Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12610
Peer-review started: June 9, 2022
First decision: July 29, 2022
Revised: August 15, 2022
Accepted: November 7, 2022
Article in press: November 7, 2022
Published online: December 6, 2022
Processing time: 176 Days and 11.9 Hours
Ureteroscopy is well-established as a primary treatment modality for urolithiasis. Ureteral avulsion, particularly complete or full-length avulsion with a resultant long segment of the ureter left attached to the ureteroscope, is a rare but devastating complication of the procedure. Management of this complication is challenging. Moreover, general consensus regarding the optimal management is undetermined. We report our experience of managing a complete ureteral avulsion case via an extended Boari flap technique with long-term results.
A 41-year-old female patient subjected to complete ureteral avulsion caused by ureteroscopy was referred to our hospital. A modified, extended Boari flap technique was successfully performed to repair the full-length ureteral defect. Maximal mobilization of the bladder and affected kidney followed by psoas hitch and downward nephropexy maximized the probability of a tension-free anas
The extended Boari flap procedure is a feasible and preferred technique to manage complete ureteral avulsion, particularly in emergencies.
Core Tip: Management of complete ureteral avulsion caused by ureteroscopy is challenging. In the presented case, a modified, extended Boari flap technique was successfully performed to repair the full-length ureteral defect. During the 4-year study period, no complications except for a mild urinary frequency and a slightly lower maximum urinary flow rate were reported. The patient was satisfied with the surgical outcomes. This manuscript suggests the importance of the extended Boari flap procedure as a feasible and favorable treatment option to manage complete ureteral avulsion; moreover, ileal ureteral substitution or renal autotransplantation may be reserved as the second choice.
- Citation: Zhong MZ, Huang WN, Huang GX, Zhang EP, Gan L. Long-term results of extended Boari flap technique for management of complete ureteral avulsion: A case report. World J Clin Cases 2022; 10(34): 12610-12616
- URL: https://www.wjgnet.com/2307-8960/full/v10/i34/12610.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i34.12610
Ureteroscopy (URS) is well-established as a primary treatment modality for urolithiasis. Albeit not challenging in general, it may occasionally result in severe complications, of which complete or full-length ureteral avulsion may be the most disastrous. Treatment options for this complication typically include ileal ureteral substitution, renal autotransplantation, Boari flap technique, and even nephrectomy; however, there has been no consensus regarding the hierarchy of treatment selection[1,2]. Moreover, all of these treatments are challenging. We present a case of ureteral avulsion as a complication of URS, managed via an extended Boari flap technique, and we describe the long-term results.
A 41-year-old female patient was referred to our hospital owing to ureteral avulsion caused by URS.
The patient, with left proximal ureteral calculus and associated mild hydronephrosis, underwent a left 8/9.8-Fr semirigid URS and laser lithotripsy at an outside clinic. The stone was completely fragmented. On withdrawal of the scope, the operator felt the impacted scope in the ureter, and ureteral avulsion occurred. The patient reportedly had an avulsion at the upper ureter and was finally transferred to our hospital for definitive management after refusals by several hospitals.
The patient was a hepatitis B carrier and had a history of multiple uterine leiomyomas; however, she did not have any surgical history.
The patient’s personal and family history was unremarkable.
The patient presented with body weakness but was clinically stable, with a blood pressure of 129/83 mmHg and heart rate of 93 bpm at admission. She was 156 cm tall and 53 kg in weight, with a body mass index of 22 kg/m2.
Laboratory test results revealed anemia, with a hemoglobin level of 79 g/L. The results for the other tested parameters were normal or with little clinical significance.
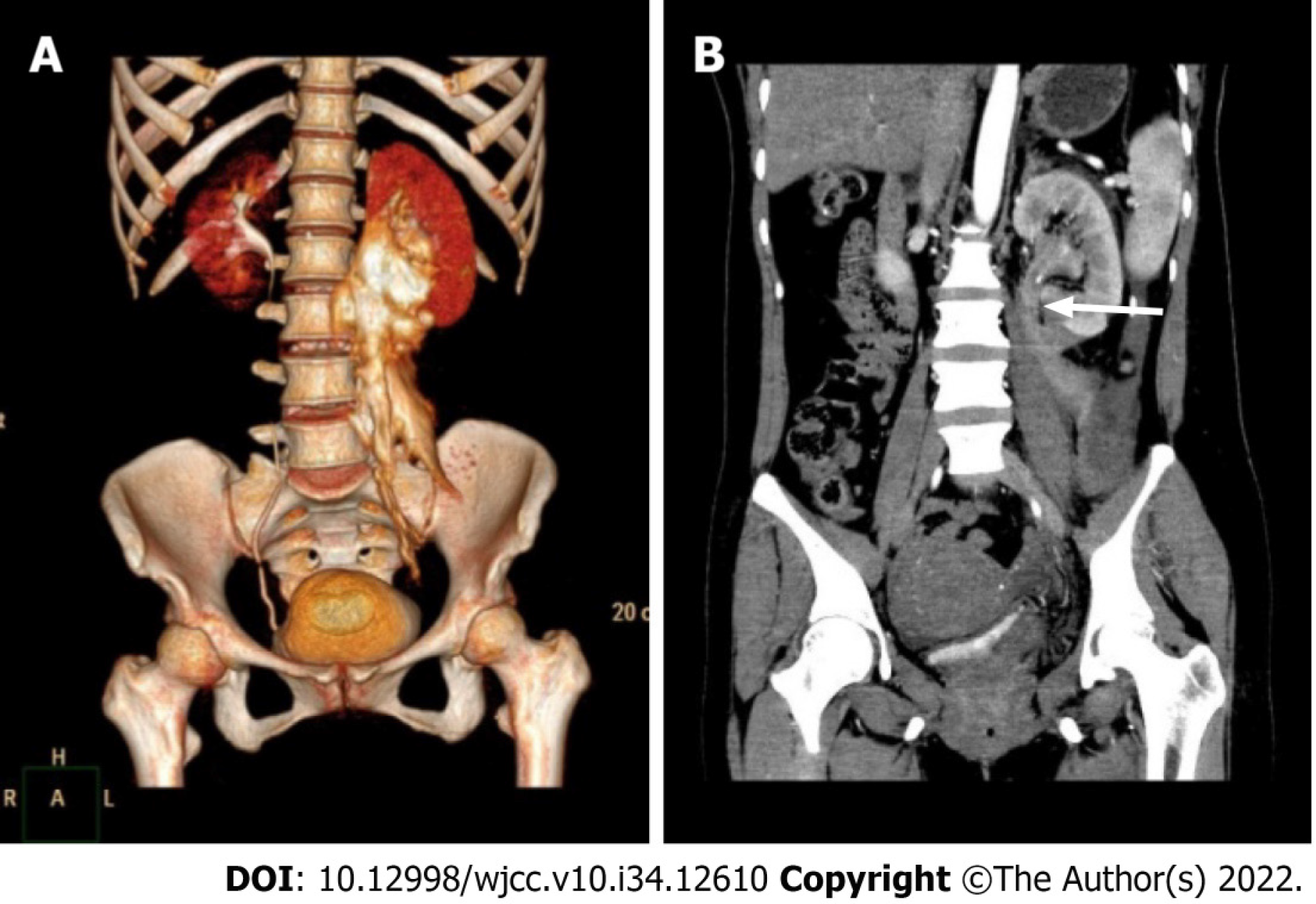
Computed tomography urography (CTU) was performed, confirming complete avulsion at the proximal ureter just below the ureteropelvic junction (UPJ) (Figure 1).
Management options were discussed with the patient and her husband, including ureteral reconstruction using a Boari flap, ileal ureteral substitution, renal autotransplantation, and nephrectomy as the last resort, and the patient was informed that the final decision had to be made in the operating room. The patient was brought to the operating room and placed in a supine position. A midline incision was performed, followed by mobilization of the descending colon and exposure of the retroperitoneum. The perirenal hematoma was cleared, and a ureteral stump was identified just below the UPJ above the lower pole level. Additionally, the distal ureter was “missing” at the entire left retroperitoneum, and full-length ureteral avulsion was confirmed.
The final diagnosis was left-sided complete ureteral avulsion injury caused by URS.
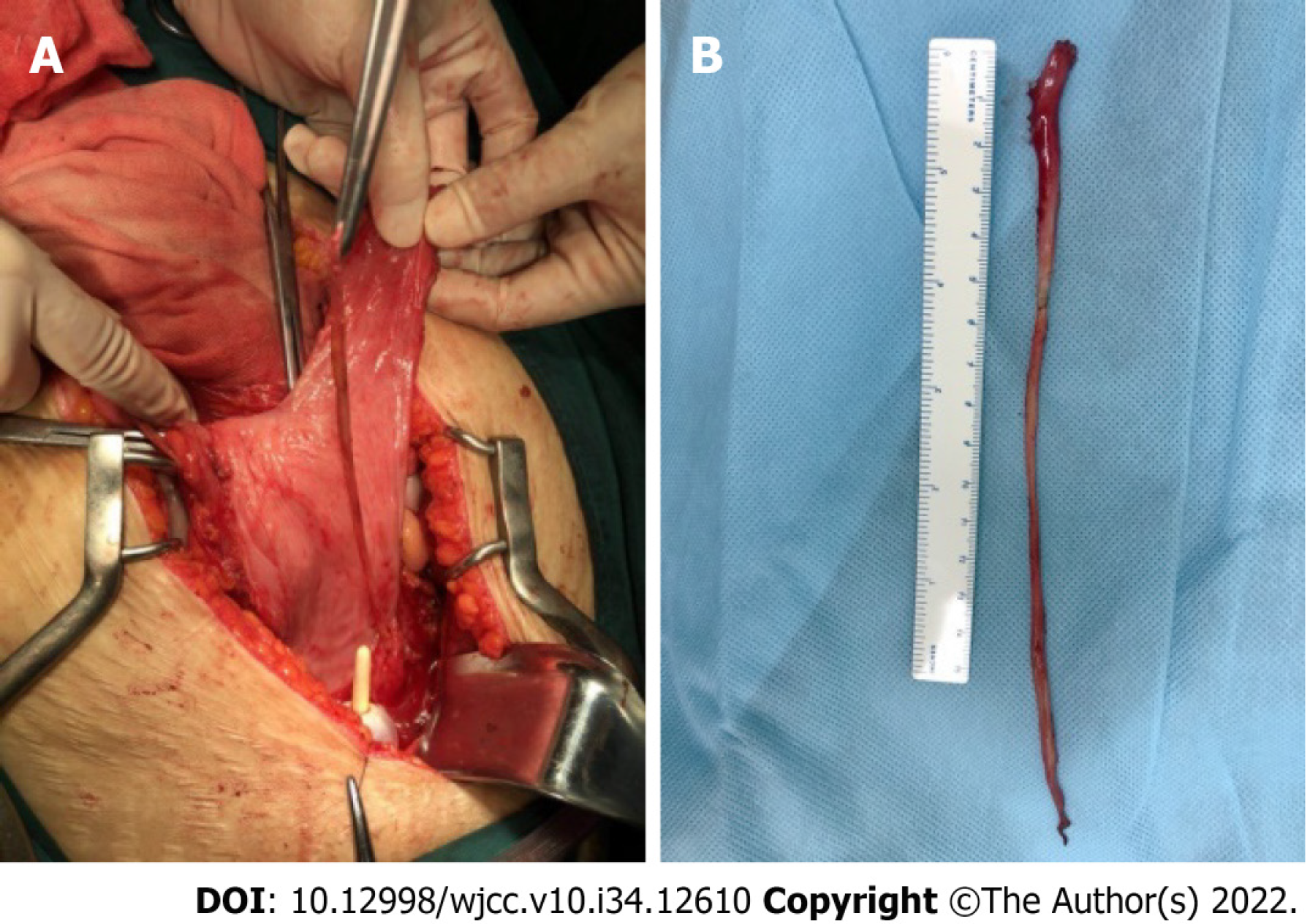
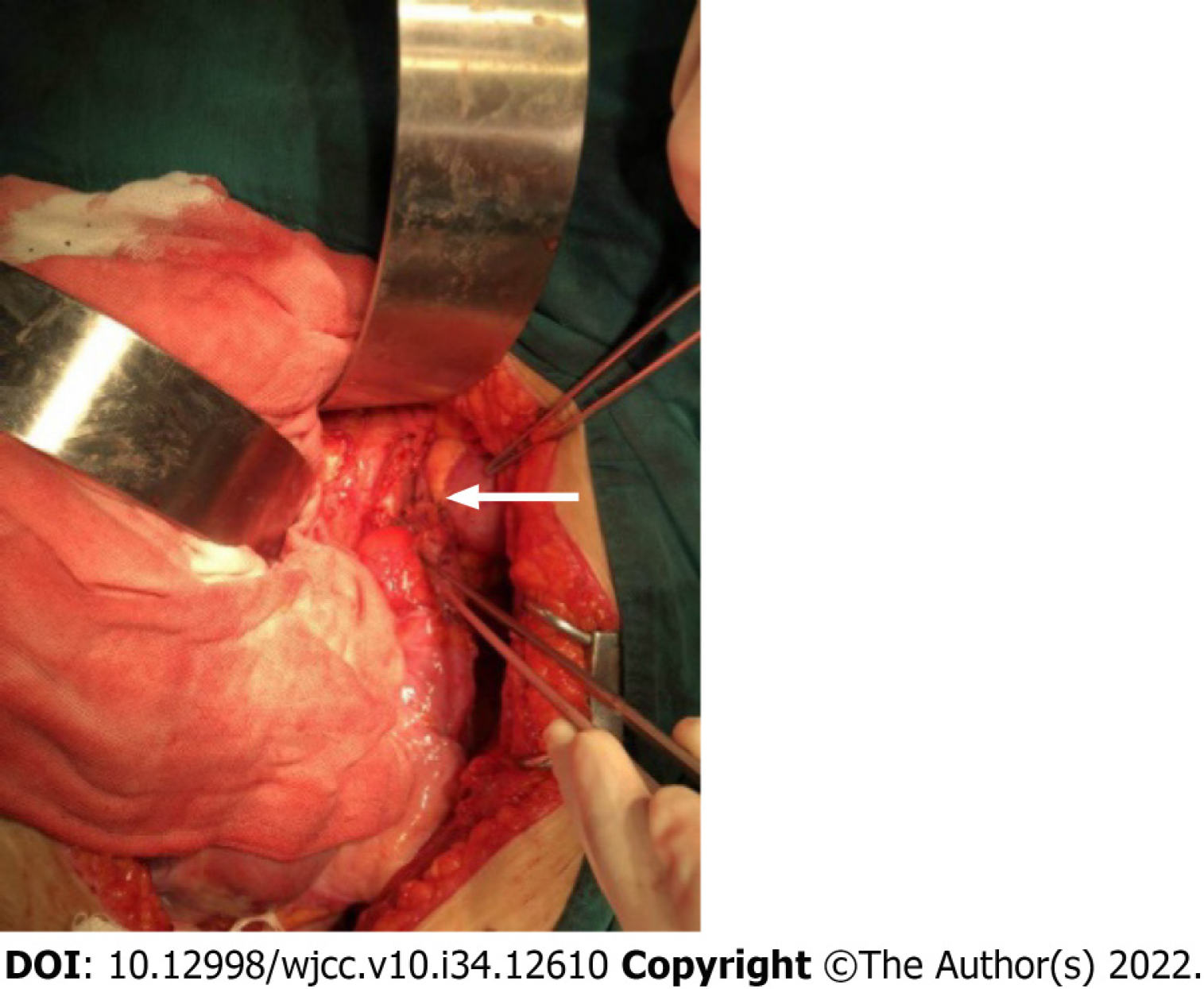
We first attempted using a Boari flap. The bladder was thoroughly mobilized to the endopelvic fascia caudally. Bilateral medial umbilical ligaments were transected at the initial level, with superior vesical vessels of both sides preserved. Traction was placed on the dome of the highly compliant bladder toward the ureteral stump, with the assistant placing a countertraction on the left kidney caudally. Then, the gap was distinctly shorter than the length between the bladder neck and dome. Furthermore, the decision was made to perform a Boari flap technique for ureteral reconstruction. The left kidney was thoroughly mobilized, and the bladder attachments, such as the peritoneum near the bladder pedicles, which restrained bladder traction, were further dissected to achieve the smallest gap possible. The assistant retracted the bladder toward the ureteral stump with his hands turning the bladder into a long sac-like pouch. Hence, a trapezoidal flap with the apex starting from the bladder neck was made obliquely on the anterior wall of the bladder using low-power monopolar cautery. Surprisingly, a long isolated devitalized ureter was noticed within the bladder, which was thought to be placed by the operator after removing the ‘‘scabbard’’ of the ureter on the ureteroscope in vitro (Figure 2). Excessive cautery was avoided to minimize blood supply damage. The apex and base measured 2.5 cm and 5 cm, respectively. Subsequently, the flap was fixed to the psoas muscle above the common iliac artery, avoiding the genitofemoral nerve by two interrupted sutures using 2-0 PDS sutures. The lower pole of the left kidney was also fixed to the psoas muscle caudally. These procedures ensured a tension-free anastomosis despite an enlarged uterus caused by multiple uterine leiomyomas. The remnant of the proximal ureter was trimmed and spatulated dorsally and then anastomosed end-to-end to the bladder flap starting dorsally using interrupted 3-0 Monocryl sutures. The bladder flap was then tubularized over a 6F Double-J stent with a running 3-0 Monocryl suture closing the mucosa layer and a second layer of 2-0 Monocryl closing the detrusor muscle (Figure 3). A watertight reconstruction was confirmed. Intraoperative blood loss was limited; however, two units of red blood cells were transfused owing to preexistent anemia.
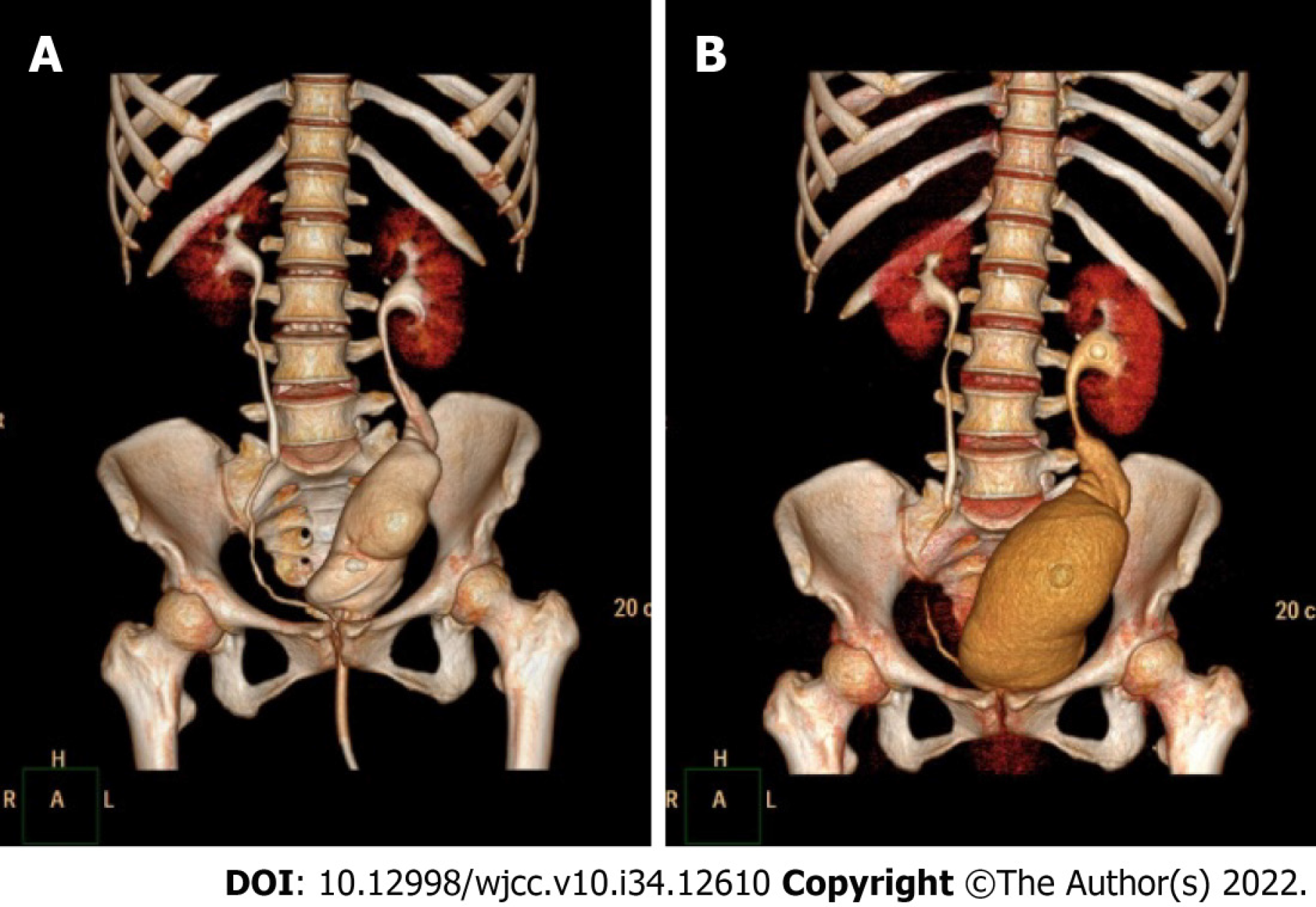
Postoperative recovery was uneventful. The Foley catheter was left in place for 14 d, at which time a CTU demonstrated a drumstick-like bladder without leakage. Cystoscopy and stent removal were performed after 2 mo; subsequently, a CTU demonstrated mild hydronephrosis in the left kidney as the baseline (Figure 4). Ultrasonography confirmed no hydronephrosis in both kidneys 1 mo later. Since then, the patient was followed up every 3–6 mo by ultrasonography, urine test, renal function test, and occasionally, urodynamics.
The patient complained of frequent urination postoperatively. She needed to urinate every 1–2 h in the daytime and 3–4 times at night in the first 3 mo after stent removal. Frequency gradually improved to 2–3 times per night in the following 6 mo. The urodynamic analysis results demonstrated normal bladder function except for a slightly lower maximum urinary flow rate at 5 and 13 mo with bladder volume tests of approximately 200 mL. After 18 mo, the patient reported approximately the same urination habits as before, with once or twice nighttime urination and bladder volume ranging from 200 to 250 mL. She did not report any urinary tract infection or lumbar pain during urination, indicating subclinical or no reflux. Neither hydronephrosis on both sides nor renal function damage was documented during the 48-mo follow-up. The patient was satisfied with the surgical outcomes.
Ureteral avulsion is rare; however, it is a devastating complication that may occur during URS. Complete ureteral avulsion, defined as a two-point ureteral avulsion with one point at the intramural ureter and the other at the proximal ureter up to the UPJ, is nearly a catastrophe that may induce a nephrectomy[3,4]. Complete ureteral avulsion often occurs during a semirigid URS in these consecutive processes: (1) The operator finds it difficult to advance the ureteroscope and feels restricted in the ureter owing to a relatively small ureteric lumen size; (2) Excessive force on the ureteroscope, of which the outer caliber is gradually larger towards the base, makes it wedged into the ureter until tightly impacted; (3) Further force results in a complete avulsion of the intramural ureter from the bladder wall; and (4) On withdrawal of the ureteroscope, because the ureter is already tightly impacted and because the operator is usually startled at that time, a second avulsion occurs at the UPJ or site where the stone is impacted, as it has been weakened by mucosa inflammation or the microtrauma caused by lithotripsy[5].
Considering the same inner lining with the ureter and relatively small anatomical changes to the patient, a Boari flap for ureteral reconstruction is an ideal treatment option if it is technically feasible with acceptable surgical complications. Owing to the complexity of the Boari flap technique, particularly for a full-length avulsion case in an emergency setting, many operators may opt for an ileal ureteral substitution, as it has no length limit when harvested to bridge a ureteral defect and achieve a tension-free anastomosis[1,6-9]. However, it results in extra bowel-related complications, such as ileus, intestinal leakage, mucus production, recurrent pyelonephritis, hyperchloremic metabolic acidosis, and impaired renal function, thus making it an unfavorable option for many operators[6-10]. Alternatively, renal autotransplantation can eliminate even a full-length ureteral defect without those bowel-related complications[11-13]. However, it requires an experienced renal transplantation team which may be unavailable for most hospitals, especially in an emergency setting. Furthermore, even in the expert’s hands, the risk of graft loss is reportedly up to 14.4%[11,14,15], not to mention the sense of insecurity felt by relocating the kidney from the retroperitoneum to the palpable iliac fossa.
The Boari flap technique is typically applied in the repair of a mid-ureteral defect. Previous reports have indicated the application of this technique in upper and even full-length ureteral defects[10,16,17]. However, owing to the complexity and challenge of the technique itself, most of the available literature was limited to small case series or case reports without long-term outcomes. The detailed techniques and complications with long-term follow-up data must be further elucidated. In the presented case, a modified, extended Boari flap technique was performed to repair the full-length ureteral defect with satisfactory long-term results for the patient. Several principles and techniques have been applied to achieve this success. First, maximal mobilization of the entire bladder and ipsilateral kidney is fundamental, guaranteeing the longest bladder flap and the most effective downward nephropexy, and thereafter, a tension-free anastomosis. We also presented our techniques for constructing an extended Boari flap, which is less complicated than L-shaped or S-shaped flaps[10,17]. Second, meticulous blood supply preservation with intact bilateral superior vesical arteries and minimal use of electrocautery also contributed to the success.
The main limitations of our study are that it is a case report and that right ureteral avulsion may confront different conditions, as it is associated with a much shorter renal vein than the left. However, the present case involved a concomitant enlarged uterus which increased the actual distance between the bladder and the ureter remnant. In addition, contemporary bladder flap reconstruction studies did not show any different outcomes regarding the surgical side[10,17]. Therefore, our presented techniques might also be applied successfully in right-sided cases. In any case, managing complete ureteral avulsion is challenging. Prevention of ureteral avulsion is always the most rewarding measure. One should never forcefully manipulate a ureteroscope during the operation, and a smaller caliber scope or a second-stage surgery is always a safer choice when confronting difficulties during ureteroscope advancement.
The use of the Boari bladder flap is a feasible and preferred technique to manage complete ureteral avulsion. Maximal mobilization of the bladder and affected kidney followed by psoas hitch and downward nephropexy would maximize the success of a tension-free anastomosis, and thereby, minimize the need for ileal ureteral substitution or renal autotransplantation. However, more cases of ureteral avulsion on both sides with substantial experience are required to fully elucidate its limitations and make modifications accordingly.
| 1. | Yuan C, Li Z, Wang J, Zhang P, Meng C, Li D, Gao J, Guan H, Zhu W, Lu B, Zhang Z, Feng N, Yang K, Li X, Zhou L. Ileal ureteral replacement for the management of ureteral avulsion during ureteroscopic lithotripsy: a case series. BMC Surg. 2022;22:262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Ragonese M, Foschi N, Pinto F, Di Gianfrancesco L, Bassi P, Racioppi M. Immediate ileal ureter replacement for ureteral avulsion during ureterescopy. IJU Case Rep. 2020;3:241-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Kuddah Y, Noegroho BS, Abriansyah AT, Mustafa A. Inverted mucosa and avulsion ureteral injury in ureteroscopic procedure: A very rare complication of a common procedure in urology. Urol Case Rep. 2021;37:101605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Ordon M, Schuler TD, Honey RJ. Ureteral avulsion during contemporary ureteroscopic stone management: "the scabbard avulsion". J Endourol. 2011;25:1259-1262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Gaizauskas A, Markevicius M, Gaizauskas S, Zelvys A. Possible complications of ureteroscopy in modern endourological era: two-point or "scabbard" avulsion. Case Rep Urol. 2014;2014:308093. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Chung BI, Hamawy KJ, Zinman LN, Libertino JA. The use of bowel for ureteral replacement for complex ureteral reconstruction: long-term results. J Urol. 2006;175:179-83; discussion 183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 93] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Kocot A, Kalogirou C, Vergho D, Riedmiller H. Long-term results of ileal ureteric replacement: a 25-year single-centre experience. BJU Int. 2017;120:273-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | Zhong W, Hong P, Ding G, Yang K, Li X, Bao J, Bao G, Cui L, Men C, Li Z, Zhang P, Chu N, Zhou L. Technical considerations and outcomes for ileal ureter replacement: a retrospective study in China. BMC Surg. 2019;19:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Sevinc C, Balaban M, Ozkaptan O, Yucetas U, Karadeniz T. The management of total avulsion of the ureter from both ends: Our experience and literature review. Arch Ital Urol Androl. 2016;88:97-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Mauck RJ, Hudak SJ, Terlecki RP, Morey AF. Central role of Boari bladder flap and downward nephropexy in upper ureteral reconstruction. J Urol. 2011;186:1345-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Meng MV, Freise CE, Stoller ML. Expanded experience with laparoscopic nephrectomy and autotransplantation for severe ureteral injury. J Urol. 2003;169:1363-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Alizadeh M, Valizadeh R, Rahimi MM. Immediate successful renal autotransplantation after proximal ureteral avulsion fallowing ureteroscopy: a case report. J Surg Case Rep. 2017;2017:rjx028. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Shekarriz B, Lu H, Duh Q, Freise CE, Stoller ML. Laparoscopic nephrectomy and autotransplantation for severe iatrogenic ureteral injuries. Urology. 2001;58:540-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Vrakas G, Sullivan M. Current Review of Renal Autotransplantation in the UK. Curr Urol Rep. 2020;21:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Yakupoglu YK, Aki FT, Kordan Y, Ozden E, Tonyali S, Bostanci Y, Vuruskan H, Bilen CY, Sarikaya S. Renal Autotransplantation at Three Academic Institutions in Turkey. Urol Int. 2016;97:466-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Grzegółkowski P, Lemiński A, Słojewski M. Extended Boari-flap technique as a reconstruction method of total ureteric avulsion. Cent European J Urol. 2017;70:188-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 17. | Li Y, Li C, Yang S, Song C, Liao W, Xiong Y. Reconstructing full-length ureteral defects using a spiral bladder muscle flap with vascular pedicles. Urology. 2014;83:1199-1204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (2)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Kaewput W, Thailand; Leowattana W, Thailand; Markic D, Croatia; Shrestha AB, Egypt; Vyshka G, Albania S-Editor: Xing YX L-Editor: Wang TQ P-Editor: Xing YX