zhao L, Xu L, Peng B, Chen Z, Li X, Zhou J. Minimally-invasive management of intramural ectopic pregnancy: an eight-case series and literature review. Eur J Obstet Gynecol Reprod Biol. 2020;253:180-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Shi L, Huang L, Liu L, Yang X, Yao D, Chen D, Xiong J, Duan J. Diagnostic value of transvaginal three-dimensional ultrasound combined with color Doppler ultrasound for early cesarean scar pregnancy. Ann Palliat Med. 2021;10:10486-10494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Dal Moro F, De Gobbi A, Crestani A. Transvaginal ultrasound and ureteral stones. Ultrasound Obstet Gynecol. 2013;42:244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Mei JY, Afshar Y, Platt LD. First-Trimester Ultrasound. Obstet Gynecol Clin North Am. 2019;46:829-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Scibetta EW, Han CS. Ultrasound in Early Pregnancy: Viability, Unknown Locations, and Ectopic Pregnancies. Obstet Gynecol Clin North Am. 2019;46:783-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Stamilio D, Carlson LM. Transabdominal ultrasound is appropriate. Am J Obstet Gynecol. 2016;215:739-743.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 13. | Plett SK, Poder L, Brooks RA, Morgan TA. Transvaginal Ultrasound-Guided Biopsy of Deep Pelvic Masses: How We Do It. J Ultrasound Med. 2016;35:1113-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Pedersen JK, Sira C, Trovik J. Handheld transabdominal ultrasound, after limited training, may confirm first trimester viable intrauterine pregnancy: a prospective cohort study. Scand J Prim Health Care. 2021;39:123-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Liu JX, Li JY, Zhao XY, Zhang QH, Cao Y, Huang XJ, Sun XF, Xie YL, Zhang ST, Yang SS. Transvaginal ultrasound- and laparoscopy-guided percutaneous microwave ablation for adenomyosis: preliminary results. Int J Hyperthermia. 2019;36:1233-1238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 16. | Duchatel FC. Ectopic pregnancy. Curr Opin Obstet Gynecol. 1995;7:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Naveed AK, Anjum MU, Hassan A, Mahmood SN. Methotrexate vs expectant management in ectopic pregnancy: a meta-analysis. Arch Gynecol Obstet. 2022;305:547-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Moore L. Ectopic pregnancy. Nurs Stand. 1998;12:48-53; quiz 54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Solima E, Luciano AA. Ectopic pregnancy. Ann N Y Acad Sci. 1997;828:300-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | Carson SA, Buster JE. Ectopic pregnancy. N Engl J Med. 1993;329:1174-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 101] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Shaw JL, Diamandis EP, Horne AW, Barnhart K, Bourne T, Messinis IE. Ectopic pregnancy. Clin Chem. 2012;58:1278-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Walker JJ. Ectopic pregnancy. Clin Obstet Gynecol. 2007;50:89-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 23. | Al-Jabri S, Malus M, Tulandi T. Ectopic pregnancy. BMJ. 2010;341:c3770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Islam A, Fawad A, Shah AA, Jadoon H, Sarwar I, Abbasi AU. Analysis Of Two Years Cases Of Ectopic Pregnancy. J Ayub Med Coll Abbottabad. 2017;29:65-67. [PubMed] |
| 25. | Hendriks E, Rosenberg R, Prine L. Ectopic Pregnancy: Diagnosis and Management. Am Fam Physician. 2020;101:599-606. [PubMed] |
| 26. | Marion LL, Meeks GR. Ectopic pregnancy: History, incidence, epidemiology, and risk factors. Clin Obstet Gynecol. 2012;55:376-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 162] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 27. | Richardson A, Gallos I, Dobson S, Campbell BK, Coomarasamy A, Raine-Fenning N. Accuracy of first-trimester ultrasound in diagnosis of tubal ectopic pregnancy in the absence of an obvious extrauterine embryo: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2016;47:28-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 28. | Bobdiwala S, Saso S, Verbakel JY, Al-Memar M, Van Calster B, Timmerman D, Bourne T. Diagnostic protocols for the management of pregnancy of unknown location: a systematic review and meta-analysis. BJOG. 2019;126:190-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 29. | Hsu S, Euerle BD. Ultrasound in pregnancy. Emerg Med Clin North Am. 2012;30:849-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Andres MP, Borrelli GM, Ribeiro J, Baracat EC, Abrão MS, Kho RM. Transvaginal Ultrasound for the Diagnosis of Adenomyosis: Systematic Review and Meta-Analysis. J Minim Invasive Gynecol. 2018;25:257-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 116] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 31. | Dueholm M, Lundorf E. Transvaginal ultrasound or MRI for diagnosis of adenomyosis. Curr Opin Obstet Gynecol. 2007;19:505-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 122] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 32. | Liu L, Li W, Leonardi M, Condous G, Da Silva Costa F, Mol BW, Wong L. Diagnostic Accuracy of Transvaginal Ultrasound and Magnetic Resonance Imaging for Adenomyosis: Systematic Review and Meta-Analysis and Review of Sonographic Diagnostic Criteria. J Ultrasound Med. 2021;40:2289-2306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 33. | Kirk E. Ultrasound in the diagnosis of ectopic pregnancy. Clin Obstet Gynecol. 2012;55:395-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 34. | Casikar I, Reid S, Condous G. Ectopic pregnancy: Ultrasound diagnosis in modern management. Clin Obstet Gynecol. 2012;55:402-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 35. | Calì G, Timor-Tritsch IE, Palacios-Jaraquemada J, Monteaugudo A, Buca D, Forlani F, Familiari A, Scambia G, Acharya G, D'Antonio F. Outcome of Cesarean scar pregnancy managed expectantly: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51:169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 196] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 36. | Bignardi T, Alhamdan D, Condous G. Is ultrasound the new gold standard for the diagnosis of ectopic pregnancy? Semin Ultrasound CT MR. 2008;29:114-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 37. | Yang H, Wang R, Zhao L, Ye J, Li N, Kong L. Diagnosis and Analysis of Transabdominal and Intracavitary Ultrasound in Gynecological Acute Abdomen. Comput Math Methods Med. 2021;2021:9508838. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 38. | Flisser E, Grifo JA, Krey LC, Noyes N. Transabdominal ultrasound-assisted embryo transfer and pregnancy outcome. Fertil Steril. 2006;85:353-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 39. | Derbak A. Ectopic pregnancy in the ultrasound. Case reports. Retrospektive analysis. Ceska Gynekol. 2016;81:63-70. [PubMed] |
| 40. | Brady PC. New Evidence to Guide Ectopic Pregnancy Diagnosis and Management. Obstet Gynecol Surv. 2017;72:618-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 41. | Zahálková L, Kacerovský M. Cesarean scar ectopic pregnancy. Ceska Gynekol. 2016;81:414-419. [PubMed] |
| 42. | Ramanan RV, Gajaraj J. Ectopic pregnancy--the leash sign. A new sign on transvaginal Doppler ultrasound. Acta Radiol. 2006;47:529-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 43. | Shaw JL, Horne AW. The paracrinology of tubal ectopic pregnancy. Mol Cell Endocrinol. 2012;358:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 44. | Levine Y, Yahav L, Schwarzman P, Yohai D, Hershkovitz R, Weintraub AY. The correlation between endometrial thickness and the criteria for MTX treatment for ectopic pregnancy. J Obstet Gynaecol. 2021;41:1230-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 45. | Babayev E, Robins JC. Endometrial thickness as an independent risk factor for ectopic pregnancy in in vitro fertilization: should we change our counseling and practice? Fertil Steril. 2020;113:78-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 46. | Marossy A, Svorc P, Kron I, Gresová S. Hemorheology and circulation. Clin Hemorheol Microcirc. 2009;42:239-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 47. | Hale SA, Schonberg A, Badger GJ, Bernstein IM. Relationship between prepregnancy and early pregnancy uterine blood flow and resistance index. Reprod Sci. 2009;16:1091-1096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 48. | Fang T, Chen M, Yu W, Ma T, Su Z, Chan DYL, Zhao M, Zheng Q, Wang W. The predictive value of endometrial thickness in 3117 fresh IVF/ICSI cycles for ectopic pregnancy. J Gynecol Obstet Hum Reprod. 2021;50:102072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |